Based on our own experience and literature data, a description of the genetic nature of hypertrophic cardiomyopathy, its clinical picture, and the results of instrumental studies is given. Treatment is being discussed. Criteria for poor prognosis are given.
Hypertrophic cardiomyopathy in children
Based on our experience and the literature describes the genetic nature of hypertrophic cardiomyopathy, its clinical presentation, results of instrumental studies. It is discuss the treatment. Some criteria of poor prognosis were held.
Hypertrophic cardiomyopathy (HCM) is a structural and functional lesion of the myocardium with an increase in its thickness (mass) with a known or suspected genetic defect of the cardiomyocyte sarcomere protein, inherited autosomal dominantly with varying penetrance and expressivity in the absence of systemic hypertension, storage diseases, hypothyroidism, atherosclerotic coronary sclerosis, valve defects, congenital heart defects and other conditions that could explain the increase in myocardial mass. Modern possibilities for the treatment of HCM with long-term support of a sufficiently high quality of life have actualized the problems of early diagnosis and adequate choice of patient management tactics [1, 2].
Etiology.HCM is inherited according to Mendelian laws in an autosomal dominant manner. The form of the disease in probands and their closest relatives is the same in 60% of cases. The genes responsible for the disease are localized on chromosome 6 (15 genes) and on the long arm of chromosome 14 [3]. Gene changes are represented by more than 400 missense mutations responsible for the regulatory, structural or functional characteristics of thin or thick filaments of cardiac sarcomeres (β-myosin heavy chain, actin, titin, myosin-binding protein C, tropomyosin T, etc.). The number of mutations itself determines the clinical variability of HCM. More than half of all genetically identified cases of HCM are determined by mutations in 3 genes that determine defects in the β-myosin heavy chain, myosin-binding protein C, and cardiac troponin T. Another 13 genes are responsible for infrequent cases of defects in titin, α-tropomyosin, α-actin, and cordial troponin I, myosin light chain. But among people with clinically and instrumentally diagnosed HCM and subjected to molecular genetic testing, gene abnormalities were detected only in 50-80% of cases [4, 5]. This means that in 20-50% we are dealing with mutations that have not yet been identified. It is likely that different populations will have their own mutations. Thus, it is suggested that the Russian population may be characterized by a missense mutation in the β-MHC gene.
The polymorphism of the clinical picture is explained by the insufficiently studied interaction of various genes (mutation MYH7 - pronounced hypertrophy, early onset and severe course; mutation TNNT2 - moderate hypertrophy; mutation MYBPC3 - incomplete penetrance and relatively late onset), gender, and external factors.
Pathophysiology . The gene defect leads to discoordination of the activity of myofibrils and subsequent fibrosis and hypertrophy of the myocardium. Chaotic cellular structure already occurs in areas without signs of hypertrophy and which are an arrhythmogenic substrate of ventricular tachycardia and fibrillation. At the same time, the intima of the intramural coronary arteries thickens, oxygen transport into the thickened myocardium is disrupted, ischemia, cell death, and sclerosis occur. The walls of the ventricles thicken, but the internal size remains unchanged or even decreases. Systolic function does not change for a long time, myocardial rigidity increases sharply, end-diastolic pressure increases, and blood return is inhibited. Hypertrophied myocardium can narrow the LV outflow tract. The degree of obstruction varies depending on the thickness of the interventricular septum, the location of the mitral annulus, anterior systolic movement of the mitral valve leaflets, and the intensity of myocardial contraction (therefore, digitalis preparations are contraindicated). The degree of obstruction does not correlate with the risk of sudden death. Progression of the disease leads to ventricular dilatation.
An experiment on animals with a positive HCM genotype but a negative phenotype showed that the administration of calcium channel blockers before the development of hypertrophy can prevent the disease [6]. Such experimental therapy is also carried out in people who are presymptomatic carriers of the HCM genotype.
The prevalence of HCM in children is 3-5: 1 million, median age is 7 years, 1/3 of all cases are diagnosed before the age of 1 year. In 25-58% of 1st degree relatives, echographic signs of HCM are detected. The incidence of HCM is approximately the same in different populations, although atypical variants of HCM are more common in Asia. Among children, there are gender differences in the incidence of HCM, but in adulthood, the disease is more often detected in men. The differences are explained by hormonal factors, environmental influences, more severe symptoms or a greater degree of LV outflow tract obstruction in men. All this determines more frequent studies leading to the diagnosis of HCM.
Clinical picture. There may be no complaints, and in these cases the diagnosis of HCM is the result of random echocardiographic studies. According to the results of our own studies (84 patients), indications of fainting, shortness of breath, a feeling of interruptions in the heart, etc. are more common. According to the results of 24-hour blood pressure monitoring, a tendency to bradycardia is recorded, apparently due to a decrease in LV ejection.
Shortness of breath is one of the earliest symptoms and occurs in 90% of patients. Dyspnea is caused by high rigidity of the thickened myocardium, increased end-diastolic pressure and transfer of pressure to the pulmonary circulation.
Syncope and presyncope are common in HCM, especially in children and adolescents with small LV diameter and ventricular tachycardia or sick sinus syndrome or sinus node dysfunction on 24-hour monitoring. In our group of patients they occurred in 27%, more often in the obstructive form of HCM. The presence of fainting is an indicator of a high probability of sudden death. Presyncope, which occurs during a sudden transition to a vertical position, can be caused by transient atrial or ventricular tachyarrhythmia and is considered a predictor of sudden death.
Dizziness is common in children with HCM with a high gradient in the left ventricular outflow tract and is aggravated by physical activity or hypovolemia (profuse sweating in the heat), rapid transition to an upright position, or a Valsalva reaction during bowel movements. Dizziness can occur with rhythm disturbances with decreased cerebral perfusion. Short-term episodes of arrhythmia are manifested by presyncope and dizziness, while persistent arrhythmias lead to fainting and sudden death.
Anginal pain is typical for children with HCM. There is no atherosclerotic coronary sclerosis. The symptoms of myocardial ischemia are explained by the increased need of the thickened myocardium for oxygen, which, if diastole is disturbed, leads to subendocardial hypoxia, especially during physical exertion. The feeling of interruptions in the heart is explained by premature atrial or ventricular contractions, intermittent atrioventricular block, supraventricular or ventricular tachycardia. Undiagnosed ventricular tachycardia is an indicator of a high risk of sudden death.
Orthopnea and paroxysmal nocturnal dyspnea are signs of heart failure in severe types of HCM with venous congestion in the lungs. Congestive heart failure in children occurs in only 10% of cases (much less often than in adults) and mainly before the age of 1 year. It is characteristic of patients with the most pronounced thickening of the myocardium. Congestive heart failure is the result of two damaging factors: high myocardial stiffness and subendocardial ischemia.
The apical impulse is diffuse, elevating, shifted to the left. A double impulse is typical, the upper part of which is formed by increased contraction of the left atrium. The most typical for HCM is the triple apical impulse, the last part of which is caused by isometric contraction of the ventricle. But this option is extremely rare.
Venous jugular pulse - a pronounced wave “a” on the venogram: a sharp increase in end-diastolic pressure in the left ventricle with an increase in pressure in the pulmonary circulation and thickening of the interventricular septum with a decrease in the cavity of the right ventricle, ultimately with inhibition of inflow to it.
The carotid pulse is high, fast and short, which is explained by the high speed of blood flow through the narrowed LV outflow tract. In some cases, the carotid pulse appears as a successive double pulsation of the carotid artery: 1st peak - as described earlier, 2nd - a low rise of the artery in late systole after the fall of the gradient.
Auscultation of the first tone is not changed, the second is usually split, and with a very high gradient it is paradoxical. A gallop rhythm or a third sound is often heard, but in HCM it does not have the same prognostic value as in valvular aortic stenosis. The IV tone is often determined due to forced atrial systole, overcoming resistance to blood flow into the LV. The diamond-shaped systolic ejection murmur (crescendo-decrescendo) is best heard at the point between the apex and the left edge of the sternum, radiates suprasternally, but is not transmitted to the carotid arteries. The intensity of the noise is determined by the subaortic gradient in the LV outflow tract. Since the degree of pressure gradient varies depending on the obstruction and the volume of inflowing blood, the intensity of the noise is not constant. The noise decreases with increasing preload: Valsalva maneuver, Müller maneuver (after forced exhalation, the inhalation movement is performed with the mouth and nose closed (subatmospheric pressure occurs in the chest and lungs = inverted Valsalva maneuver), squatting position. The gradient increases and the noise becomes louder as it decreases preload (nitrates, diuretics, standing) or decrease after exercise (vasodilators). A holosystolic murmur occurs with anterior systolic movement of the mitral valve and a very high gradient in the LV outflow tract. In 10% of children with HCM, a diastolic murmur is heard decrescendo regurgitation at the aortic valve, but with Doppler ultrasound, minimal and moderate aortic regurgitation is detected in 33%.
Additional research. Electrocardiography most often reveals signs of LV hypertrophy, deviation of the electrical axis of the heart, conduction disturbances, sinus bradycardia (33%) with ectopic atrial rhythm and atrial enlargement. With adenosine monophosphate mutation activated PRKAG2, HCM is combined with congenital Wolf-Parkinson-White syndrome and conduction disorders.
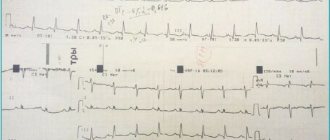
Deep Q waves in the precordial leads (40%), atrial fibrillation (a poor prognostic sign) and P wave abnormalities are relatively common. The size of the Q wave directly correlates with the thickness of the myocardium of the posterior wall of the LV (Fig. 1).
Figure 1. Electrocardiogram of patient N., 5 years old, with obstructive form of HCM. There is a pathologically deep Q wave in leads I, AVL, V5-V6. The voltage of the R wave in leads II, III, AVF, V6 is reduced. The thickness of the interventricular septum according to echocardiography is 1.5 cm, the posterior wall of the left ventricle is 0.7 cm.
The Q wave in leads II, III, aVF was recorded mainly in patients with moderate isolated myocardial hypertrophy. In severe progressive HCM, in addition to leads II, III, aVF, the Q wave was recorded in leads V4-V6; in cases of combined hypertrophy of the LV and right ventricular myocardium - in leads I, II, aVL, V4-V6. It can be assumed that the pathological Q wave is not only an isolated sign of hypertrophy of the interventricular septum, but also an indirect sign of the characteristics of LV hypertrophy. Changes in the repolarization process are typical: a decrease in the amplitude of the T wave (21% of those examined), its pronounced inversion (61%) up to giant negative T waves in leads V1-V6. Patients with the obstructive form of HCM are characterized by atrioventricular blockades.
With Holter monitoring, rhythm and conduction disturbances are recorded much more often than with simultaneous ECG recording.
There are major and minor ECG criteria for HCM. Major criteria include: 1) Q wave change (>40 ms or 1/3R) in at least 2 leads and 2) T wave inversion (≥3 mm) in at least 2 leads. Minor: 1) left atrium enlargement (Pv1), 2) PR<120 ms, 3) His bundle block or hemiblock (or interventricular conduction disorder: QRS≥120 ms), 4) deep wave Sv2, 5) reoplarization disorders. ECG criteria are nonspecific and must be combined with ultrasound data. For adults, echographic criteria are stable due to the completeness of the body’s development. For a child, the concept of normal is more blurred. Therefore, in children it is advisable to use the ratio of the thickness of the interventricular septum and the posterior wall of the LV. The latter is normally always thicker than the interventricular septum.
2D echocardiography is a leading diagnostic technique. The interventricular septum is thickened relative to the posterior wall of the LV. The internal diameter of the ventricle is at the lower limit of normal or reduced (Fig. 2).
Figure 2. Echogram along the long axis of the LV with asymmetric hypertrophy of the interventricular septum. The interventricular septum is sharply thickened and overlaps the LV outflow tract by almost half. 1 and 2 – aortic wall, 3 – interventricular septum, 4 – posterior wall of the LV.
The smaller the LV diameter, the higher the likelihood of fainting. With mitral regurgitation and/or low LV compliance, the left atrium cavity expands. A typical sign of HCM is anterior systolic motion of the mitral valve. It is explained by the displacement of the mitral ring into the outflow tract of the LV due to thickening of the interventricular septum and the shift of the valve leaflets to the septum (the pressure behind the closed leaflets of the mitral valve is high, and in front of them in the outflow tract, according to Bernoulli’s law, the pressure in the fast fluid flow is low) during systole (echographic Venturi phenomenon). Doppler ultrasonography is used to determine the rate of blood ejection in the LV outflow tract or the rate of blood flow in diastole through the left atrioventricular orifice. In the latter case, the velocity in the rapid filling phase (VEF) is reduced, the peak velocity in the systole phase of the left atrium (VA) relative to VEF is increased. This pathological relationship is also found in genotypically positive but asymptomatic patients.
The X-ray picture varies from unchanged to enlarged cardiac shadow. The left atrial arch bulges with high LV stiffness and mitral regurgitation.
Magnetic resonance imaging makes it possible to clarify the degree of obstruction and the anatomy of cardiac structures and reveals myocardial fibrosis, the prevalence of which directly correlates with the risk of sudden death.
Cardiac catheterization is performed to determine the degree of obstruction, the state of diastolic function, the interventricular septum and the coronary arteries.
Laboratory tests are nonspecific and are required only when secondary forms of myocardial thickening are excluded. Genetic testing most often (80% of HCM cases) reveals mutations in 9 sarcomeric genes MYH7, MYBPC3, TNNT2, TNNI3, TNNC1, TPM1, ACTC, MYL2, andMYL3 and in the CAV3 regulator gene.
Histologically, the myocardium is hypertrophied, myocardiocytes and myofibrils are arranged randomly, and fields of fibrosis are visible. In 80% of patients, the walls of the intramural branches of the coronary arteries are thickened, and the lumen is unevenly narrowed. These changes are most often recorded in the interventricular septum and are accompanied by fields of fibrosis. Along with the listed changes, even in supposedly unchanged areas of the myocardium, defects in calcium transport, disturbances in glycogen metabolism and other transformations are found that adversely affect the prognosis of the disease. This point of view can be confirmed by the fact that in 60% of those who died from HCM, according to light microscopy, 10-15% of the myocardial mass was changed, while for a fatal outcome in myocardial infarction or post-infarction cardiosclerosis, damage to at least 50% of the myocardial mass is required [7 , 8].
Doctor's tactics. After identifying myocardial thickening, it is necessary to carry out differential diagnosis with secondary causes of cardiac muscle hypertrophy:
- "the heart of an athlete" Long-term exercise can lead to myocardial hypertrophy, but with an appropriate history, concentric myocardial hypertrophy with expansion of the LV cavity is detected, which is not typical for HCM;
- aortic stenosis, aortic, subvalvular, coarctation of the aorta;
- restrictive cardiomyopathy;
- storage diseases (glycogenosis, mucopolysaccharidosis, amyloidosis, etc.);
- arterial hypertension (including neonatal);
- congenital hypothyroidism, newborn from a mother with diabetes mellitus;
- neuromuscular diseases;
- ventricular fibrillation.
General recommendations, monitoring physical activity and dynamics of disease symptoms. There is no special diet. Parents and patients should be warned about limiting physical activity, abolishing anaerobic exercise, and avoiding sports (especially in cases of arrhythmias and familial cases of sudden death). Avoid dehydration, control body weight. In dynamics, the thickness of the myocardium (myocardial mass), indicators of LV diastolic function, the diameter of its outflow tract, the pressure gradient, the presence of anterior systolic movement of the mitral valve, and arrhythmias are assessed. In the absence of emergency indications, an ECG is performed every 6 months, an ultrasound examination of the heart - annually, during puberty - every 6 months. If symptoms of HCM or signs of obstruction occur, it is advisable to initiate therapy with calcium channel blockers or β-blockers. In case of severe obstruction, together with surgeons, determine the indications for myectomy (or alcohol ablation) and pacemaker implantation. Prevention of bacterial endocarditis with antibiotics is not indicated. Diuretics, inotropic drugs, nitrates and sympathomimetics are contraindicated. Rule out digitalis unless there is uncontrolled atrial fibrillation.
Controlling risk factors for sudden death is the goal of any therapy for HCM. There are no uniform recommendations. Prognostic factors include familial cases of sudden death, familial variants of HCM, anamnestic indications of periods of asystole, unexplained fainting, pressure gradient (disputed), arrhythmias, thickness of the interventricular septum.
Drug therapy. The drugs of choice are β-blockers and calcium channel blockers. For heart rhythm disturbances, amiodarone and other antiarrhythmic drugs are prescribed. β-blockers reduce the pressure gradient in the LV outflow tract and optimize LV compliance. The effect of treatment was recorded in ½ patients. There is no evidence that β-blockers reduce the risk of sudden death. An alternative to β-blockers are calcium channel blockers. They improve diastolic function and reduce the pressure gradient by reducing LV contractility.
Propranolol (Inderal) is a non-selective β-blocker, the dose is adjusted according to the clinical effect. Atenolol (tenormin) is a selective β1 receptor blocker with minimal effect on β2 receptors. Efficiency is higher than that of propranolol.
Verapamil (isoptin) blocks slow calcium channels in vascular smooth muscle cells and myocardiocytes. The dose is selected individually, maximum effectiveness has been recorded during physical activity.
Amiodarone (cordarone), an effective antiarrhythmic drug, has several points of application. If long QT syndrome is excluded, it is the drug of choice in the treatment of life-threatening ventricular arrhythmias refractory to β-blockers.
Implantation of a pacemaker [7] leads to an improvement in the course of HCM and a reduction in pharmacological load.
LV myectomy with a gradient of 50 mm. rt. Art. regardless of whether it was recorded at rest or during provocative tests. In most cases, the positive dynamics of symptoms persists for 5 years. There is no complete correlation between the success of myectomy and the likelihood of sudden death. Catheter transvenous alcohol ablation of the interventricular septum is more dangerous than open surgery. It is fraught with irreversible atrioventricular block, myocardial infarction, necrosis of the interventricular septum with its iatrogenic defect [9].
Forecast. Sudden death may be the first and fatal manifestation of HCM in previously asymptomatic patients. In children and adolescents, sudden death is provoked by physical activity and sports activities. The maximum mortality rate was recorded in children with HCM diagnosed before the age of 1 year. In the group of children over 1 year of age, mortality is 1-1.4% per year [10, 11]. In 80-85% of cases, sudden death is the result of atrial flutter. Ventricular flutter develops after atrial flutter or fibrillation, ventricular tachycardia, supraventricular tachycardia in combination with Wolff-Parkinson-White syndrome, or catastrophically low cardiac output with hemodynamic collapse. The most important condition for preventing sudden death is early diagnosis of HCM, which allows changing lifestyle, physical activity, prescribing medication, determining indications for surgical treatment or implantation of a cardioverter defibrillator. Taking into account the autosomal dominant type of inheritance, in order to prevent familial cases of sudden death, examination of relatives is required.
Other complications of HCM include infective endocarditis, heart failure, arrhythmias, and atrial fibrillation with intramural thrombosis.
The criteria for poor prognosis and progressive course of HCM in children are:
- family history of sudden death;
- formation of a QS type complex and increasing conduction disturbance along the left bundle branch;
- high grade ventricular arrhythmia;
- atrial fibrillation;
- sick sinus syndrome;
- distal atrioventricular block 1-2 degrees;
- initially low rates of heart rate variability or their decrease by 30% during observation;
- decreased heart rate variability while taking β-blockers.
Conclusion
Hypertrophic cardiomyopathy is a genetically determined disease that rarely manifests itself in childhood and is more often detected in adults. Myocardial hypertrophy is often asymmetrical. Although any sector of the LV can be affected, the interventricular septum often becomes thickened with obstruction of the LV outflow tract. Systolic functions remain intact for a long time, but compliance suffers early. HCM is a chronic disease with a variable clinical picture from the complete absence of clinical symptoms to significant limitation of vital activity with sudden death. HCM is the leading cause of sudden death during exercise in adolescents. The pediatrician is required to organize interdisciplinary and interprofessional support for patients with the choice of therapeutic or surgical tactics, determine the degree of risk of sudden death and its prevention, and screening examinations of relatives.
V.M. Delyagin, E.A. Tikhomirova, A. Urazbagambetov
Federal Scientific and Clinical Center for Pediatric Hematology, Oncology and Immunology, Moscow
Delyagin Vasily Mikhailovich - Doctor of Medical Sciences, Chief Researcher of the Department of Rare Diseases, Head of the Department of Functional Diagnostics
Literature:
1. Maron B. Hypertrophic cardiomyopathy. A systematic review // J. Am. M.As. - 2002. - Vol. 287. - P. 1308-1320.
2. Maron B., McKenna W., Danielsen W. et. al. American College of Cardiology // Eur. Heart J. - 2003. - Vol. 24. - P. 1665-1691.
3. Jarcho J., McKenna W., Pare J. et. al. Mapping a gene for familial hypertrophic cardiomyopathy to chromosome 14q1 // New Engl. J. Med. - 1989. - Vol. 321. – P. 1372-1378.
4. Bos J., Towbin J., Ackerman M. Diagnostic, prognostic, and therapeutic implications of genetic testing for hypertrophic cardiomyopathy // J. Am. Coll. Cardiology. - 2009. - Vol. 54. - P. 201-211.
5. Kim L., Devereux R., Basson C. Impact of genetic insight into Mendelian disease on cardiovascular clinical practice // Circulation. - 2011. - Vol.123. — P. 544-550.
6. Semsarian C., Ahmad I., Giewat M. et. al. The L-type calcium channel inhibitor diltiazem prevents cardiomyopathy in a mouse model // J. Clin. Invest. - 2002. - Vol. 109. - P. 1013-1020.
7. Epstein A., DiMarco J., Ellenbogen K., Estes N. et. al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology // J. Am. Col. Cardiol. - 2008. - Vol. 51. - P. 62.
8. Siegenthaler W. Differential diagnosis innerer Krankheiten // Neubearbeitete Auflage. - Stuttgart: Georg Thieme Verlag, 1993.
9. Sorajja P., Valeti U., Nishimura R., Ommen S. et. al. Outcome of alcohol septal ablation for obstructive hypertrophic cardiomyopathy // Circulation. - 2008. - Vol. 118. - P. 131-139.
10. Tikhomirova E.A. Criteria for predicting the course and outcome of hypertrophic cardiomyopathy in children: abstract of thesis. ... Ph.D. - M. - 2007. - 27 p.
11. Colan S., Lipshultz S., Lowe A. et. al. Epidemiology and cause-specific outcome of hypertrophic cardiomyopathy in children: findings from the Pediatric Cardiomyopathy Registry // Circulation. - 2007. - Vol. 115. - P. 773-781.
Enlarged heart in a child
As a rule, an enlarged heart is detected by chance during a routine examination and chest x-ray. The diagnosis of an enlarged heart, or cardiomegaly, shocks parents.
Cardiomegaly can be primary or secondary. Secondary cardiomegaly develops against the background of infectious diseases, toxic lesions, and also with respiratory failure. But the exact causes of primary cardiomegaly remain not fully known.
An enlarged heart is quite difficult to determine for a non-specialist, which is why parents are surprised by the diagnosis. And, indeed, the symptoms that accompany the disease are rapid heartbeat, rapid breathing, cyanosis of the nasolabial triangle, swelling, pale skin, and lack of appetite. Such symptoms can accompany various diseases, so it doesn’t even occur to many parents that their child has an enlarged heart.
Children's hearts beat much faster than adults'. If the beat frequency exceeds 160 beats per minute, then this is already an alarming sign. But, if parents cannot measure the heart rate themselves, then they can monitor the rhythm of breathing. With cardiomegaly, breathing not only becomes more frequent, but also the rhythm is disturbed, it becomes shallow with missed breaths.
Weak heart function provokes disturbances in the circulatory system, which causes pale skin and a bluish tint to the lips and nose. Swelling is also evidence that something in the body is not working as it should. When the heart fails to cope with its work, fluid from the blood vessels begins to accumulate in the tissues. Finally, lack of appetite is also an important sign of some disease. Many parents, unfortunately, do not always pay due attention to this symptom, especially when the child is always reluctant to eat.
With such signs, you need not only to see a pediatrician, but also to consult a cardiologist. Only experienced specialists can suspect heart problems. If you listen to the heart and the child has any side symptoms, the doctor will send you for an x-ray, which will show the size of the heart tissue. In addition, small changes can be detected on the cardiogram.
Cardiomegaly is usually discovered when a child is seen for deteriorating health. If the disease is not detected in time, it can even lead to dire consequences. That is why you should not neglect heart diagnostics.
If a child is nevertheless diagnosed with a heart pathology, then there is no need to panic ahead of time. The child needs to do a series of studies, during which complete information about the condition of the heart will be collected. Based on the data obtained, the cardiologist makes a diagnosis and prescribes adequate treatment. There is no need to neglect routine medical examinations, since treatment will be most effective when there are no secondary signs of the disease. And if noticeable symptoms appear, you should under no circumstances hesitate.
Heart disease in children: what parents should be wary of.
1. In 2021, 211 children died in physical education lessons. If you subtract vacations, holidays and weekends from 273 school days, it turns out that every day a child died in one of the Russian schools. From a medical point of view, sudden death in children can be caused by various reasons - both cardiological with the development of acute heart failure, and diseases of the central nervous system. Parents may not even know that their child has such a problem. However, everything can be diagnosed with a timely visit to a pediatric cardiologist.
2. According to the medical examination plan, at 1 year, then at 3 years (before kindergarten) and 6–7 years (before school), children must undergo a medical commission, which includes a cardiologist, who is obliged to refer the child for standard studies - EchoCG and ECG. EchoCG (or ultrasound of the heart) allows you to evaluate the functioning of the heart, its anatomical structure, the contractility of the ventricles, and measure the pressure in the cavities, which is necessary to exclude congenital and acquired anomalies of the heart and lungs. An ECG analyzes the functioning of the conduction system of the heart and identifies its disorders, including life-threatening ones. If a child is suspected of having an arrhythmia, the doctor will refer him for further examination - daily ECG monitoring and consultation with a pediatric arrhythmologist.
3. With some undiagnosed heart defects, tragedy can occur even with average physical exertion. But it’s even more dangerous when under-examined children, trying to earn points before admission, decide to pass the GTO standards, which require absolute health and serious preparedness. Therefore, doctors insist that before passing the GTO standards and competitions, children undergo a full cardiac examination (echocardiography, stress ECG, daily ECG monitoring) to exclude life-threatening disorders in the heart.
4. Often, after suffering from viral diseases, myocarditis (inflammation of the heart muscle) and inflammation of the blood vessels of the heart (aortitis, coronaritis) develop. This leads to a decrease in the contractility of the myocardium, disruption of its blood supply (including the conduction system of the heart), to the development of heart failure and life-threatening arrhythmias. Therefore, after recovering from a viral infection (especially a severe one), the child should be released from physical education for two weeks and must undergo an ECG.
5. The causes of fainting can be associated with both cardiac dysfunction (cardiac arrest, vegetative-vascular dystonia), and with pathology of the central nervous system (tumors, epilepsy), diseases of the endocrine system (hypoglycemia, diabetes mellitus), abnormal development of the spine (Kimmerle anomaly) etc.
6. The cardiovascular system of a rapidly growing child's body is extremely vulnerable. In adolescence, many children develop vegetative-vascular dystonia of the vagotonic type - a condition in which there is a tendency to hypotension. A sharp drop in blood pressure can lead to fainting, in which unsuccessful falls can cause fatal brain damage. Therefore, if a child complains of dizziness, headache, or periodically loses consciousness, be sure to consult a specialist and undergo the necessary examination.
7. Another problem is the special nutrition system that teenagers who are concerned about their figure choose. They eliminate fats from the diet and replace meals with protein shakes. However, the exclusion of one food component provokes the early and rapid development of atherosclerosis of the coronary arteries, leading to myocardial ischemia, the development of acute heart failure and sudden cardiac arrest.
8. There are many children who have had heart surgery at an early age. But they lead a normal life. They participate in sports clubs, as they say, without fanaticism, for their health. But to practice, they, like other children, need to get a certificate from a cardiologist.
9. What parents should be wary of:
- Blue discoloration of the nasolabial triangle and the area around the eyes is a sign of deterioration of venous outflow and insufficient blood oxygen saturation.
- Pain in the heart, shoulder blade, left arm.
- Persistent hypothermia is a low body temperature.
- Shortness of breath, which occurs due to blood stagnation and oxygen starvation.
- Cold palms and feet.
- Fatigue after physical activity - the child sits down, sighs, and complains of palpitations.
- Fainting.
10. It must be remembered that hypertension is rarely asymptomatic. Children complain of headaches, dizziness, weakness, fatigue, blurred vision or spots before their eyes. Children with hypertension often have sharply reduced vision. It is very important not to attribute these complaints to overwork, but to consult a doctor in time. The initial forms of childhood hypertension are corrected without medication. Results can be achieved if you normalize the child’s weight, daily routine (the student needs to get enough sleep, he should not get tired or overexcited) and nutrition. It is very important to choose suitable physical activity. The best results are achieved by cardio training (fast walking - 30-40 minutes daily, swimming, cross-country skiing, cycling).
11. But strength training for children with hypertension is absolutely contraindicated. If these measures do not produce results, medications are prescribed, the doses of which are selected individually and can only be discontinued by a doctor.
12. Most often, increased blood pressure worries children in adolescence (13–16 years). Blood pressure standards in children vary depending on age, weight (overweight children have higher blood pressure), height (short children have lower blood pressure) and gender (boys have higher blood pressure than girls). In children under 14 years of age, the average pressure should not exceed 120/80 mm Hg. Art., for older ones – 135/85 mm Hg. Art. Make an appointment with the cardiologist of the Children's Department, Anna Yuryevna Kozhina, by phone. 43-03-03 and 41-03-03 or