Journal "Medical Council" No. 17/2021
DOI:
10.21518/2079-701X-2021-17-294-299
I.N. Zakharova1, I.M. Osmanov2,3 I.I. Pshenichnikova1, T.M. Tvorogova1 I.N. Kholodova1, I.V. Berezhnaya1 E.V. Skorobogatova3, D.I. Kholodov4 T.A. Bocharova3, Yu.V. Koba1
1 Russian Medical Academy of Continuing Professional Education; 125993, Russia, Moscow, st. Barrikadnaya, 2/1, building 1 2 Russian National Research Medical University named after N.I. Pirogov; 117997, Russia, Moscow, st. Ostrovityanova, 1 3 Children's City Clinical Hospital named after Z.A. Bashlyaeva; 125373, Russia, Moscow, st. Geroev Panfilovtsev, 28 4 Children's city clinic No. 94; 125362, Russia, Moscow, st. Vishnevaya, 20, bldg. 2
Familial hypercholesterolemia is characterized by a significant increase in the concentration of low-density lipoprotein cholesterol in the blood serum, which, even in the absence of other risk factors, leads to the development of atherosclerotic vascular lesions starting in childhood. With a significant prevalence in the population, familial hypercholesterolemia is rarely diagnosed in a timely manner due to the long absence of clinical manifestations. An urgent task today is the development and implementation of programs for the primary detection of familial hypercholesterolemia in children and adolescents. Early identification of patients with familial hypercholesterolemia and timely initiation of adequate lipid-lowering therapy will curb the rate of progression of atherosclerosis, which will significantly reduce disability and mortality from cardiovascular diseases in older age groups. There are four types of screening: cascade, targeted, opportunistic and universal. Cascade screening
Today it is considered the most effective and cost-effective way to identify new patients with familial hypercholesterolemia among relatives of the index patient - a patient with an established diagnosis.
Targeted screening
is based on searching for individuals suffering from familial hypercholesterolemia among groups of patients with early development of atherosclerotic vascular lesions, for example, in cardiology or neurology hospitals.
Opportunistic screening
is an unsystematized, sporadic determination of cholesterol levels in patients seeking medical help for any reason.
The method is most applicable in primary health care institutions. Universal screening
is a mass examination of certain age groups and is a highly effective method of early diagnosis, especially in combination with reverse cascade screening of parents, siblings and other relatives of the index patient. The implementation of programs for early detection of familial hypercholesterolemia in childhood, the establishment of adequate patient routing systems, and the timely administration of effective lipid-lowering therapy will contribute to the preservation of health and the extension of working age, the development and preservation of the country’s labor potential.
For quotation:
Zakharova I.N., Osmanov I.M., Pshenichnikova I.I., Tvorogova T.M., Kholodova I.N., Berezhnaya I.V., Skorobogatova E.V., Kholodov D.I., Bocharova T. .A., Koba Yu.V.
Hypercholesterolemia in children and adolescents: focus on the family variant. Medical advice
. 2021;(17):294–299. https://doi.org/10.21518/2079-701X-2021-17-294-299.
Conflict of interest:
The authors declare no conflict of interest.
Hypercholesterolemia in children and adolescents: focus on the familial variant
Irina N. Zakharova1, Ismail M. Osmanov2,3 Irina I. Pshenichnikova1, Tatiana M. Tvorogova1 Irina N. Kholodova1, Irina V. Berezhnaya1 Ekaterina V. Skorobogatova3, Dmitri I. Kholodov4 Tatiana I. Bocharova3, Yuliya V. Koba1
1 Russian Medical Academy of Continuous Professional Education; 2/1, Bldg. 1, Barrikadnaya St., Moscow, 125993, Russia 2 Pirogov Russian National Research Medical University; 1, Ostrovityanov St., Moscow, 117997, Russia 3 Bashlyaeva City Children's Clinical Hospital; 28, Geroev Panfilovtsev St., Moscow, 125373, Russia 4 Children's City Clinic No. 94; 20, Bldg. 2, Vishnevaya St., Moscow, 125362, Russia
Familial hypercholesterolemia is characterized by a significant increase in serum low-density lipoprotein cholesterol concentration, which even in the absence of other risk factors leads to the development of atherosclerotic vascular lesions beginning in childhood. With significant prevalence in the population, familial hypercholesterolemia is rarely diagnosed in time due to the long absence of clinical manifestations. Today the urgent task is to develop and implement programs of primary detection of familial hypercholesterolemia in children and adolescents. Early detection of patients with familial hypercholesterolemia and timely initiation of adequate lipid-lowering therapy will curb the rate of atherosclerosis progression, which will significantly reduce disability and mortality from cardiovascular diseases in older age groups. There are four types of screening: cascade, targeted, opportunistic and universal. Cascade screening
is currently considered the most effective and cost-effective way to identify new patients with familial hypercholesterolemia among relatives of an index patient, the patient with the established diagnosis.
Targeted screening
is based on searching for individuals with familial hypercholesterolemia among groups of patients with the early development of atherosclerotic vascular lesions, for example, in cardiology or neurology hospitals.
Opportunistic screening
is a non-systematic, sporadic determination of cholesterol levels in patients seeking medical care for any reason.
It is most applicable in primary care health care settings. Universal screening
is a mass screening of certain age groups and is a highly effective way of early diagnosis, especially in combination with reverse cascade screening of parents, siblings, and other relatives of the index patient. Implementation of programs of early childhood detection of familial hypercholesterolemia, setting up systems of adequate routing of patients, timely prescription of effective lipid-lowering therapy will contribute to health preservation and prolongation of working age, development, and preservation of labor potential of the country.
For citation:
Zakharova IN, Osmanov IM, Pshenichnikova II, Tvorogova TM, Kholodova IN, Berezhnaya IV, Skorobogatova EV, Kholodov DI, Bocharova TI, Koba Yu.V.
Hypercholesterolemia in children and adolescents: focus on the familial variant. Meditsinskiy sovet = Medical Council
. 2021;(17):294–299. (In Russ.) https://doi.org/10.21518/2079-701X-2021-17-294-299.
Conflict of interest:
the authors declare no conflict of interest.
What is the cause of hypercholesterolemia?
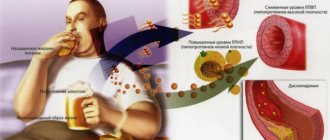
The most common cause of increased cholesterol levels is excess nutrition and a sedentary lifestyle. Modern man spends too few calories with a “full” diet. Hereditary predisposition plays a certain role.
In addition, hypercholesterolemia can be secondary and provoked by diseases such as:
- diabetes;
- decreased thyroid function (hypothyroidism);
- kidney damage in the form of nephrotic syndrome;
- liver dysfunction;
- genetic diseases (familial hypercholesterolemia).
Hypercholesterolemia can also occur while taking certain groups of pharmacological drugs.
These include:
- progestins;
- anabolic steroid;
- different types of immunosuppressants.
Risk factors for the development of hypercholesterolemia are:
- hereditary predisposition;
- excess body weight;
- low physical activity;
- chronic or acute stress.
Diagnostics
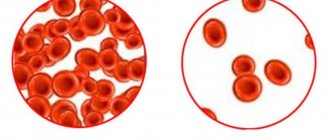
Laboratory hypercholesterolemia is detected by examining venous blood. In addition to the concentration of total cholesterol, the determination of its fractions and triglycerides is of great information. For differential diagnosis, the patient’s age and other anamnestic data are important - taking medications, the presence of close relatives with a confirmed familial form of hypercholesterolemia. To clarify the etiological factor, the following examination is carried out:
- Routine laboratory tests.
The content of liver transaminases (ALT, AST), markers of cholestasis (alkaline phosphatase, gamma-glutamyl transpeptidase), and glucose are measured. If nephrotic syndrome is suspected, a general urinalysis, analysis for microalbuminuria, and daily proteinuria are performed. - Hormonal studies.
The concentration of TSH and thyroid hormones (free T4 and T3) is determined. To confirm hypercortisolism, the level of cortisol in the blood is checked after performing small and large dexamethasone tests. - Immunological tests.
Tests are performed for markers of viral hepatitis (HBsAg, HCV), antimitochondrial (AMA), antineutrophil (ANCA) antibodies. - Ultrasound.
An ultrasound of the abdominal organs may reveal gall bladder stones, wall thickening, and signs of fatty infiltration in the liver. - Genetic research.
If hereditary hypercholesterolemia is suspected, mutations in the LDLR, PSCK-9, and ApoB-100 receptor genes are detected using the polymerase chain reaction.
For drug correction of hypercholesterolemia, different groups of drugs are prescribed
What can hypercholesterolemia lead to?
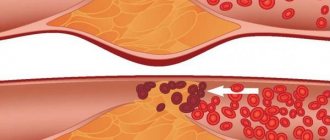
First of all, high cholesterol is the main factor in the development of atherosclerosis. Its deposits on the walls of blood vessels with the formation of atherosclerotic plaques pose a direct threat to all organs and systems of the patient.
Firstly, the lumen of the vessel itself narrows, which means that it begins to let in less and less blood, causing ischemia (oxygen starvation) of the organs that it supplies. The heart, kidneys and brain are primarily affected. The diameter of the vessels supplying these organs narrows due to the presence of atherosclerotic plaques, causing ischemia. With severe damage to the arteries of the legs, chronic insufficiency of blood supply develops, which can lead to the appearance of foci of necrosis and tissue ulceration.
Hypercholesterolemia leads to the formation of plaques in the wall of the largest vessel in our body - the aorta, leading to a loss of its elasticity and thickness. As a result, the wall is stretched under blood pressure and an aortic aneurysm occurs. And this, in turn, can lead to delamination or rupture, which is an extremely dangerous condition for the patient’s life.
Correction
Conservative therapy
If hypercholesterolemia is detected, it is imperative to consult a doctor to find out the cause of this laboratory phenomenon and select appropriate treatment. Much attention is paid to the fight against the underlying disease (immunosuppressive therapy for nephrotic syndrome, hormone replacement therapy for hypothyroidism, choleretic therapy for cholestasis), since its elimination can lead to normalization of cholesterol levels without additional intervention.
Non-drug methods for correcting hypercholesterolemia include complete smoking cessation and limiting alcohol consumption. Also, in order to reduce body weight, obese patients must follow a diet with a decrease in the proportion of animal fats in the diet (butter, fried meat, sausages) and an increase in vegetable fats (vegetables, seafood), fruits and whole grains, and regularly perform various physical exercises.
For the drug correction of hypercholesterolemia, the following drugs are used:
- Statins
(atorvastatin, rosuvastatin). The most effective and frequently prescribed means to reduce cholesterol levels. The mechanism of action is based on the suppression of cholesterol synthesis in the liver. - Fibrates
(clofibrate). These drugs stimulate the activity of the LPL enzyme, thereby accelerating the degradation of the drug. They reduce not only cholesterol, but also triglycerides, so they often become the drugs of choice for patients suffering from diabetes. - Ezetimibe
. Inhibits the absorption of cholesterol in the intestine. Used in combination with statins. - PCSK9 inhibitors
(alirocumab). These are monoclonal antibodies that bind to LDL receptors in the liver, which stimulates the breakdown of lipoproteins. Prescribed when statins are ineffective. - Bile acid sequestrants
(cholestyramine, colestipol). They are ion exchange resins that suppress the absorption of bile acids in the intestine. Depletion of FA reserves activates their synthesis from cholesterol in the liver. Used in patients with cholestasis. - A nicotinic acid
. This drug reduces the flow of fatty acids into the liver, which suppresses the synthesis of lipid. It has a weak hypocholesterolemic effect, therefore it is used as an addition to other drugs. - Omega-3 fatty acids
. Eicosapentaenoic acid and docosahexaenoic acid are components of fish oil. These substances bind to the nuclear PPAR receptors of liver cells, which leads to a decrease in serum lipid levels.
Surgery
One of the prerequisites for the effective treatment of hypercholesterolemia is normalization of body weight. For patients with morbid obesity (body mass index above 40), especially in combination with type 2 diabetes mellitus, if conservative methods are unsuccessful, bariatric surgery is indicated - gastric banding, gastric bypass or resection.
If hypercholesterolemia is caused by cholestasis due to cholelithiasis, surgical removal of the gallbladder (cholecystectomy) is performed. Patients with Cushing's disease undergo endoscopic transnasal adenomectomy (removal of the pituitary adenoma). For Itsenko-Cushing syndrome, bilateral adrenalectomy is used.
How to treat hypercholesterolemia?
The patient must be prescribed a diet low in fat and carbohydrates. As drug therapy, doctors at the CELT clinic use a wide range of lipid-lowering (lowering fat-lipid levels) agents. Their purpose, as well as the regimen of use, is selected individually and depends on the results of the examination of each individual patient.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
4.Treatment
In fact, the only way to medically influence the concentration of cholesterol in the blood (in the direction of reducing it) are drugs from the pharmacological group of statins. However, to date, extensive medical and statistical material has been accumulated, which reliably indicates, firstly, the insufficient effectiveness of these drugs (the so-called residual cardiovascular risk with such therapy remains at the level of 60-70%), and secondly, the unacceptably high likelihood of complications and side effects, incl. very heavy.
Therefore, one of the primary tasks of modern research medicine is the search and testing of alternative, more effective and safe ways to control the concentration of both total cholesterol and its individual fractions.
However, statins in any case play the role of ultima ratio (“last argument”), which should be resorted to only if there is no effect from all other measures. They always begin with examination and treatment of identified pathology, often latent or asymptomatic (chronic somatic diseases, endocrine-metabolic disorders, etc.), with the most serious correction of lifestyle and daily diet, cycle of rest and stress (physical and mental); with normalization of body mass index and categorical refusal of harmful habits.
With this approach, pharmacotherapy will most likely not be needed.
There is a misconception that atherosclerosis, caused by increased levels of low-density lipoproteins, mainly occurs in older people, as well as in patients with diabetes, obesity and other related pathologies. However, in Russia, 22% of girls and 24% of boys aged 15–19 years have high cholesterol levels. These people have a significantly higher risk of cardiovascular events (heart attacks, strokes, and more often there is a need for coronary artery bypass surgery), and at working age. Impaired lipid profile at a young age is most often caused by hereditary forms of dyslipidemia.
Familial hypercholesterolemia is a fairly common pathology throughout the world. That's why a Global Call to Action on the disease, written by EAS, together with the FH Study Collaboration and FH Europe, and in collaboration with the World Heart Federation (WHF), IAS and FH Foundation, was published in early 2021 in JAMA Cardiology. The purpose of this message is to draw the attention of the global medical community to the problem of familial hypercholesterolemia in order to prevent premature cardiovascular disease and mortality in patients with hereditary forms of dyslipidemia. Konovalov Gennady Aleksandrovich spoke about this
Doctor of Medical Sciences, Professor, Chairman of the Academic Council of the MEDSI Group of Companies, Head of the Center for Diagnostics and Innovative Medical Technologies of the MEDSI CDC on Belorusskaya.
Professor Konovalov acted as a moderator of the section “Family hypercholesterolemia and other disorders of fat metabolism” at the All-Russian online conference with international participation “Academy of Rare Diseases: from A to Z”. There he presented his report “Genetically determined forms of cholesterol metabolism disorders - clinical signs, diagnosis and modern therapy
", which was attended by more than 310 doctors in different cities of Russia and participants from other countries.
The professor noted that familial hypercholesterolemia is an urgent public health priority, since patients with this pathology are more likely to encounter cardiovascular diseases such as coronary heart disease, myocardial infarction, and aortic stenosis. Without prompt diagnosis and treatment, individuals with familial hypercholesterolemia have a 20-fold higher risk of cardiovascular disease and death.
The economic damage from this problem in our country in 2021 amounted to 1.29 trillion rubles per year, which is equivalent to 1.5% of GDP.
However, hereditary dyslipidemia is a disease whose course and outcome can be influenced by reducing possible risks both in terms of the duration and quality of life of a particular patient, and in economic terms.
“To do this, it is important to diagnose familial hypercholesterolemia in a timely manner, which in most cases does not require either expensive equipment or any special tests. The diagnosis is not difficult in the presence of several factors, such as elevated cholesterol levels in the patient and in his close relatives, an unfavorable family history under the age of 55, the presence of visible cholesterol deposits in the patient’s tissues (xanthomatoses, xanthelasmas, lipoid arch of the cornea),”
- said Gennady Alexandrovich.
Thus, already at the stage of examination and careful collection of anamnesis and evaluation of laboratory data, a diagnosis of familial hyperlipidemia can be established. However, in the vast majority of observations, a genetic test is not required.
In the world, artificial intelligence has already begun to be used to identify people with a hereditary form of dyslipidemia, when a computer, analyzing the electronic medical history, identifies the most typical signs of familial hypercholesterolemia with 80% confidence and transmits the list of patients to cardiologists to clarify the diagnosis.
Once the disease is confirmed, it is important to achieve the target level of atherogenic lipoproteins, at which atherosclerosis does not progress and, in some cases, reverses. This is precisely the main goal of preventing cardiovascular complications, both primary and recurrent.
To do this, it is necessary to determine the patient’s risk of complications of coronary artery disease. Thus, some people can be immediately classified as at high and/or very high cardiovascular risk. This is true for patients with familial hypercholesterolemia, as well as patients with documented cardiovascular disease, patients with diabetes mellitus, chronic kidney disease, the presence of atherosclerotic plaques in the carotid and femoral arteries, a coronary calcium index > 100, or extreme elevations in lipoprotein (a) levels.
The professor paid special attention to Lp(a), since an increase in this atherogenic and extremely thrombogenic lipoprotein leads to atherosclerosis of the vessels of the heart, brain, peripheral arteries and damage to the aortic valve. In other words, patients with initially elevated Lp(a) have a very high risk of developing coronary heart and brain disease, thrombosis, as well as destabilization of existing but inactive atherosclerotic plaques in patients with covid infection, which in turn can provoke acute myocardial infarction and stroke .
“For patients with an abnormal lipid profile in 2021, the European Atherosclerosis Society and the National Atherosclerosis Society of Russia have defined new target values for low-density lipoproteins: less than 1.4 mmol/L in the very high-risk group and less than 1.8 mmol/L in the high-risk group . For patients at extreme risk of complications (when, despite achieving target levels, atherosclerosis continues to progress), this figure should be less than 1 mmol/l,”
- noted the professor.
Achieving such a significant reduction in low-density lipoprotein cholesterol is often possible only with combination therapy, which includes modification of the patient’s lifestyle, the use of statins, and ezetemibe. If the effect is insufficient, PCSK9 inhibitors and the most effective method of therapeutic LDL and Lp(a) apheresis are used.
For some categories of patients with very high lipoprotein levels, it is important to add PCSK9 inhibitors to standard statin therapy immediately after diagnosis, since only this approach will reduce the level of low-density lipoproteins and Lp (a) to target values.
PCSK9 inhibitors have proven effective in a variety of patient populations, including high, very high, and extreme risk. They are indicated for patients with primary dyslipidemia, familial hypercholesterolemia, as well as patients with statin intolerance and diabetes mellitus. Moreover, this method is effective for hyper Lp (a) cholesterolemia, when other pharmacological drugs are not effective.
Treatment with PCSK9 inhibitors remains effective for a long time and leads to regression of atherosclerotic plaques. This method also works well with the use of LDL and Lp(a) apheresis.
“At the MEDSI Lipidology Clinic, we successfully use combination therapy. Every month we see 1500–1600 patients with dyslipidemia, of which about 25% have hyper Lp(a) cholesterolemia and 10% have other forms of familial dyslipidemia. Our experience at MEDSI shows that therapeutic lipid apheresis and pharmacotherapy to reduce Lp(a) levels can minimize the thrombogenic potential and proinflammatory effects in patients with covid infection,”
— Gennady Aleksandrovich shared his experience.
He noted that 80% of patients with combination therapy achieve the target level of low-density lipoproteins, 20% experience regression of atherosclerosis, and 80% of them stop the progression of atherosclerosis.