Blockage of arteries in the vertebrobasilar region leads to the development of ischemic stroke with localization of the infarction zone in various parts of the brain stem, thalamus, occipital lobes and cerebellum. Individual characteristics of the location of the arteries and the variety of pathogenetic mechanisms very often determine the individual characteristics of the neurological clinic in acute ischemic strokes in this area. Along with the presence of typical neurological syndromes, doctors at the Yusupov Hospital often note atypical symptoms of acute cerebrovascular accident. In this clinical situation, they use brain neuroimaging methods that help confirm the diagnosis (computed tomography and magnetic resonance imaging).
Neurologists at the Yusupov Hospital assess the degree of impairment of neurological functions during patient hospitalization, during treatment and at the end of therapy. All patients admitted to the neurology clinic undergo the following examinations:
- Doppler ultrasound of the great vessels of the head in the extracranial region;
- transcranial Doppler sonography;
- duplex scanning.
A 12-electrode ECG is also performed, blood pressure is monitored, and the volumetric maximum blood flow through the internal carotid and vertebral arteries is determined. Spiral computed tomography of the brain at the Yusupov Hospital is performed in all cases immediately upon admission of patients to the hospital. In the presence of several foci of cerebral infarction, neurologists use a more sensitive neuroimaging technique - diffusion-weighted magnetic resonance imaging.
A modern sensitive technique for neuroimaging of the brain - perfusion-weighted magnetic resonance imaging - allows doctors at the Yusupov Hospital to obtain information about the state of blood supply to brain tissue, and identifies blood supply disturbances both in the ischemic core zone and in surrounding areas.
Types of ischemic strokes in the vertebrobasilar region
The following ischemic cerebral infarctions in the vertebrobasilar region are distinguished:
- lacunar strokes due to damage to small perforating arteries, caused by microangiopathies against the background of arterial hypertension and diabetes mellitus;
- non-lacunar strokes that developed due to damage to the short or long circumflex branches of the vertebral and basilar arteries in the presence of sources of cardioembolism and the absence of narrowing of the large vertebrobasilar arteries;
- non-lacunar strokes due to blockage of the vertebral and basilar arteries in the intracranial and extracranial parts, caused by their damage.
They have different symptoms and require differentiated therapy.
Epidemiology
According to Russian literature, the share of VBI among all cerebrovascular accidents is about 25-30% and about 70% of TIA. In 60-70% of cases, VBI is associated with damage to the extracranial parts of the VA.
About 20-25% of all ischemic strokes develop in brain structures that receive blood supply from the arteries of the vertebrobasilar system.
Atherosclerotic lesion (mainly of the extracranial part) of the VA is the cause of ischemic cerebrovascular accidents in the VBB in 20% of cases. The annual risk of stroke in patients with intracranial VA or OA lesions is 8 and 11%, respectively.
The prevalence of spondylogenic PA syndrome (spondylogenic VBN) among all neurological diseases is 3.8% and for osteochondrosis of the cervical spine - 30-42.5%.
In case of injuries and damage to the cervical spine, according to foreign authors, structural and functional changes in the vertebral column occur in 19.7% - 33% of cases.
Symptoms of ischemic stroke in the vertebrobasilar region
Lacunar strokes in the vertebrobasilar region occur as a result of damage to a separate paramedian branch of the vertebral artery, common artery or branch of the posterior cerebral artery against the background of arterial hypertension, which is often combined with high levels of lipids in the blood or diabetes mellitus. The disease begins suddenly and is accompanied by dizziness, nausea, and vomiting. There are disturbances in motor function caused by damage to the motor pathways in the area of the base of the bridge, which are supplied with blood by small arteries branching from the main artery:
- incomplete paralysis of facial muscles;
- arm paralysis;
- impaired movement of the arm and leg on one side of the body.
Lacunar infarctions in the thalamus cause the development of a purely sensory syndrome, the cause of which is damage to the lateral parts of the thalamus due to blockage of the thalamogenicular artery. Complete hemisensory syndrome is manifested by a decrease in superficial or deep sensitivity, or numbness of the skin of one half of the body. Some patients have unilateral decrease in sensitivity of the corner of the mouth, palm and foot.
When ischemia spreads towards the internal capsule, a sensorimotor stroke develops. It is manifested by motor impairments, which are preceded by sensory disorders. If the lacunae are located in the area of the bridge, doctors at the Yusupov Hospital determine the following signs of ischemic stroke:
- impaired coordination of movements on one half of the body;
- moderate leg weakness;
- Mild paresis of the arm.
Nonlacunar ischemic infarction in the vertebrobasilar region develops as a result of damage to the short or long circumflex branches of the vertebral or basilar arteries and is manifested by the following symptoms:
- systemic dizziness;
- headache;
- hearing loss with noise in the same ear;
- motor and cerebellar disorders;
- sensory disturbances in one or both limbs of one side of the body.
Blockage of the posterior inferior cerebellar artery is manifested by the following symptoms:
- systemic dizziness;
- nausea;
- vomit;
- swallowing disorder;
- speech and hearing impairment;
- sensitivity disorders on the face of a segmental type;
- cerebellar ataxia (impaired stability) on the side of the ischemic lesion;
- movement disorders, decreased pain and temperature sensitivity on the limbs and torso on the opposite side.
When the branches of the main artery supplying the midbrain are blocked, paresis of the muscles innervated by the oculomotor nerve occurs on the side of the lesion and paralysis of the limbs on the opposite side. With a heart attack in the quadrigeminal artery basin, upward gaze paralysis and convergence insufficiency develop, which is combined with involuntary high-frequency oscillatory eye movements.
Cerebellar infarction in most cases occurs due to cardiac or arterial embolism of the anterior inferior cerebellar artery or superior cerebellar artery.
Blockage of the vertebral artery can occur both inside and outside the skull. When the extracranial section is blocked, the following symptoms are noted:
- short-term loss of consciousness;
- systemic dizziness;
- visual impairment;
- oculomotor and vestibular disorders;
- violations of statics and coordination of movements.
Often, patients suddenly fall, their muscle tone is impaired, autonomic disorders develop, breathing and cardiac activity are impaired.
Tactics for managing patients with VBI
TREATMENT of vertebrobasilar insufficiency
- 1. All patients with acute VBI, which corresponds to TIA, should be hospitalized in the neurovascular department of the hospital as soon as possible after the onset of clinical manifestations
- 2. All patients with chronic VBI (discirculatory encephalopathy) or spondylogenic VBN (vertebral artery syndrome) should be examined by a neurologist with further dynamic monitoring
Attention!
The information on the site does not constitute a medical diagnosis or a guide to action and
is intended for informational purposes only.
Treatment of ischemic stroke in the vertebrobasilar region
Neurologists at the Yusupov Hospital take an individual approach to the treatment of each patient diagnosed with ischemic stroke of the basilar artery. In the presence of high blood pressure, antihypertensive therapy is carried out. To stimulate spontaneous formation of channels in a blocked artery and prevent re-embolization in atherothrombotic and cardioembolic subtypes of nonlacunar ischemic infarction, direct anticoagulants, as well as antiplatelet agents, are used.
Complex therapy of acute ischemic strokes in the vertebrobasilar region also involves the prior use of neuroprotectors. In order to determine the feasibility of neuroprotective therapy, doctors at the Yusupov Hospital use diffusion-perfusion MRI studies, which help identify viable areas of the ischemic penumbra. After this, neuroprotective drugs are prescribed.
The Neurology Clinic of the Yusupov Hospital is equipped with the necessary equipment to diagnose complex locations of cerebral infarction. Neurologists treat patients with modern medications that have a pronounced effect on blockage of the vertebrobasilar artery. Call and they will make an appointment with a neurologist.
Causes of obstruction of blood flow from the brain
It is quite difficult to determine exactly what exactly provoked the disruption of the normal outflow of blood from the brain, because more than one year may pass after the event that provoked the blockage. The main causes of venous discirculation may be:
- pulmonary and heart failure;
- compression of extracranial veins;
- jugular vein thrombosis;
- brain tumors;
- traumatic brain injury;
- cerebral edema;
- systemic diseases (lupus erythematosus, Wegener's granulomatosis, Behcet's syndrome).
Discirculation can be provoked by either one disease or a complex of several unpleasant symptoms. For example, a mutation in the prothrombin protein in combination with the use of contraceptives in the form of pills increases the risk of developing dysgemia (another name for venous discirculation).
What does ignoring the problem lead to?
Ignoring symptoms for a long time results in oxygen and glucose not reaching the brain. This can lead to neurological problems. Lack of treatment can provoke more severe conditions.
Stroke
If any tumor blocks the flow of blood in the carotid artery, a heart attack or stroke may occur. As a result, some brain tissue may die. The death of even a small amount of tissue can affect speech, coordination, and memory. The severity of the consequences of a stroke depends on how much tissue has died and how quickly the outflow of venous blood has been restored. Some patients are able to fully recover, but most of those affected suffer irreversible changes.
Causes and mechanisms of stroke development
Stroke is a syndrome of acute cerebrovascular accident, which is characterized by the rapid onset of focal and/or cerebral symptoms that persist for more than 24 hours. General cerebral nonspecific symptoms include loss of consciousness, headache, dizziness, nausea and vomiting. The development of focal neurological deficit is associated with damage to a part of the brain that performs a particular function. Suddenly developed weakness in a separate limb or half of the body (paresis), up to complete immobilization (plegia), smoothness of the nasolabial fold, loss of speech and sensitivity are noted.
ACVA can be caused by spontaneous hemorrhage into the brain or under the meninges. In this case, we are talking about hemorrhagic stroke and subarachnoid hemorrhage, respectively. In another situation, a vascular accident develops as a result of a decrease in cerebral blood flow for various reasons, resulting in an ischemic stroke.
If hemorrhage occurs , then there is both a direct damaging effect of blood on brain cells, and indirect, due to compression of neighboring cells by the forming hematoma. A more complex mechanism develops during ischemia of brain tissue. Brain cells can only use glucose as an energy source, and can process it only with the required amount of oxygen.
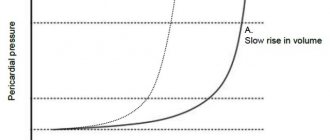
In conditions of insufficient blood circulation, oxygen starvation of neurons increases, glucose is converted into lactic acid, cell membranes are damaged, which ultimately leads to their death. Two zones are formed: the stroke core, containing dead cells, and the zone of the ischemic penumbra or penumbra, the neurons of which are in a depressed state, but have not yet died.
Prevention
To prevent the occurrence of manifestations of vertebrobasilar syndrome, a person predisposed to the development of such pathologies should adhere to certain rules, namely:
- practice proper nutrition, primarily limiting salt intake;
- do as much physical exercise as possible;
- spend more time outdoors;
- avoid stress and injury ;
- give up all bad habits;
- control blood pressure ;
- create comfortable conditions for work and sleep (in terms of body position);
- be periodically examined by a neurologist.
In order to prevent relapse after an attack of VBI, the patient must follow all the recommendations described above, as well as follow preventive therapy (antihypertensive, anticoagulant, antiplatelet, etc.) prescribed during the hospital stay.
Characteristics of VBB
The cerebral circulatory system , which provides a continuous supply of oxygen and nutrients to nerve cells, consists of 2 pools. 2/3 of the total blood volume enters the carotid system, internal carotid arteries and its branches. They form the Circle of Willis. This system nourishes the anterior and middle parts of the brain - the frontal, parietal, temporal lobes, thalamus, hypothalamus, structures of the limbic system.
1/3 of the volume enters through the vertebrobasilar system. It is formed from 2 vertebral arteries, the unpaired basilar artery and their branches.
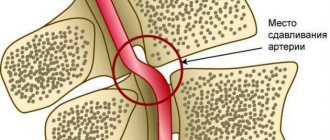
The vertebral arteries arise from the right and left subclavian arteries. They go in the bone canal formed by the transverse processes of the cervical vertebrae from the sixth to the second. Then they leave the canal, enter the cranial cavity and merge into the main artery.
The main, or basilar, artery lies on the anterior surface of the brain stem (pons). At the border of the pons and midbrain, it divides into 2 posterior cerebral arteries. The main branches of the vertebrobasilar system are the superior, inferior posterior, and inferior anterior cerebellar arteries. The VBB vessels supply blood to the brain stem (medulla oblongata, pons, midbrain), cerebellum (vermis and hemispheres), as well as the occipital lobe cortex.
Forecasts for venous discirculation
The prognosis and speed of recovery will depend on several factors.
For example, the survival prognosis for dysgemia may be quite negative if the patient has had a stroke or thrombosis. But if the cause of the disease is hypertension or diabetes, the prognosis will be much better.
Presence of hypoxia
The prognosis will be poor if venous discirculation previously led to hypoxia. Even after eliminating dysgemia, sudden loss of consciousness or problems with the musculoskeletal system are possible.
Most of all, the result of treatment will depend on the age and general health of the patient. Young people with good immunity have the best prognosis for a full recovery.
How to treat venous discirculation?
The doctor may recommend several different treatment methods, depending on the identified causes of the disease. But most patients will be advised to make changes to their daily lifestyle, namely:
- stop smoking and drinking alcohol;
- perform simple physical exercises daily;
- follow a diet to lower cholesterol levels;
- Monitor your blood sugar and blood pressure daily.
As for the drug treatment of patients with venous discirculation, specific therapy is prescribed, which includes taking anticoagulants or thrombolytics (depending on the medical history). But the use of systemic anticoagulation as primary treatment is recommended for all patients without exception (even for a child and in the presence of intracranial hemorrhage).
Drug therapy is the most effective method of treating dysgemia
Most often, drugs containing heparin are prescribed. When administered intravenously, its action begins immediately, which is very important for patients with acute dyshemia.
Enoxaparin sodium is a low molecular weight heparin and is prescribed if it is necessary to restore venous outflow to patients suffering from allergic reactions, or for prophylaxis. The main advantage of enoxaparin is the possibility of intermittent administration of the drug, which allows the patient not to go to the hospital, but to take advantage of outpatient treatment.
Warfarin is prescribed to patients with bleeding disorders for whom heparin and enoxaparin are strictly contraindicated. The drug has a slight effect on coagulation activity, but the therapeutic effect can only be seen after a few days. Therefore, such treatment is not prescribed in the acute stages of dyscirculation.
The dose of the administered drug must be carefully monitored by a doctor, so use at home is excluded. Higher doses are administered at the beginning of treatment in order to speed up the time to restore normal outflow, but at the same time, this tactic leads to an increased risk of bleeding. Treatment with warfarin should be continued for 3-6 months to obtain lasting results.
Surgical intervention to get rid of dyscirculation is prescribed in extreme cases
If the disturbances in the venous system are too severe, the doctor may recommend surgery to quickly improve the flow of blood from the brain. But surgery is prescribed only if medical methods do not work.
Types of surgical operations recommended for dysgemia:
- endarterectomy (removal of the inner lining of the affected artery);
- bypass surgery: a new blood vessel is placed near the narrowing of the vein to create a new route for blood flow;
- angioplasty: a balloon catheter is inserted into a narrow section of the artery to widen the walls and improve blood flow.
Part of the vascular system
The cardiovascular system is the main transport route, supplying all cells with oxygen and useful substances carried in the blood, as well as removing waste products for metabolism, utilization and excretion. It consists of three main types of vessels - arteries, veins and capillaries, and in some organs, specialists combine them into certain structures in order to characterize the pathology as accurately as possible, if necessary. One of these structures is the vertebrobasilar basin of the brain.