Modern cardiac resynchronization devices (CRT) are pacemakers that are implanted in the subclavian region and are connected to three electrodes passed through the subclavian vein into the right atrium, right and left ventricles. Modern devices have many programmable parameters (for example, the value of atrioventricular and intraventricular delay), which make it possible to provide the optimal mode of biventricular (two-ventricular) pacing based on a specific clinical situation.
The biventricular pacemaker entered testing by the American Licensing Authority (FDA) in 2001 and was approved for clinical use in the Russian Federation in 2003.
The first results of treatment of patients with CHF were successful.
1990–1992 Margarete used dual-chamber (atrioventricular) pacing with shortened atrioventricular delay to treat end-stage heart failure caused by dilated cardiomyopathy.
In 1994, two groups of researchers - S. Cazeau and P. Bakker - for the first time undertook a three-chamber (on the atrium and both ventricles) pacemaker in patients with a combination of severe HF and intraventricular block.
In 1994, Y. Bai published data on left ventricular pacing in two patients with impaired AV conduction through electrodes inserted into the coronary sinus. In one case, the electrode could not be passed into the right ventricle due to a previously implanted mechanical tricuspid valve, and in the other, due to pronounced diaphragmatic stimulation with adequate positioning of the electrode in the right ventricle.
In 1998, J. Daubert proposed inserting an electrode into the wall of the left ventricle through a vein from the coronary sinus.
Introduction
This information has been specially prepared for you, so that you, your family and friends can find answers to your questions on these pages.
More than two million people, thanks to a pacemaker, live a full life - study, work, travel, and play sports. Most patients with pacemakers remember it only when they come for a medical examination, and in everyday life their activity in the family, on vacation and at work is no different from the people around them. First of all, the main purpose of pacemaker implantation is to eliminate life-threatening arrhythmias and improve your quality of life. All subsequent restrictions and your regimen will depend on your physical condition, manifestations of the disease and the recommendations you receive from your doctor.
Pacing and why it is necessary for your heart
The most common condition that requires a pacemaker is called bradycardia, which means the heart rate is too low for the body's needs. Possible symptoms of bradycardia are dizziness, extreme fatigue, shortness of breath, and fainting. Bradycardia is usually caused by one of the following heart diseases (or complications of the underlying disease) or a combination of them:
- Sick sinus syndrome (SSNS) – the sinus node sends impulses infrequently, at too long or irregular intervals.
- Heart block is a disruption of the normal passage of electrical impulses from the heart. Heart block can occur at various levels of the conduction system, but usually this term refers to conduction block at the level of the atrioventricular (atrioventricular) node. In this case, the impulses produced by the sinus node do not reach the ventricles. The ventricles contract very rarely, in their own rhythm, asynchronously with the atria.
Your heart rate usually beats between 60 and 80 beats per minute. A reading below 60 beats per minute is called bradycardia. For many people in good physical shape (or such a rhythm occurs during rest and sleep), such a rhythm is the norm. A distinctive feature of such bradycardia is that with increasing physical activity, the heart rate begins to accelerate, covering the body’s needs with its frequency.
We talk about bradycardia as a disease when the rhythm has a very low frequency, does not respond by increasing frequency to physical activity, or large pauses occur in the rhythmic contraction, which can reach or even exceed more than 2 seconds.
When bradycardia is confirmed diagnostically and such a rhythm is the only manifestation, then such a rhythm is effectively corrected by a pacemaker.
Electrocardiac pacemaker (Pacemaker)
Modern pacemakers are miniature computers that monitor your heart's own rhythm. Stimulants can come in a variety of shapes and are generally small and light (approximate weight 20 to 50 grams).
The pacemaker consists of a titanium housing that contains a microcircuit and a battery.
The main function of a pacemaker is to monitor the heart rhythm and stimulate if a rare or irregular rhythm occurs with skips in contractions. If the heart beats with the correct frequency and rhythm, the pacemaker in this case does not work, but constantly monitors its own heart rhythm.
Each type of pacemaker is designed for a specific type of heart rhythm disorder. The indications for implantation are determined by your doctor based on the data obtained from your examination.
Pacemakers can be either single-chamber or multi-chamber (two or three stimulating chambers). Each stimulation chamber is designed to stimulate one part of the heart. Dual-chamber devices stimulate the atrium and right ventricle, while three-chamber cardiac resynchronization devices (CRT) stimulate the right atrium, right and left ventricles.
Cardiac resynchronization stimulators are used to treat severe forms of heart failure, eliminating uncoordinated contractions of the heart chambers (dyssynchrony).
Pacemakers may be equipped with sensors. Such stimulators are called frequency-adaptive; they use a special sensor that detects changes in the body (such as movement, nervous system activity, respiratory rate, body temperature). Frequency-adaptive stimulators (indicated by a special letter R - indicates frequency adaptation) are used for rigid, i.e. Since the heart rate does not change depending on physical activity and emotional state, then in this case the increase in rhythm due to physical activity will occur due to the pacemaker.
The pacemaker consists of:
- Battery (accumulator) The battery supplies electrical energy to the pacemaker and is designed for many years of uninterrupted operation (up to 10 years). When the pacemaker battery capacity is depleted, the pacemaker is replaced with another one.
- Microcircuit The microcircuit is like a small computer inside a pacemaker. The microcircuit transforms battery energy into electrical impulses to stimulate the heart. The microcircuit controls the duration and power of electrical energy expended for the pulse.
- Connector block A transparent plastic block is located at the top of the pacemaker. The connector block is used to connect the electrodes and the pacemaker.
Electrodes
The pacemaker is connected to the heart through veins using special electrodes. The electrodes are attached to the cavities of the heart and play a connecting role between the activity of the heart and the stimulator.
The electrode is a special coiled conductor that is flexible enough to withstand the torsion and bending caused by body movements and heart contractions. The electrode transmits the electrical impulse generated by the pacemaker to the heart and carries back information about the activity of the heart.
The electrode contacts the heart through a metal head at the end of the wire. With its help, the stimulator “monitors” the electrical activity of the heart and sends electrical impulses (stimulates) only when the heart requires them.
Programmer
The programmer is a special computer that is used to control and change the settings of the pacemaker. The programmer is located in medical institutions where pacemakers are implanted or where there is a consulting room for working with patients with pacemakers.
The doctor analyzes all the functions of the pacemaker and, if necessary, can change the settings necessary for the pacemaker to function correctly. In addition to technical information about the pacemaker operation, the doctor can view all recorded cardiac events in chronological order. Such events include atrial and ventricular cardiac rhythm disturbances (atrial flutter and fibrillation, supraventricular and ventricular tachycardia, ventricular fibrillation).
Single-chamber pacemaker
A single-chamber stimulator uses a single endocardial lead placed in either the right atrium or right ventricle to stimulate the cardiac chamber (atrium or ventricle).
Isolated atrial stimulation is used in cases where the generation of sinus rhythm (SSRS) is impaired while the atrioventricular junction (atrioventricular node) is functioning intact. In this case, cardiac pacing completely or partially replaces the function of sinus rhythm.
Ventricular stimulation is used if the patient has a permanent form of atrial fibrillation or transient atrioventricular blockade of the sinus rhythm into the ventricles occurs. In rare cases, it can be implanted with complete atrioventricular block.
Dual chamber pacemaker
A dual-chamber pacemaker uses two endocardial leads to pace the right atrium and right ventricle. The electrodes are placed in the appropriate areas, thereby stimulating two chambers of the heart at once.
Dual-chamber stimulators are used to synchronize the atria and ventricles in cases of impaired atrioventricular conduction (AV junction dysfunction), which makes the heart rhythm closest to natural.
Both single-chamber and dual-chamber pacemakers can be equipped with a frequency adaptation function. The frequency adaptation function is used to increase the heart rate if one’s own, natural rhythm cannot respond by increasing the frequency to physical activity or to the emotional state of a person.
Frequency adaptation is marked with the Latin letter R. In single-chamber stimulators the designation SR is used, in dual-chamber stimulators - DR.
What types of ICDs are there?
Single chamber ICD
A single-chamber ICD is used in cases of atrial fibrillation or when the patient does not have transient conduction blocks and the heart rate fully corresponds to the needs of the body.
The stimulator has one ventricular electrode, which is placed in the cavity of the right ventricle. When VT or VF occurs, the pacemaker delivers a defibrillator shock.
The stimulator has an algorithm for ultra-frequent and programmed stimulation to prevent an attack of VT with “painless stimulation”. In addition to the high efficiency of the painless stimulation algorithm in stopping VT, this mode practically does not consume the pacemaker battery charge. In this case, the defibrillator does not discharge.
If the patient has bradycardia, the ICD works like a regular pacemaker.
Dual chamber ICD
A dual-chamber ICD contains two pacing chambers designed to stimulate the right atrium and the right ventricle. Electrodes are placed in the appropriate areas, thereby tracking the heart rhythm in the atria and ventricles.
During AV blockade, the ICD paces the atrial and ventricular rhythms. Antitachycardia therapy is carried out at all levels, including the ability to stop a sudden increase in atrial rhythm during atrial flutter, atrial tachycardia, and supraventricular tachycardia with antitachycardia pacing (ATS). ATC is widely used to provide pain-free therapy for VT, thereby preserving ICD battery charge.
Three-chamber ICD (CRT/ICD)
Cardioverter-defibrillator with cardiac resynchronization therapy. CRT/ICD is used to treat heart failure (HF) by synchronizing the ventricles of the heart into a single heartbeat cycle.
CRT/ICD can provide the full range of antiarrhythmic therapy, including defibrillator shock therapy to restore heart rhythm.
Pacemaker implantation procedure
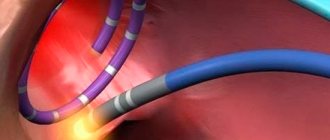
Pacemaker implantation is a surgical procedure in which a small incision is made in the right (if you are left-handed) or left (if you are right-handed) subclavian region. Depending on which pacemaker you are implanted with, one, two or three electrodes will be inserted through a vein and placed inside the heart under X-ray guidance.
As with most surgical procedures, a short course of prophylactic therapy with antibiotics and anti-inflammatory drugs will be prescribed after pacemaker implantation.
Before surgery, your doctor will limit or stop certain medications you take, and the choice of anesthesia will be determined by your anesthesiologist before surgery. The operation of implanting (sewing in) a stimulator seems simple, since it causes little damage to tissue, and is carried out in an operating room equipped with an X-ray machine. A vein is punctured (pierced) under the collarbone, a special plastic tube (introducer) is inserted into it, through which endocardial electrodes are inserted into the superior vena cava (transvenously). Under X-ray control, the electrodes are directed into the right atrium and right ventricle, where they are fixed.
The most difficult procedure is to install and secure the tip of the electrode in the atrium and ventricle so as to obtain good contact. Usually the surgeon makes several tests, all the time measuring the threshold of excitability, i.e. the smallest impulse value (in volts) to which the heart responds with a contraction, visible on the ECG. The challenge is to find the most sensitive spot and at the same time get a good ECG graphic recorded from the electrodes being installed. After fixing the electrodes, they are connected to a stimulator, which is placed in a formed bed under the fascia of the fatty tissue or under the muscles of the chest.
Of course, the operation requires strict sterility and careful control of bleeding to avoid accumulation of blood under the skin and suppuration. The stimulator itself and electrodes are supplied sterile. In total, all manipulations take from one to two hours.
The described method is most often used for pacemaker implantation in surgical practice. There are other implantation methods that are used in connection with certain characteristics or concomitant diseases of the cardiovascular system.
If a patient is scheduled to undergo open heart surgery due to an underlying medical condition and there is an indication for pacemaker implantation, then, as a rule, the leads will be placed epicardially (the outer lining of the heart) and the pacemaker will be placed in the rectus abdominis muscle. This placement of electrodes is optimal because the electrodes do not come into contact with human blood and are not located in the heart cavity.
How to install an automatic defibrillator, replace it - stages of the operation
Before carrying out the procedure in question, the patient should undergo examination:
- Take a blood test.
- Examine the condition of the chest cavity using an x-ray method.
- Get an ECG and EchoCG.
In order to exclude/confirm coronary heart disease, catheterization or stress testing is performed.
You should tell your doctor if you are taking any medications.
A few days before surgery, you need to stop taking medications that thin your blood.
8-10 hours before the manipulation, water and food should not be taken.
The procedure for the initial installation of an automatic cardioverter-defibrillator can last from 1 to 3 hours .
ICD implantation algorithm:
- Intravenous administration of sedatives to relax the patient before surgery.
- Treating the work area with antiseptic agents.
- The use of local anesthetics to numb the manipulation area.
- Piercing the subclavian vein for the purpose of introducing endocardial electrodes into it, which are initially placed in a flexible plastic tube. These electrodes are advanced under X-ray control to the right ventricle and right atrium.
- Fixation of the electrode tip. This stage is the most difficult part of the operation. The surgeon should conduct several tests to find the best contact.
- Connecting electrodes to the stimulator. The ICD itself is placed in a flap pocket, which is made in the area of the second incision.
- Stitching. Absorbable threads are often used.
- Applying a pressure bandage to prevent blood leakage. It is removed in a day.
To prevent infection of the work area after surgery, the patient is prescribed a short course of antibiotic therapy, as well as anti-inflammatory drugs.
X-ray after installation of an automatic cardioverter-defibrillator
The operation to replace an ICD takes less time, and the recovery period is shorter than with the initial implantation of the specified device.
The doctor periodically checks the wear level of the battery, as well as the degree of serviceability of the cardiac defibrillator using the programmer. In this regard, a medical facility needs to be visited several times a year.
If the battery capacity is low, the patient is informed several months in advance and a procedure is planned to replace the ICD. On average, a battery is useful for 5-7 years.
During the operation, the surgeon inserts a new cardioverter-defibrillator into the old pocket. In extremely rare cases, the electrodes are also changed. But often old conductors are connected to a new stimulator after they have been thoroughly tested.
What is CRT/ICD?
There are a large number of pacemakers (pacers) that are designed to treat cardiac arrhythmias and conduction disorders. Depending on the complexity of the arrhythmias, your doctor will suggest one type of pacemaker or another. Its size will depend on the specifics of the stimulator and its functions and battery capacity of the pacemaker. The first stimulators developed were placed on a cart and pacing was carried out through wires to the heart. Over the past three decades of technological progress, complex pacemakers with a large battery capacity and dimensions no larger than a matchbox have been introduced into clinical practice.
In the late 90s, implantable cardioverter-defibrillators (ICD) and cardiac resynchronization devices (CRT) were developed and put into practice. The first pacemakers were presented separately and had a large weight and size. Cases have been described where it was necessary to implant two CRT and ICD stimulators at once in one person.
Implantable cardioverter-defibrillator with cardiac resynchronization therapy ICD/CRT is a combined device intended for the treatment of heart failure and suppression (relief) of ventricular tachycardia or ventricular fibrillation (life-threatening arrhythmias).
ICD (ICD) implantable cardioverter-defibrillator.
Used to detect and relieve most cardiac arrhythmias. Its main function is to restore the heart rhythm by shock discharge (defibrillation) when ventricular tachycardia (VT) or ventricular fibrillation occurs. In addition to the possibility of a shock discharge, the function of painless suppression of VT through ultra-frequent and programmed stimulation is provided.
After implantation, the pacemaker operates automatically.
The stimulator is no larger than the size of a pager or the palm of a small child.
How does an ICD work?
Therapy of tachyarrhythmias
An ICD pacemaker constantly “monitors” the electrical activity of your heart. It can always tell what your rhythm is, including performing the function of a “Holter monitor” by recording fragments of the heart rhythm into memory, helping the doctor learn more about the patient’s rhythm than a regular electrocardiogram. If a tachyarrhythmia occurs in the heart, the stimulator algorithms will provide electrical therapy automatically. The type of treatment and program of stimulator functions depends on the settings that your doctor chooses.
After implanting the ICD, your doctor will tell you what therapy he has prescribed.
Ventricular fibrillation is a very life-threatening event. The ICD is specifically designed to restore sinus rhythm with a shock shock. This is called defibrillation. Your ICD has pain-free rhythm restoration (anti-tachycardia function) and anti-bradycardia function to treat all types of bradyarrhythmias.
Defibrillation
If the ICD detects VF, it delivers a high-energy shock. This is called defibrillation. During defibrillation, a shock is delivered directly to the heart. Restoring sinus rhythm requires much less energy (1/10th) compared to external defibrillation, which is performed by doctors in emergency situations.
The total time from the onset of a VF attack to the defibrillator shock is about 10 seconds. During this time, energy accumulates in the ICD, which is necessary to produce a high discharge during defibrillation.
Cardioversion is the restoration of heart rhythm by a defibrillator discharge (shock energy discharge). There are two types of electrical cardioversion: external, by applying special plates to the chest, and internal, through an electrode in the right ventricle with an electric current discharge.
Antitachycardia pacing (ATP)
Antitachycardia pacing has been widely used to suppress most cardiac tachyarrhythmias, including VT. The meaning of ATS is to determine heart rhythm disturbances and suppress an attack through ultra-frequent or programmed stimulation.
ATS is widely used to provide pain-free therapy for VT, thereby preserving battery charge. If the ATS is ineffective or in VF, it produces a defibrillator discharge.
If ventricular tachycardia occurs, your ICD will check for the abnormal rhythm and provide the necessary therapy to restore sinus rhythm. The type of antitachycardia function program is determined by your doctor when programming the ICD. If an antitachycardia function is established (painless relief of tachyarrhythmias), then during an attack of VT the stimulator will restore the correct heart rhythm with frequent electrical stimulation with a certain sequence. This stimulation is called antitachycardia therapy; when it occurs, the patient does not feel it.
Antibradycardia pacing
If your heart rhythm becomes very slow or skips (pauses) occur, the ICD can work like a simple pacemaker used for bradycardia. The atrial and ventricular pacing chambers synchronize the upstream and downstream rhythms, thereby creating the optimal pacing pattern.
Alarm system
The ICD may have a built-in function to alert the patient to the need to see a doctor for evaluation. The ICD can be programmed to sound 30-second beeps when conditions require urgent medical attention. The two different beep tones correspond to different reasons. The signals are repeated every 24 hours until the doctor reads the information using the programmer. If the ICD beeps, consult a doctor immediately!
Why does my doctor recommend CRT/ICD implantation?
The doctor’s recommendations are based on the results of studies confirming the diagnosis and the presence of a threat to your life.
In many patients, severe systolic heart failure is accompanied by significant intra- or interventricular conduction delays, which lead to disruption of the synchrony of contraction, which is accompanied by a decrease in the efficiency of the pumping function of the ventricles.
1. Due to progressive symptoms of heart failure, which are accompanied by shortness of breath, swelling of the legs, weakness:
- Patients in whom the ventricles of the heart do not contract together (ventricular dyssynchrony).
- Patients with symptoms refractory to drug therapy - without improvement in quality of life (NYHA functional class III or IV).
- Patients with ineffective heart function – low ejection fraction (35% and below), increased volume and size of the heart.
Pacemakers with CRT/ICD function are able to restore synchronous contraction of the heart and, as a result, eliminate symptoms associated with heart failure. Studies have shown that most patients after CRT/ICD implantation experience improved well-being and quality of life, and increased exercise tolerance.
2. Your heart may be susceptible to very life-threatening palpitations. Heart rhythm disturbances can occur in almost every person, but are more often caused by coronary heart disease, myocardial infarction, heart defects, cardiomyopathies and inflammatory diseases.
Ventricular tachycardia is a life-threatening rhythm disorder. With excessively frequent contractions, the ventricles of the heart do not have time to fill with enough blood. As a result, insufficient blood flows to organs, including the brain. In addition to palpitations, you may feel weak, dizzy, and possibly lose consciousness.
Ventricular tachycardia is accompanied by a decrease in blood pressure and in some cases can cause ventricular fibrillation. Cardiac arrest is a very serious event that requires emergency medical care and defibrillation to restore heart rhythm. Unfortunately, this procedure is not always possible in the first minutes of cardiac arrest. Therefore, the implantable CRT/ICD has a built-in defibrillator that provides the emergency therapy (shock) needed to restore normal rhythm.
Are there alternative treatments?
Alternative treatment for heart failure.
The possibility of alternative treatment depends on the form and stage of heart failure.
Mild forms of heart failure respond well to medication, lifestyle changes and diet. The mainstays in the treatment of heart failure are a strict diet and the use of drug therapy aimed at eliminating the causes of heart failure.
If the cause of heart failure is coronary artery disease or valvular heart disease, your doctor will refer you to a heart surgeon. Surgical correction of valve pathology and angioplasty of the affected arteries of the heart can completely eliminate all symptoms and manifestations of heart failure.
In the most complex cases of heart failure with ineffective drug therapy to save the patient's life, the issue of cardiac transplantation or the use of left ventricular bypass systems (artificial heart ventricle) will be considered.
Cardiac resynchronization devices (CRT) are considered as an alternative to heart transplantation (HT).
The advent of cardiac resynchronization devices in medical practice has made it possible to effectively combat the manifestations of HF in cases where the cause of HF is myocardial dyssynchrony, low ejection fraction and left bundle branch block (LBBB). Numerous implantations of devices have given reason to consider the effect of such therapy not only as a “bridge to transplantation,” but also as a “bridge to recovery.” CRT implantation is indicated for patients with severe forms of heart failure, NYHA functional class III-IV.
Alternative treatments for life-threatening cardiac arrhythmias.
Heart rhythm disturbances can occur in different parts of the heart and manifest themselves in the form of extrasystole or very fast rhythm (tachycardia). As a rule, heart rhythm disturbances are divided into functional (reversible) and organic (non-reversible). Functional disorders include those types of heart rhythm disturbances that are caused by endocrine and metabolic disorders, poisoning, alcohol use, and severe stress. Timely correction and elimination of the causes of arrhythmia leads to recovery.
The most dangerous arrhythmias are considered to be rhythm disturbances caused by damage or changes in the myocardium, which are observed with myocardial infarction, myocarditis, cardiosclerosis, arrhythmogenic dysplasia of the right ventricle, etc.
Most cardiac arrhythmias respond to antiarrhythmic therapy. An effective method of surgical treatment is radiofrequency ablation (RFA) of pathological heart rhythms. However, for many patients, antiarrhythmic therapy may not be effective, and RFA is contraindicated due to the anatomical features and severity of the patient’s condition. In such a situation, pacemakers with ICD function are the best method and choice to prevent serious complications of VT.
It is obvious that severe forms of HF are often accompanied by attacks of VT, the occurrence of which can be fatal for a patient with HF. Many studies conducted around the world have confirmed the high effectiveness of implantable pacemakers with CRT/ICD functionality.
Thus, CRT/ICD provides resynchronization therapy for severe forms of heart failure and high protection against the risk of death from life-threatening arrhythmias and cardiac arrest.
Indications and contraindications for CRT/ICD implantation
Indications for implantation of CRT/ICD cardiac resynchronization devices are determined by your doctor based on your medical history and medical studies.
Indications for CRT/ICD implantation:
- Moderate and severe degree of heart failure (III-IV functional class), when the symptoms of heart failure are not amenable to drug therapy in compliance with all diet regimens (water restriction, etc.).
- Decreased contractility of the heart. The ejection fraction is equal to or lower than 35%.
- Uncoordinated contractions of the ventricles with the manifestation of electrical dyssynchrony of the myocardium on the electrocardiogram (QRS duration greater than 120 milliseconds), and/or during an echocardiographic study with the identification of mechanical dyssynchrony of the walls of the myocardium of the left ventricle.
Patients with heart failure who are not candidates for CRT/ICD implantation and who do not meet the indications for cardiac resynchronization (as determined by the treating physician):
- Patients with moderate heart failure (functional class I-II), whose symptoms are well controlled by drug therapy and diet.
- Patients whose heart failure is not associated with uncoordinated ventricular contractions (no dyssynchrony).
Living with an ICD
Your ICD. Some facts
- The human heart is a muscle approximately the size of a fist. The heart has a complex electrical system. It produces its own electricity, which causes the heart to contract and relax at the correct rhythm. Thanks to this, the heart muscle is able to pump blood throughout the body.
- For the heart to work properly, the chambers must contract in a coordinated manner and the resting heart rate must be between 60 and 100 beats per minute.
- Electrical signals may be blocked or arrive irregularly. This causes the heart to beat too fast (tachycardia or fibrillation) or too fast (bradycardia).
- Implantable cardioverter defibrillators (ICDs) are miniature computers that fit in the palm of your hand. Typically, they are implanted under the skin in the chest area.
- ICDs help cope with dangerous disorders that result in accelerated rhythm. These disorders occur in the lower chambers of the heart (the ventricles) and are called ventricular tachycardia (VT) and ventricular fibrillation (VF).
- In ventricular fibrillation, the heart beats so fast that it flutters and loses its ability to pump blood. This condition leads to sudden cardiac arrest. If the heart is not immediately made to beat, the person will die.
- If ventricular fibrillation occurs, the ICD can send a shock to the heart muscle to stop the fibrillation or fibrillation muscle contractions.
- ICDs have saved hundreds of thousands of lives and reduced the risk of sudden cardiac arrest for patients.
Living with an ICD
An ICD is a small implantable device that looks similar to a pacemaker (pacemaker). Typically, the ICD fits easily in the palm of your hand. While pacemakers speed up slow heart rates, ICDs are designed to slow down fast rates and provide life-saving therapy when the rate is dangerously fast. ICDs have saved hundreds of thousands of lives and reduced the risk of sudden cardiac arrest for patients.
Why do I need an ICD?
The heart has a complex electrical system. It constantly produces its own electricity, which causes the heart to contract and relax at the correct rhythm. Thanks to this, the heart muscle is able to pump blood throughout the body. Electrical signals may be blocked or arrive irregularly. This causes the heart to beat too fast (tachycardia) or too slow (bradycardia). For the heart to work properly, the chambers must contract in a coordinated manner and the resting heart rate must be between 60 and 100 beats per minute.
ICDs are intended for the treatment of dangerous disorders characterized by accelerated rhythm. These disorders occur in the lower chambers of the heart (the ventricles) and are called ventricular tachycardia (VT) and ventricular fibrillation (VF). If the ventricles fibrillate, they do not contract in a normal rhythm and efficient pumping of blood is impossible. Ventricular fibrillation becomes permanent and effective pumping of blood ceases. Most doctors believe that ventricular fibrillation is a condition in which the heart beats at least 300 beats per minute. If the heart muscle flutters, it is no longer able to pump blood. If in this case measures are not taken immediately, the patient may die.
Typically, ventricular fibrillation leads to sudden cardiac arrest. It should be noted that, if assistance is provided immediately, some people can be brought out of the state of sudden cardiac arrest, despite such a formidable name. Immediate care includes cardiopulmonary resuscitation. Its task is to maintain the blood pumping process. In addition, the erratic electrical activity of the heart should be stopped, the heart's normal rhythm should be restored, and serious complications that occur during periods of significant reduction in blood flow should be prevented. This requires a four to six minute shock from an external defibrillator or implantable cardioverter defibrillator (ICD).
How does an implantable cardioverter defibrillator (ICD) work?
An ICD is a medical device that is implanted in the body to monitor the rhythm of the heart and detect certain types of potentially dangerous rhythm disorders that cause very rapid heartbeats. The ICD is implanted under the skin and connected to one or two electrodes (thin insulated wires) that are placed in or on the heart muscle. Once ventricular fibrillation occurs, the ICD can send a shock to the heart muscle to stop the fibrillation or fibrillary muscle contractions.
How does a shock restore heart rhythm?
The pattern of electrical impulses in the heart is called the heart rhythm. The ICD tracks every beat of your heart. When it senses a dangerously fast rhythm, the ICD delivers an electrical shock. This interrupts the abnormal rhythm pattern and gives the heart the opportunity to restore its normal heart rate.
What other therapy does an ICD perform?
Defibrillation is the most important function that an ICD performs. Some ICDs are also capable of performing low-energy therapy to treat less severe rhythm disorders. This type of therapy is called anti-tachycardia pacing (ATP). In addition, an ICD can stimulate the heart in the same way as a pacemaker. These devices not only help maintain your heart rate, but also store a lot of information about your heart. The collected information can be obtained by the attending physician. They will help the doctor program the device so that the therapy performed best suits your condition.
What sensations accompany the discharge?
Different people perceive shock differently, so the experience of an ICD shock varies greatly. Some people don't even feel it. Some people experience moderate intensity sensations. Others describe the shock as a shock to the chest. Although the shock may cause discomfort, it means that the ICD has responded to a very dangerous heart rhythm disorder.
How often will I receive a shock?
It depends on the characteristics of the patient. Some people live for years with an implanted ICD and have never received a shock. Others receive shocks more often. It is not unusual for ICD patients to receive one or two shocks over many years. Ask your doctor about what to prepare for, but keep in mind that even he is not able to absolutely accurately predict what kind of therapy you will need.
What to do after the discharge?
The best thing is to find a place where you can sit down and catch your breath. Very soon the normal heart rate will be restored. You may feel slightly dizzy or disorientated for a short time. Do not worry. Some patients require only a few minutes to recover, while others require several hours. Most doctors ask patients to contact them after shock. The attending physician may ask you to come to him after the discharge for control. Because your healthcare provider is aware of your clinical condition, it is best to contact your healthcare provider for instructions about post-shock behavior.
How will the ICD “understand” that a shock is not needed if the heart is beating rapidly for a natural reason?
Any person leading an active life will experience tachycardia under stress. This is fine. After stopping physical activity, a healthy heart gradually restores its normal rhythm of contractions.
Most modern ICDs are capable of distinguishing natural from pathological tachycardia. Medically speaking, a fast heart rate caused by exercise differs from a potentially dangerous fast heart rate in the area where electrical impulses are generated in the heart. During physical activity, a healthy heart generates electrical impulses in its upper chambers. After this, the impulses are transmitted along the conduction pathways of the heart to the lower chambers, causing them to contract. Dangerously fast rhythms originate in the ventricles. To distinguish between these pulses, ICDs use formulas called “discriminators.”
How is an ICD implanted?
Generally, cardiac device implantation does not require general anesthesia. Usually, pain relief while maintaining consciousness is sufficient for implantation. You will receive medication to help you relax, but during the procedure you will remain aware of everything that is happening and will be able to hear and even talk to the doctor and nurses. Several medications will be administered when the incision is made. Although the local anesthetic will prevent severe pain, you may feel some pressure when the device is implanted.
What to expect during ICD implantation surgery?
First, the doctor will make a small incision in the upper chest and find a vein. A small puncture will be made in the vein, and then long flexible wires will be passed through the vein into the heart. The operating team monitors the progress of the electrode using a high-mounted monitor called a fluoroscope. The monitor shows a moving image in the X-ray part of the spectrum. Often the placement of the electrodes is the longest part of the operation. Once the electrodes are placed, your doctor will check them to make sure the electrodes are positioned optimally to deliver energy to the heart.
Once the electrodes are placed, your doctor will connect you to the implantable device. Then the doctor, separating the skin and underlying tissue from the underlying muscle, will form a “pocket.” Once the ICD is connected to the leads, it is placed in a pocket. After placing the device, the doctor will stitch the incision.
After the incision has healed, many people barely notice the small scar and slight protrusion. However, if the patient is short or thin, the device may protrude a little more. If you are concerned about how you will look after surgery, discuss this with your doctor. Sometimes the device can be placed in another place where it will not be so noticeable.
The length of surgery depends on the type of device being implanted, as well as your anatomy and the time spent determining the optimal position of the electrodes. Typically, ICD implantation lasts several hours.
What to expect after surgery?
Immediately after surgery, you will be taken to the intensive care unit. You may experience increased sensitivity at the implantation site for some time. You will stay in the hospital for anywhere from several hours to several days. Discuss the specifics of your case with your doctor.
During the postoperative period, carefully follow all instructions from your doctor. First, be sure to report any redness, tenderness, or tenderness near the implant site. If you notice redness or tenderness around your scar after leaving the hospital, contact your doctor immediately without waiting for your appointment.
How long will the recovery period last?
Because every patient is different, it will be difficult to accurately determine the length of the recovery period in your specific case. Follow your doctor's instructions carefully. For some time after surgery, your usual activities will be limited. Once your recovery period is complete, your doctor will be your best source of advice on how to resume your normal lifestyle.
What are the risks of using an ICD?
Your doctor is the best person to tell you about the risks of using an ICD. Do not forget to ask him all the questions you have and share all your doubts. A small number of patients with ICDs develop complications related to the implantation procedure. These complications include infection, a reaction to drugs used during surgery or to the device itself, blood loss, or damage to a blood vessel, heart wall, or other organs.
After the operation, you will experience some discomfort and loss of strength. Once you recover, you will feel better. However, some patients continue to experience discomfort at the ICD implantation site. If you also feel discomfort, tell your doctor about it. After ICD implantation, it is important to take certain precautions. You can safely use most appliances that are in working order and properly grounded, but you should avoid strong magnetic fields, including MRI devices. Your doctor will discuss any necessary precautions with you. In addition, you should carefully read all brochures supplied with your product, paying particular attention to the “Caution” and “Attention” sections. These sections contain important safety information.
ICD therapy may not stop the arrhythmia. Moreover, there is a possibility that therapy will make it worse. However, in an attempt to control the arrhythmia, the ICD will deliver more intensive therapy. There is a small risk that the ICD may fail to deliver needed therapy or provide therapy when it is not needed. An ICD does not always eliminate all symptoms of an arrhythmia. You may continue to feel dizzy or faint.
How often should I visit my doctor after implantation?
For routine check-ups, you will need to see a cardiologist or GP regularly. Immediately after surgery, you may need to visit your doctor several times. All of these visits are very important because they will allow the doctor to ensure that the implanted device is functioning correctly. The necessary adjustments are made painlessly in the doctor's office using a desktop computer called a programmer. Your doctor will also check whether your incision is healing. After this, you will visit your doctor regularly for follow-up examinations. Your doctor will advise you how often to do them. If the situation is stable, your doctor may suggest that you visit him once or twice a year or after you receive a shock. Your doctor may also need to see you if your family or GP has any concerns.
If many changes were made during your visit to the doctor, you may need to make your next visit a shorter period of time to ensure that the changes are effective and that there are no problems associated with them.
How is the inspection carried out?
The follow-up examination is absolutely painless and usually takes less than half an hour. During the examination, the doctor or nurse will place a sensor on the area of skin located over the implanted device. This sensor is similar in size and shape to a TV remote control.
Some devices do not require a sensor because they transmit information remotely. The device reports battery status information to the programmer, performs other system checks, and reports your heart rate information accumulated since your previous health check. If you have experienced a shock or therapy in the past time, the programmer will receive this information.
If necessary, the doctor can change some device settings to optimize therapy. For these reasons, it is very important that you follow your follow-up inspection schedule.
How will the doctor replace the battery in my device?
Implanted devices are powered by special batteries that are designed to last for a long time. These batteries do not die suddenly like flashlight batteries, but provide multiple warnings that the end of their life is approaching. Monitoring the condition of the batteries by the attending physician is part of the routine follow-up examination. Most devices' batteries last between three and six years, although this depends on the device and how often it sends electrical impulses to the heart. Once the device warns that the battery is low, your healthcare provider will schedule a replacement. Implantable devices are sealed, so batteries cannot be replaced. Instead, the doctor implants a new device. As a rule, this operation takes less time than the first one, since the doctor only needs to connect the new device to the existing cardiac electrodes.
Will an implantable device change my life?
You can live longer, healthier, more productive and happier. After surgery, you should limit your exercise for a while. Make sure you carefully follow all your doctor's instructions. Very soon you will be able to do everything you did before, and even more.
Should I stay away from devices like microwaves, magnets, and strobe lights?
Implantable devices cannot be damaged by working appliances such as microwave ovens, electric blankets, and most power tools. Using electric arc welding equipment or working with vehicle ignition systems will also not cause harm to the ICD. However, they may cause short-term interference with the proper operation of the device. Some medical equipment may also interfere with ICD operation. If you experience dizziness or palpitations (fast, irregular heartbeats), simply turn off the electrical equipment or move away from it. After this, the implanted device will restore normal functioning. If you must use equipment that may cause EMF, consult your healthcare professional. You can also request instructions from the equipment manufacturer.
Will medical equipment interfere with my ICD?
Although medical equipment generally does not interfere with ICD function, some devices can interfere with its function. Before you undergo any medical, including dental, procedure or test, such as electrosurgery, electrocautery, lithotripsy, or radiation therapy, tell your healthcare provider that you have an ICD implant.
Even with the ICD turned off, any diathermy is contraindicated for you. This procedure can damage the tissue around the implanted leads or permanently damage the ICD. Try to stay away from transcutaneous neuro- and myostimulation (TENS) devices. They may interfere with the operation of the ICD. Magnetic resonance imaging (MRI) scanners can seriously damage the ICD. When approaching or standing in the MRI room, the ICD may not function properly.
Can I use a mobile phone?
Mobile phones that send electromagnetic pulses can interfere with the normal functioning of the device. However, you can minimize the risk by taking simple precautions, such as not carrying your phone in your chest pocket above the ICD and keeping the device near the ear farthest from the ICD. ICDs contain special filters that protect devices from interference generated by mobile phones.
Will my iPod® or other portable media player affect the performance of my ICD?
There is no evidence that a portable media player such as an iPod or MP3 interferes with the normal functioning of the devices.
When can I resume physical activity?
Ask your doctor if you can resume physical activity. It is important to avoid shock to the area of the implanted device. So it's best to avoid contact sports like football. Otherwise, the device or electrodes may be damaged. After implantation, you may have more energy. Many people believe that by reducing the severity of symptoms, strength increases.
Can I do activities that require intense physical activity, such as hiking, skiing, or jogging?
It is best to always discuss your plans with your doctor. The doctor will give you advice about intense physical activity based on knowledge of your capabilities and condition. If the sport you play involves stress on your arm or chest (such as swimming or golf), you may want to discuss your pre-implant exercise with your doctor. This may influence the choice of device type and implantation site.
Is sex safe for me?
Typically, the implanted device does not have a negative impact on the patient's sex life except for a short period of hospital stay and recovery. However, it is important to follow your doctor's instructions about resuming physical activity.
Will I be able to drive a car?
Talk to your doctor about this. Keep in mind that although an ICD can stop fast heartbeats, it may not be able to prevent symptoms associated with the rhythm (such as dizziness and fainting). Before driving again, discuss the advisability of doing so with your doctor.
Can I travel?
Your doctor will best answer this question. Many ICD patients find that with a little more care and planning, they can enjoy traveling to many parts of the world. It always makes sense to plan your route carefully and leave a copy of the program with your loved ones. Just in case of difficulties along the way.
Will airport security systems affect the performance of my device?
Many patients are concerned about the security systems used at airports. They worry in vain. Indeed, security rules at airports have become stricter, but having an implanted device will not bring any additional inconvenience. It is best to go through the airport metal detector at normal speed. If an alarm sounds (which is completely optional), this only means that the system has detected the presence of metal in the implanted device.
Please present your patient card for screening. Ask for a manual search.
A security officer may use a hand-held metal detector. In this case, be sure to inform the supervisor that this procedure must be performed quickly and the sensor should not be held over the implanted device for more than a second.
What else should I know about traveling if I have an implanted device?
When traveling, be sure to carry important medical information with you, such as the names and dosages of medications, the name and telephone number of your doctor, and emergency medical care information. Also ask your healthcare provider for a copy of the most recent printout of the programmer test data and settings made during the last test. If you are traveling to a country that speaks Spanish, French or German, your doctor may be able to give you a printout in the appropriate language. (Some devices may soon be able to print in Italian, Japanese and Chinese.) Carry enough medications with you. If you are traveling by train or plane, keep some of your medications in your carry-on luggage and some in your suitcase.
Finally, let the attendants know if you have special dietary needs and develop healthy eating habits while on the road.
Do I need to take medications after ICD implantation?
Ask your doctor this question. Typically, an implanted device does not replace medications. Instead, the drugs and the implanted device work together. However, your doctor may adjust the dose.
Are there any food restrictions?
In general, to keep your heart healthy, doctors recommend eating foods that are low in sodium, fat, and sugar and rich in fiber and carbohydrates.
What is ICD?
An implantable cardioverter defibrillator (ICD) is used to treat heart rhythm problems in which your heart beats too quickly or irregularly. When the ICD detects a heart rate that is too fast, it sends electrical impulses to your heart. These impulses can restore normal heart rhythm. The ICD combines a pacemaker and a defibrillator; its main functions will be described in detail in the sections of this brochure. The ICD is implanted in the upper chest and is small in size, about the size of a small child's palm or the size of a pager. Implantation is performed strictly according to confirmed indications, after research has been carried out according to the doctor’s recommendations.
Subsequent visits
After the stimulator is implanted, your doctor will schedule your next visit. It is important to remember that your health now largely depends on the correct functioning of the ICD. The effectiveness of such therapy depends on a properly selected ICD program and antiarrhythmic therapy. The frequency of consultations will be determined by your attending physician, and it will depend on your state of health and heart rhythm disorders.
During your consultation, your doctor will use a programmer to evaluate the performance of the ICD.
Your doctor will test your ICD:
• check the operation of the pacemaker;
• check the effectiveness of the main functions;
• check the battery capacity;
• will check the chronology of all events recorded by the ICD;
• if the ICD discharged the defibrillator, the doctor will evaluate the effectiveness of the therapy and possibly make adjustments to the stimulator program. After programming, the doctor may change antiarrhythmic therapy or prescribe additional tests. It is important to remember that the performance of your ICD depends on the settings of the basic functions and the correct antiarrhythmic therapy. Therapy is needed to exclude possible attacks of dangerous ventricular arrhythmias.
Why does my doctor recommend ICD implantation?
A patient’s circulatory arrest can occur due to conduction disturbances (blockades), ventricular fibrillation and ventricular tachycardia.
If a person is at high risk of circulatory arrest for this reason, a cardioverter-defibrillator is implanted. In addition to the stimulation function for bradysystolic rhythm disturbances, it has the function of interrupting ventricular fibrillation (as well as ventricular flutter, ventricular tachycardia).
ICDs are implanted:
- patients who have had episodes of sudden cardiac death or ventricular fibrillation;
- patients who have had a heart attack and are at high risk of sudden cardiac death;
- patients with hypertrophic cardiomyopathy and at high risk of sudden cardiac death;
- patients who have had at least one episode of ventricular tachycardia;
Indications for ICD implantation – who needs surgery?
The device in question is implanted in the following pathological conditions:
- The patient has a history of sudden cardiac arrest.
- Insufficient contraction of the heart muscle - ventricular fibrillation.
- Severe ventricular tachyarrhythmias. The introduction of an ICD will prevent sudden cardiac arrest.
- Heart rate is significantly lower than normal.
- A history of serious arrhythmias (1 or more).
- Myocardial infarction, in which the electrical conductivity of the heart was disrupted. This phenomenon may cause dangerous arrhythmias to appear in the future.
- Heart failure.
Types and degrees of heart block - symptoms and consequences of heart block
Video: Installation of a pacemaker: indications, stages of surgery and the principle of treatment of cardiac arrhythmia
Are there alternative treatments?
Heart rhythm disturbances are a very complex branch of cardiology. The human heart works throughout life. It contracts and relaxes 50 to 150 times per minute. During the systole phase, the heart contracts, ensuring blood flow and delivery of oxygen and nutrients throughout the body. During the diastole phase it rests. Therefore, it is very important that the heart contracts at regular intervals.
Heart rhythm disturbance is a disturbance in the frequency, rhythm and sequence of contractions of the heart muscle. Heart rhythm disturbances can occur in different parts of the heart and manifest themselves in the form of extrasystole (extraordinary contraction) or a very fast rhythm (tachycardia). As a rule, heart rhythm disturbances are divided into functional (reversible) and organic (non-reversible). Functional disorders include those types of heart rhythm disturbances that are caused by endocrine and metabolic disorders, poisoning, alcohol use, and severe stress. Timely correction and elimination of the causes of arrhythmia leads to recovery.
The most dangerous arrhythmias are considered to be those rhythm disturbances that are caused by damage or changes in the myocardium, which are observed with myocardial infarction, myocarditis, cardiosclerosis, arrhythmogenic dysplasia of the right ventricle, etc. Most cardiac arrhythmias are amenable to antiarrhythmic therapy. An effective method of surgical treatment is radiofrequency ablation (RFA) of pathological heart rhythms. However, for many patients, antiarrhythmic therapy may not be effective, and RFA is contraindicated due to the anatomical features and severity of the patient's condition. In such a situation, pacemakers with ICD function are the best method and choice to prevent serious complications of VT.
Who is not eligible for ICD implantation?
Not all patients are candidates for ICD implantation. In many patients, tachyarrhythmia is temporary or in cases where the use of an ICD cannot eliminate the cause of the underlying disease.
These include:
- Patients whose tachyarrhythmias are associated with a reversible cause, such as treatment for drug addiction, electrolyte imbalance, etc.
- Patients with tachyarrhythmias as a consequence of a heart attack or non-sustained episodes of myocardial ischemia.
- Patients with frequent episodes or continuous VT.
- Patients whose tachyarrhythmias occurred after a lightning strike or electric shock.
Alternative treatment for heart failure
The possibility of alternative treatment depends on the form and stage of heart failure.
Mild forms of heart failure respond well to medication, lifestyle changes and diet. The mainstays in the treatment of heart failure are a strict diet and the use of drug therapy aimed at eliminating the causes of heart failure.
If the cause of heart failure is coronary artery disease or valvular heart disease, your doctor will refer you to a heart surgeon. Surgical correction of valve pathology and angioplasty of the affected arteries of the heart can completely eliminate all symptoms and manifestations of heart failure.
In the most complex cases of heart failure with ineffective drug therapy to save the patient's life, the issue of cardiac transplantation or the use of left ventricular bypass systems (artificial heart ventricle) will be considered.
Cardiac resynchronization devices (CRT) are considered as an alternative to heart transplantation (HT).
The advent of cardiac resynchronization devices in medical practice has made it possible to effectively combat the manifestations of HF in cases where the cause of HF is myocardial dyssynchrony, low ejection fraction and left bundle branch block (LBBB). Numerous implantations of devices have given reason to consider the effect of such therapy not only as a “bridge to transplantation,” but also as a “bridge to recovery.” CRT implantation is indicated for patients with severe forms of heart failure, NYHA functional class III-IV.
Should I be concerned about my ICD?
The ICD is designed to improve quality of life by helping overcome symptoms and provide confidence in the face of the consequences of sudden cardiac arrest. Remember, your ICD is there to protect you from tachyarrhythmias. ICD pacemakers are extremely reliable—they save lives every day.
Give yourself and your family time to adjust to life with an ICD. Most patients quickly get used to it. However, some people feel depressed, anxious, and afraid. If these feelings do not go away after 2 months, consult your doctor. You can also consult with another person who has undergone a similar operation and ask them how they and their family members have adjusted. Over time you will feel confident. You will be able to return to work, normal activities and family life. Your family can help you. You need to give her information about the cardioverter defibrillator and what help you may need.
Will I experience pain or discomfort?
Adaptation to ICD occurs gradually. First of all, follow your doctor's advice. Most patients feel “protected” from the disease and are able to return to a full, active life.
After the wound has healed, pain is unlikely; discomfort at the site of the stimulator will persist for some time when raising the arm. Typically, many patients forget that they have an ICD implanted. After the scar has formed, only a thin light strip remains.
WARNING: Consult your doctor if you continue to experience pain after your wound has healed.
What to expect after ICD implantation, are there any risks and possible complications?
for the first 1-3 days after surgery . During this period of time, the doctor once again checks the quality of operation of the installed device and monitors the general condition of the patient.
If conventional surgical sutures were used to close the wound, they are removed 10 days after ICD implantation.
Swelling and pain in the area of the device for the first couple of days are quite normal. Mild analgesics may be prescribed to relieve pain.
Discomfort associated with the introduction of a foreign body will be present for the first 2 months , especially when raising the arm. However, over time, a person gets used to the cardiac defibrillator and does not feel its presence.
A thin white scar forms at the site of the incision.
Possible exacerbations:
- Infection of the surgical site.
- Bleeding from the area where the ICD was placed.
- Poor tolerance of anesthetics used during manipulation.
- Damage to a nerve root, heart wall, or blood vessel.
- Entry of air into the pleural cavity.
Other likely consequences:
- Sending impulses that are not needed . This is especially true for young patients: their excessive physical activity increases the heart rate, which leads to unnecessary discharges. This phenomenon is usually accompanied by pain in the sternum and can cause damage to the organ. In such cases, you should consult a doctor: he will reconfigure the device or prescribe certain medications: Sotalol, Amiodarone, beta blockers, etc.
- Absence of impulses in case of cardiac arrhythmia . The reason for this lies in the malfunction of the stimulator - it needs to be changed or adjusted.
In addition, in order to protect the device from malfunction, it is necessary to avoid prolonged contact with devices that produce magnetic fields.
Examples of such devices are:
- Mobile/cell phones, MP3 players. If they are turned on, they should not be carried in a pocket in close proximity to the ICD.
- Microwave.
- Electric generators.
- Welders.
- Metal detectors. Before undergoing them, it is necessary to inform the personnel that there is a cardioverter-defibrillator in the body. You can pass through such detectors, but you should not sit near them or linger in the opening.
- Magnetic resonance tomographs.
The patient can confirm that an ICD is implanted into the body using a special certificate card , which must be given to him by a doctor. You must carry this card with you at all times.