Doctors Cost
Price list Doctors clinic
Cerebrovascular accident (CVA) is a reduction in blood access to the brain. This is a real vascular catastrophe. The brain weighs approximately 2% of a person's body weight. A relatively small organ consumes 20% of all incoming energy. The brain does not accumulate the substances necessary for its activity. For normal functioning, it needs a continuous flow of glucose, oxygen, and some other elements supplied with the blood.
Cerebral circulation is distinguished by a multi-level system of redundant vessels and several regulatory mechanisms. But sometimes this is not enough. Cutting off blood supply to the brain for 10 seconds is enough to cause irreparable harm.
Causes of circulatory disorders in the brain
- Systolic pressure is less than 60 or more than 180 millimeters of mercury.
- Insufficient metabolic control, accompanied by unreasonable dilation of cerebral vessels.
- Atherosclerosis of cerebral vessels.
- Decreased blood oxygen saturation.
The compensatory capabilities of the brain are great. Vascular anastomoses allow blood to be distributed throughout the entire volume of the organ, even if the inflow through the left or right carotid artery is disrupted. However, these mechanisms do not work for long; after some time, oxygen starvation develops, and the first signs of the disease appear. This is why it is important to seek medical help immediately.
Most often, NMC develops against the background of:
- history of traumatic brain injury;
- chronic venous insufficiency;
- hypertension,
- atherosclerosis, ischemic heart disease,
- osteochondrosis,
- diabetes mellitus,
- hormonal imbalance,
- excess weight,
- stress, stress
- chronic fatigue,
- lipid metabolism failure,
- drinking alcohol,
- smoking.
How is placental circulation disrupted?
Poor blood flow associated with the placenta is called placental insufficiency. It can occur at any stage of pregnancy in two forms.
Acute appears suddenly, even during childbirth, and does not depend on the duration of pregnancy. The fetus falls into a state of hypoxia (oxygen deficiency), which threatens its death.
The main pathological mechanisms of this condition:
- premature placental abruption;
- heart attack due to thrombosis.
Chronic often complicates the course of pregnancy after 13 weeks. Symptoms appear in the third trimester. The mechanism of formation is early aging of the placenta due to the deposition of fibrin on the villi.
As a result of changes in the structure of chorionic villi (placental tissue), the functioning of the hematoplacental barrier ceases, metabolic processes between the maternal body and the fetus are disrupted
Negative consequences in such conditions, depending on the degree of violation, can lead to inevitable death of the fetus.
Acute cerebral circulatory disorders. Symptoms
According to the World Health Organization (WHO), 17 million people are diagnosed with stroke every year. Five million of them die, another 5 million remain disabled.
Table 2. Types of NMC
| NMK | Kinds | Development mechanism |
| Ischemic. | Cerebral infarction (ischemic stroke). | Stopping the blood supply to a part of the brain. |
| Transient NMC. | Lasts up to a day. | |
| Transient cerebrovascular ischemic attack. | Occurs periodically. | |
| Hemorrhagic. | Intracerebral hemorrhage. | Rupture of a vessel with subsequent effusion of blood into the brain tissue. |
| Subarachnoid hemorrhage. | Hemorrhage into the subarachnoid space. | |
| Non-purulent thromboembolism. | Thrombosis. | Blockage of a vessel by a thrombus. |
| Embolism. | Blocking of a vessel with an embolus. |
Types of chronic placental insufficiency
Depending on the development of consequences for the fetus and the ability of the mother’s body to adapt, 4 forms or stages of chronic placental insufficiency are distinguished:
- compensation - the mother’s body fully protects the fetus by improving blood flow through other pathways, and the child does not feel a lack of oxygen, develops normally, is born on time and develops well;
- subcompensation - the mother is not able to fully compensate for the lack of nutrition, and the fetus lags behind in development, there is a risk of complications and congenital defects;
- decompensation - accompanied by a complete disruption of the adaptation mechanisms, normal pregnancy is impossible, the fetus develops serious defects that are incompatible with viability, and death in utero is very likely;
- critical - due to severe changes in the structure of the placenta, further gestation of the fetus is impossible, inevitable death occurs, any treatment is ineffective.
Signs and symptoms of acute cerebrovascular accidents depending on the area of brain damage
- The basin of the internal carotid artery – paresthesia, paresis, paralysis on the opposite side of the face and body. Pathology of speech and vision in one eye.
- Vertebrobasilar basin - systemic dizziness, pain in the back of the head, unsteady gait, loss of visual fields, double vision, inability to swallow and speak.
- Brain stem - eye paralysis, hearing loss, swallowing and speech disorders, paresthesia of the facial skin.
- Medulla oblongata – bilateral paralysis.
- Temporal lobe – loss of spatial and temporal orientation, memory impairment.
What degrees of blood flow disturbance does placental insufficiency cause?
A comparison of clinical manifestations and ultrasound examination results made it possible to distinguish 3 degrees of blood flow disturbance between mother and fetus.
The first is characterized by minimal changes at the uteroplacental level, provides a “reserve” of time of about a month for treatment and full recovery without consequences, there are 2 types:
- Ia - only the uteroplacental blood flow is reduced, with the fetal-placental blood flow unchanged. It manifests itself as a delay in fetal development in 90% of cases.
- Ib - fetal-placental circulation suffers, but the uteroplacental circulation remains normal. Delayed formation and development of the fetus suffers somewhat less (in 80% of cases).
The conclusion is issued after examining all components of the fetal blood flow
The second is that the disorder occurs both at the level of the uterine and umbilical vessels; hypoxia can be fatal to the fetus.
Third, blood circulation indicators are at a critical level, and it is even possible that the direction of blood flow is reversed (reverse).
For clinicians, such a classification provides an opportunity to accurately determine the level of disorders and choose the most appropriate treatment tactics.
Diagnostics of NMC
- Duplex ultrasound examination of blood vessels.
- Contrast venography, angiography.
- CT, MRI.
- Transcranial Doppler.
- Laboratory tests - clinical, biochemical blood tests with determination of lipid profile, hematocrit.
- Fundus examination.
- Detection of hearing loss, smell, taste, and pathology of the vestibular apparatus.
Etiology of CNMK
There are many extracerebral causes leading to pathology of cerebral circulation. First of all, these are diseases accompanied by a disorder of systemic hemodynamics, leading to a chronic decrease in adequate blood supply - chronic cerebral hypoperfusion. The main reasons leading to chronic cerebral hypoperfusion include arterial hypertension (AH), atherosclerotic vascular damage, and heart disease accompanied by chronic heart failure. Other causes include diabetes mellitus, vasculitis in systemic connective tissue diseases, other diseases accompanied by vascular damage, blood diseases leading to changes in its rheology (erythremia, macroglobulinemia, cryoglobulinemia, etc.) [3–5].
Treatment
In case of acute cerebrovascular accident, treatment should be started immediately. The minutes count down.
For chronic pathology, the course of therapy is drawn up individually after diagnosis. The doctor takes into account age, concomitant diseases, and stage of the process.
Basic treatment includes, among other things, 3 mandatory recommendations.
- Nutrition correction. It should help normalize lipid metabolism and reduce blood cholesterol. Usually the consumption of meat, deli meats, and animal fats is limited. It is recommended to eat more vegetables, herbs, and dairy products.
- Increased physical activity. Helps normalize blood flow and increase vascular tone.
- Weight loss. Correcting your diet and increasing physical activity usually helps you lose extra pounds and be in good physical shape. If this is not enough, seek the help of an endocrinologist.
In case of cerebrovascular accident, with various symptoms, treatment is prescribed:
- physiotherapy;
- physical therapy;
- medicines;
- surgical treatment.
Structure of the uteroplacental blood flow
Mother and child are connected not only by the placenta, but also by a complex system of blood vessels. Therefore, all joint blood circulation is usually divided into levels that cannot exist in isolation, but work only in combination.
- The central part of the system is the placenta. It ensures the “absorption” of products from the maternal blood through the villi that have grown deep into the wall of the uterus. At the same time, the blood of mother and child does not mix. Several rows of special cells form a hematoplacental barrier, which is a serious obstacle to substances unnecessary for the fetus. Through it, the waste blood returns to the mother's venous system.
- The second part of the blood flow consists of the branches of the uterine arteries. If before pregnancy in the female body they are in a collapsed state and are called spiral, then from the period of 1 month they lose the muscle layer that can cause spasm. And by four months, the arteries transform into full-fledged trunks, filled with blood and heading to the placenta area. It is this mechanism, useful for feeding the fetus, that can turn out to be fatal during uterine bleeding: the walls of the vessels can no longer contract.
- The vessels in the umbilical cord form the third pathway of blood flow. There are 2 arteries and a vein here. They connect the baby with the placenta and form the fetal-placental circle. Reduced blood flow at this level causes the most severe damage to the fetus.
Prevention
To avoid the sudden appearance of cerebrovascular accidents, you need to lead an active lifestyle. Do as much physical activity as possible, morning exercises. Walk more, swim, take a contrast shower. Be sure to monitor blood pressure.
You should stop smoking and drinking alcoholic beverages.
It is recommended to consume more foods rich in vitamins C, D, E, and fiber. Minimize the intake of fried, fatty, spicy, salty foods. If you have chronic diseases, they must be treated. If you have hypertension, monitor your blood pressure.
What to do to prevent blood flow disorders?
Gynecologists urge women at risk to prepare themselves for pregnancy in advance and prevent unplanned conception.
Choosing the right body position while sleeping helps fetal blood flow
If you are already pregnant, it is recommended:
- avoid emotional and physical overload;
- eliminate bad habits;
- organize nutritious meals for the pregnant woman;
- monitor daily walks and stay in a ventilated room;
- do special gymnastics for pregnant women, yoga exercises;
- control body weight, carry out monthly weighing and measurement of abdominal circumference;
- It is considered more beneficial to sleep on the left side; this position reduces pressure on the inferior vena cava, which runs to the right of the uterus, but in some cases, with stagnation in the kidneys, sleeping on the right side improves the outflow from these important organs.
Modern diagnostic methods and approaches to the management of pregnant women make it possible to prevent severe disorders. However, many possibilities depend on the woman herself and her desire to have a healthy heir.
Clinical manifestations of CNM
The main clinical manifestations of CNM are disturbances in the emotional sphere, balance and gait disorders, pseudobulbar disorders, impairment of memory and learning ability, neurogenic urination disorders, which gradually lead to maladjustment of patients [1].
During CNM, three stages can be distinguished [10, 11]:
At stage I, the clinic is dominated by subjective disorders in the form of general weakness and fatigue, emotional lability, sleep disturbances, decreased memory and attention, and headaches. Neurological symptoms do not form distinct neurological syndromes, but are represented by anisoreflexia, discoordination, and symptoms of oral automatism. Violations of memory, praxis and gnosis can be identified, as a rule, only when special tests are carried out.
At stage II, there are more subjective complaints, and neurological symptoms can already be divided into distinct syndromes (pyramidal, discoordination, amyostatic, dysmnestic), and one neurological syndrome usually dominates. The professional and social adaptation of patients decreases.
At stage III, neurological symptoms increase, a distinct pseudobulbar syndrome appears, and sometimes paroxysmal conditions (including epileptic seizures); Severe cognitive impairment leads to disruption of social and everyday adaptation and complete loss of working capacity. Ultimately, CNM contributes to the formation of vascular dementia [4].
Cognitive impairment is a key manifestation of CNM, which largely determines the severity of the patient’s condition. They often serve as the most important diagnostic criterion for CNM and are a sensitive marker for assessing the dynamics of the disease. It is worth noting that the location and extent of vascular changes detected by MRI or computed tomography are only partially correlated with the presence, type and severity of neuropsychological findings. In CNMC, there is a more pronounced correlation between the severity of cognitive impairment and the degree of brain atrophy [20, 21]. Correcting cognitive impairment is often critical to improving the quality of life of the patient and his relatives.
Syndrome of blood flow insufficiency in the arteries of the vertebrobasilar system
Maksimova M.Yu., Piradov M.A. RMJ. 2021. No. 7. pp. 4-8 The article is devoted to the problem of blood flow insufficiency syndrome in the arteries of the vertebrobasilar system. Methods for diagnosing and treating vertebrobasilar insufficiency are presented, which should be aimed at preventing its progression, improving blood supply to the brain, and correcting certain syndromes and symptoms.
The independent clinical concept of “blood flow insufficiency syndrome in the arteries of the vertebrobasilar system” was formed in the 1950s, during the period of revision of views on the pathogenesis of ischemic cerebrovascular accidents (CVA) and the emergence of the concept of the leading role of cerebrovascular insufficiency in this case [1]. The peculiarities of the structure and functions of this arterial system, which provides nutrition to vital structures of the brain, and the uniqueness of clinical symptoms in case of disturbances of blood flow in it led to its identification in the latest version of the international classification into an independent symptom complex - “vertebrobasilar arterial system syndrome” within the framework of “transient transient cerebral ischemic attacks (attacks) and related syndromes” (International Classification of Diseases, 10th Revision, G45.0). Even earlier, a group of experts from the World Health Organization defined “vertebrobasilar insufficiency” as “a reversible impairment of brain function caused by a decrease in the blood supply to the area supplied by the vertebral and basilar arteries.” The ischemic nature and reversible nature of the disorders were emphasized, but the duration of neurological symptoms was not indicated, which previously did not allow them to be classified as transient ischemic attacks (TIA) and which has now become possible. Blood flow disturbances in the arteries of the vertebrobasilar system account for about 70% of all TIAs. Stroke with localization of focal changes in areas of the brain that receive blood through the arteries of this system develops 2.5 times less frequently than in regions belonging to the arterial basins of the carotid system [1].
Causes of blood flow insufficiency syndrome in the arteries of the vertebrobasilar system
The main causes of blood flow insufficiency syndrome in the arteries of the vertebrobasilar system, caused by arterial hypertension (AH) and atherosclerosis (AS), include [1, 2]:
- atherostenosis or atherobliteration of one of the vertebral arteries;
- characteristic arterial tortuosity, which in some cases can lead to kinking of the vertebral artery with the formation of septal stenosis and disruption of blood flow in it;
- congenital anomalies of the vertebral arteries (hypoplasia of one of the vertebral arteries, lateral displacement of the mouth of the vertebral artery), in which the insufficiency of blood flow in one of the vertebral arteries is compensated by another vertebral artery, but decompensation occurs against the background of AS and hypertension;
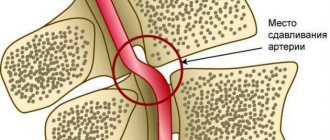
- compression of the vertebral artery by an osteophyte in the bone canal of the cervical spine, an articular process with instability of the cervical spine, an accessory cervical rib, a spasmodic neck muscle (posterior scalene muscle, longus colli muscle, inferior oblique muscle of the capitis), which is most often observed with congenital abnormally high entry vertebral artery into the spinal canal - at the level of 3–5 cervical vertebrae.
The syndrome of blood flow insufficiency in the arteries of the vertebrobasilar system can also be observed:
- with subclavian “steal syndrome”, in which, as a result of occlusion of the subclavian artery, blood flows not only to the entire vertebrobasilar system, but also to the arm through only one vertebral artery;
- with occlusion or severe atherostenosis of both internal carotid arteries
(ICA), since the vertebrobasilar system plays a significant role in the blood supply to the cerebral hemispheres and, under certain conditions, “steal syndrome” may occur; - with disturbances of general hemodynamics.
Subclavian “steal syndrome” is characterized by a phenomenon when a patient, during intensive work of the arm (retrogradely supplied with blood from the contralateral vertebral artery), experiences brainstem symptoms - most often dizziness. A certain contribution to the development of blood flow deficiency syndrome in the vertebrobasilar system can be made by changes in the rheological properties of blood (increased levels of fibrinogen, blood viscosity, platelet aggregation and hematocrit, increased rigidity of erythrocytes), leading to deterioration of microcirculation.
Diagnosis of blood flow insufficiency in the arteries of the vertebrobasilar system
Subjective data
The diagnosis of insufficiency of blood flow in the arteries of the vertebrobasilar system is based on a characteristic symptom complex that combines several groups of clinical symptoms found in patients with AS and hypertension.
These are visual and oculomotor disorders, disorders of statics and coordination of movements, vestibular disorders. In this case, the presumptive diagnosis is determined on the basis of at least two of these symptoms. They are short-lived and often go away on their own, although they are a sign of impaired blood flow in the arteries of this system, which requires clinical and instrumental examination. A thorough medical history is especially necessary to clarify the circumstances of the occurrence of certain symptoms [1, 2]. Visual disturbances
include a feeling of blurred vision, photopsia, scotoma, changes in visual fields, decreased visual acuity and are associated with transient ischemia of the occipital lobes of the brain.
Blurred vision in the form of a veil before the eyes and blurred vision often occurs at the height of a headache. Photopsia appear in the form of flashes of colored dots, most often red or green, black, with a light halo, as well as spots, fiery lightning, lines, rings, zigzags. Photopsia differ from the rainbow circles characteristic of glaucoma in that their appearance is not associated with an external light source; they also occur with closed eyes. Changes in visual fields are usually observed in the form of their concentric narrowing. Decreased visual acuity often develops after the onset of headache and progresses; vision deteriorates noticeably during headache attacks and after them. Oculomotor disorders
manifest themselves in the form of transient diplopia with mild paresis of the eye muscles and impaired convergence.
In most patients, these disorders are among the initial manifestations of the disease, and in a quarter of them they serve as one of the main complaints with vertebrobasilar insufficiency. Static and dynamic ataxia are also among the permanent symptoms that are manifested by patient complaints of instability and staggering when walking and standing. Coordination of movements is significantly less impaired; a persistent change occurs, as a rule, with cerebellar infarctions. Vestibular disorders
manifest themselves in the form of sudden dizziness - systemic, which is characterized by a feeling of “rotation of objects”, “an inverted room”, and non-systemic with a feeling of “motion sickness”, nausea, and less often vomiting.
Spontaneous nystagmus is also detected, sometimes only after special tests with turning the head to the side and fixing it in these positions (De Klein test). The development of dizziness is associated with ischemia of either the vestibulocochlear organ or the vestibular nuclei and their connections. The vestibular nuclei are most sensitive to ischemia and hypoxia. In this case, dizziness as a monosymptom can be regarded as a sign of impaired blood flow in the arteries of the vertebrobasilar system only in combination with other signs of its impairment in patients with a relatively persistent otoneurological symptom complex. Less known, although not uncommon, are optic-vestibular disorders. These include symptoms of “shading shadow” and “convergent vertigo,” in which patients experience dizziness or unsteadiness when flashing light and shadow or when looking downward. Characteristic symptoms are attacks of sudden falling
without loss of consciousness (“drop attacks”), usually occurring during sudden turns or throwing back the head.
Syncopal vertebral Unterharnscheidt syndrome has been described, in which loss of consciousness and muscle hypotonia are observed in the absence of evidence of epilepsy and other paroxysmal conditions. Manifestations of diencephalic
disorders include severe general weakness, irresistible drowsiness, disturbances in the rhythm of sleep and wakefulness, as well as various autonomic-visceral disorders, a sudden increase in blood pressure (BP), and heart rhythm disturbances.
These disorders are associated with ischemia of the structures of the reticular formation of the brain stem. The described symptom complex has now been supplemented by other signs, which, in combination with them, also make it possible to judge the insufficiency of blood flow in the arteries of the vertebrobasilar system. At various stages of vertebrobasilar insufficiency, patients often complain of decreased memory
(“forgetfulness”), concentration disorders and instability of active attention. Most often, memory for names, numbers, and recently occurring events decreases. The ability to memorize new material decreases, it becomes more difficult to retain what has been read in memory, what is planned for implementation is forgotten, and the need to write it down arises. It becomes difficult for patients to comprehend a large amount of information, which leads to a certain decrease in performance and limitation of creative possibilities in people engaged in mental work. At the same time, professional memory and memory of past events are preserved. This applies more to RAM than to logical memory. Often, a decrease in memory and performance is regarded by others as a result of overwork, and not as a manifestation of cerebral vascular insufficiency. During neuropsychological research, the preservation of the level of generalization, the correspondence of judgments to the general educational and cultural level, and the preservation of the stock of ideas and skills are noted. Impaired cognitive functions significantly reduce the quality of life and also affect the progression of cerebrovascular insufficiency. Decreased memory for current events in patients with vertebrobasilar insufficiency is associated with chronic ischemia of the medial parts of the temporal lobes, primarily the hippocampus and mammillary bodies. With vertebrobasilar insufficiency, attacks of transient global ischemia are also observed, during which working memory (the ability to remember new information) is impaired for several hours. The patient looks absent-minded, he is disoriented in space and time, sometimes excited, persistently tries to find out from those around him where he is, how he got here, but being unable to remember the answers, he constantly asks the same questions. With the return of the ability to remember, orientation is also restored, only the episode itself is amnesic. Acute amnesia can also be caused by acute cerebrovascular accident in the basins of both posterior cerebral arteries. In this case, amnesia may be accompanied by limitation of visual fields (unilateral or bilateral hemianopia), visual agnosia, alexia, amnestic aphasia, and sensory impairment. The combination of a number of characteristic symptoms makes it possible to diagnose the syndrome of blood flow insufficiency in the arteries of the vertebrobasilar system, although in this case only the ischemic nature of the cerebrovascular accident and the localization of the source of ischemia are determined, and not the reasons that determined this nature.
Objective data
The most accessible and safest methods for determining insufficiency of blood flow in the arteries of the vertebrobasilar system are neurological examination and ultrasound methods of studying the vascular system of the brain.
Among the objective signs revealed during a neurological examination
, one should first of all mention nystagmus, static and dynamic ataxia.
In the Romberg test, the patient deviates to the side. Walking with eyes closed reveals unsteadiness and persistent deviation to one side in a patient with insufficient blood flow in the vertebrobasilar system. When performing the Unterberger test, the patient is asked to march in one place with his eyes closed for 1–3 minutes. Normally, it remains in place or moves slightly relative to the starting point or rotates slightly around its axis. A forward shift of more than 1 m and a rotation of more than 40–60° (after 50 steps in place) are considered pathological. The results of the Babinski-Weil test (“star test”) are interpreted in a similar way. With eyes closed, the patient is asked to take two steps forward, turn 180° and take two steps back. Any deviations to the side or rotation indicate dysfunction of the vestibular labyrinth. If the patient is asked to walk in the forward and reverse directions several times, then as a result of a deviation to one side, the trajectory of his movement resembles the outline of a star (hence the name of the test). It is also necessary to measure blood pressure in both arms in a sitting and lying position. Objective signs of the syndrome include differences in pulse and blood pressure in the arms and noise in the supraclavicular region. With a significant decrease in systolic blood pressure (more than 20 mm Hg) in an upright position, symptoms reminiscent of insufficiency of blood flow in the vertebrobasilar system should be attributed to orthostatic hypotension. Subclavian “steal syndrome” is characterized by a phenomenon when a patient, against the background of intense hand work, develops brainstem symptoms—usually dizziness. Doppler ultrasound
allows you to obtain data on blood flow in the vertebral arteries, linear speed and direction of blood flow in them.
Compression-functional tests make it possible to assess the condition and resources of collateral circulation, blood flow in the carotid, temporal, supratrochlear and other arteries. Duplex scanning allows you to determine the condition of the artery wall, the structure and surface of atherosclerotic plaques that stenose these arteries. Transcranial Doppler ultrasound with pharmacological tests is important for determining cerebral hemodynamic reserve. Data on the condition of the great arteries of the head (MAG) and intracerebral arteries obtained from CT and MRI angiography are extremely informative. X-rays
of the cervical spine can provide information about the condition of the structures around the vertebral arteries and the effect of these structures on the vertebral arteries and the blood flow in them;
functional tests are used in this case. A special place among instrumental methods is occupied by otoneurological research
, especially if it is supported by electronystagmographic and electrophysiological data on auditory evoked potentials characterizing the state of brain stem structures, as well as MRI of these structures. The algorithm for using the listed instrumental research methods is determined by the logic of constructing a clinical diagnosis.
Treatment of vertebrobasilar insufficiency
Treatment of vertebrobasilar insufficiency is aimed at preventing its progression, improving blood supply to the brain, and correcting individual syndromes and symptoms.
The most effective measures in this direction are the elimination or correction of the main risk factors
for the development of vertebrobasilar insufficiency, which include smoking, hyperlipidemia, AS of the cerebral arteries, hypertension, diabetes mellitus, obesity, heart disease, disorders of the rheological properties of the blood, psycho-emotional stress, alcohol abuse [3 ].
A large place in the prevention of the progression of vertebrobasilar insufficiency is occupied by recreational activities, climate therapy at local resorts, in low-altitude conditions, at sea resorts, balneotherapy (radon, brine, carbon dioxide, sulfide, iodine-bromine baths). Moderate physical activity (therapeutic exercises, walking, swimming) and regular mental exercise are needed. The diet
should not be burdensome for the patient (do not overeat, limit the consumption of animal fats, easily digestible carbohydrates and foods rich in cholesterol, reduce the total calorie content of food, introduce fresh vegetables and fruits, wholemeal products, fish products into the diet).
Smoking is excluded and alcohol consumption is limited. When treating vertebrobasilar insufficiency, the following measures should be taken: early detection; determination of the severity of clinical symptoms; exclusion or correction of the main risk factors for the development of cardiovascular diseases; dynamic observation; timely initiation of treatment; its duration and continuity; treatment of concomitant somatic, neurological and mental disorders; medical, professional and social rehabilitation. Methods of drug treatment
of chronic musculoskeletal disorders include: antihypertensive therapy, the use of lipid-lowering drugs, improving blood supply to the brain using antithrombotic drugs, neuroprotective therapy [3, 4].
One of the most promising neuroprotective drugs from the perspective of evidence-based medicine is citicoline
[4, 5].
Citicoline, a natural endogenous compound also known as cytidine-5'-diphosphocholine (CDP-choline), is a mononucleotide consisting of ribose, cytosine, pyrophosphate and choline. When taken orally, citicoline is rapidly absorbed and hydrolyzed into choline and cytidine in the intestinal wall and liver. These substances enter the systemic circulation, pass through the blood-brain barrier and recombine to form citicoline within the central nervous system [6]. Phosphatidylcholine in brain cell membranes is broken down into fatty acids and free radicals by phospholipases under ischemic conditions. By restoring the activity of Na+/K+-ATPase of the cell membrane, reducing the activity of phospholipase A2 and participating in the synthesis of phosphatidylcholine, the membrane-stabilizing effect of citicoline is realized. In addition, citicoline affects the formation of free fatty acids, the synthesis of acetylcholine and an increase in the content of norepinephrine and dopamine in nervous tissue. Citicoline is also able to inhibit glutamate-induced apoptosis and enhance neuroplasticity mechanisms [7]. The first studies of citicoline, conducted at the end of the twentieth century, concerned patients with vascular dementia. Thus, R. Lozano et al. (1986) observed 2067 elderly patients treated in geriatric psychiatry departments and found a positive effect of a 2-month course of citicoline therapy on the severity of neuropsychological symptoms [8]. In a study by B. Chandra (1992), assessing the effectiveness of the drug in 146 patients with vascular dementia, it was demonstrated that therapy with citicoline at a dose of 750 mg/day IV for 2 months. led to a significant improvement in cognitive function scores (assessed on the MMSE scale) compared to placebo. Moreover, the effect of therapy was maintained after 10 months. after completion of treatment [9]. In 2005, a Cochrane review of the effectiveness of citicoline in the treatment of cognitive and behavioral impairment due to chronic cerebrovascular insufficiency in elderly patients was published [10]. The review included the results of 14 randomized placebo-controlled trials involving 1336 patients. The average dose of citicoline in these studies was 1000 mg/day, the duration of treatment was 3 months. The effectiveness of treatment was assessed using tests for memory, attention, and behavior. The review demonstrated the positive effect of citicoline on behavioral disorders, as well as improving memory. The only significant limitation of this review was the short duration of the included clinical studies. In subsequent years, researchers focused on studying the drug's effectiveness in patients with mild cognitive impairment (MCI) and post-stroke cognitive impairment. Thus, according to M. V. Putilina (2009), already at the initial stages of manifestations of cognitive impairment in patients with chronic cerebrovascular insufficiency, the use of citicoline (at a dosage of 1000 mg IM or IV for 10 days followed by oral administration in the form of a solution for oral administration for 3 months) contributes to the regression of these disorders. In addition, the drug has a positive effect on concomitant emotional, affective and behavioral disorders in this group of patients [11]. In 2013, the results of two controlled studies evaluating the effect of the drug on cognitive function in patients with chronic cerebrovascular diseases were published. In a placebo-controlled study, L. Alvarez-Sabin et al. (2013) took part in 347 elderly patients (mean age 67.2±11.3 years) who had suffered a stroke and had cognitive impairment. In the active treatment group (172 patients), citicoline was prescribed at a dose of 2000 mg/day per os for 6 months, then 1000 mg/day for another 6 months. The criteria for the effectiveness of treatment were the results of a neuropsychological examination (a battery of tests for memory, attention, executive (regulatory) functions, time orientation), as well as an assessment of clinical outcomes using the modified Rankin Scale after 6 and 12 months. after starting treatment. Long-term therapy with citicoline resulted in a slowdown in the progression of cognitive impairment and better functional recovery (compared to placebo) due to improved attention, regulatory functions, and time orientation [12]. The IDEALE study assessed the effectiveness of citicoline in the long-term treatment of vascular MCI in elderly patients. 349 patients with MCI of predominantly vascular origin were prescribed citicoline (265 patients) at a dose of 1000 mg/day per os for 9 months. or placebo (84 patients). Treatment with citicoline had no effect on measures of functional daily activities compared with placebo. At the same time, during treatment with citicoline, there was a positive dynamics of cognitive functions when assessed on the MMSE scale (improvement after 9 months by an average of 0.5 points); in the placebo group, progression of cognitive impairment was observed (after 9 months - worsening by an average of 1.9 points) (p=0.0001). Thus, long-term therapy with citicoline is associated with a decrease in the rate of progression of cognitive impairment in patients with vascular MCI [13]. Recently, new generic dosage forms have been widely introduced into practice. Among them is the domestic drug Neypilept
. The drug is produced from the Japanese substance of the KYOWA company in the form of a solution of 125 and 250 mg/ml for IV and IM administration, as well as two oral forms - an oral solution of 100 mg/ml in bottles of 30 ml and 100 ml. The volume of the 100 ml bottle corresponds to the sachet form of the original drug. As part of post-registration multicenter randomized studies, Neypilept was compared with the original drug in 152 patients in the acute period of ischemic stroke in the carotid system (RCT No. 396 of June 24, 2013) [14] and the effectiveness and safety of its oral form was studied in 128 patients with cognitive impairment (RCT No. 145 dated March 26, 2015) [15]. The results of the studies demonstrated the tolerability and effectiveness of Neypilept in these conditions comparable to the original drug [16, 17].
Conclusion
It should be emphasized that timely and systematic treatment can prevent the progression of cerebrovascular insufficiency and significantly improve the quality of life of patients. The adequacy and effectiveness of taking citicoline (Neipilept) is of particular importance. Adequacy of therapy implies a course of taking the drug, as well as cooperation between the patient and the attending physician in prescribing and carrying out treatment, the goals of which are to preserve the ability to work and maintain the patient’s quality of life. The following areas for assessing the effectiveness of treatment for vertebrobasilar insufficiency can be recommended (as early as 6–12 months from the start of treatment): reduction or disappearance of cerebral complaints, improvement of cognitive functions (primarily memory).
The original article was published on the RMJ website (Russian Medical Journal): https://www.rmj.ru/articles/nevrologiya/Sindrom_nedostatochnosti_krovotoka_varteriyah_vertebrobazilyarnoy_sistemy/#ixzz5NyXkC9vV
Appointment form...
Methods for diagnosing cognitive impairment
To assess the overall severity of cognitive defect, the Mini-Mental State Examination scale is most widely used. However, this method is not an ideal screening tool, since its results are significantly influenced by the patient's premorbid level and type of dementia (the scale is less sensitive to frontal cortex dysfunction and therefore better detects the early stages of Alzheimer's disease than the early stages of vascular dementia). In addition, its implementation requires more than 10–12 minutes, which the doctor does not always have at an outpatient appointment.
Levin O.S. et al. [22] recommend for a screening study a set of three simple neuropsychological tests, the completion of which requires about 5–6 minutes:
Clock drawing test: subjects are asked to draw a clock with its hands pointing to a specific time. Normally, the subject draws a circle, places the numbers from 1 to 12 inside it in the correct order at equal intervals, draws 2 hands (the hour hand is shorter, the minute hand is longer), starting in the center and showing the specified time. Any deviation from correct test performance is a sign of fairly severe cognitive dysfunction.
Speech activity test: subjects are asked to name as many names of plants or animals as possible in a minute (semantically mediated associations) and words starting with a certain letter, for example “l” (phonetically mediated associations). Normally, most elderly people with secondary and higher education name from 15 to 22 plants and from 12 to 16 words starting with “l” per minute. Naming fewer than 12 semantically mediated associations and fewer than 10 phonetically mediated associations usually indicates significant cognitive dysfunction. Visual memory test: patients are asked to remember 10–12 images of simple, easily recognizable objects presented on one sheet; Subsequently, the following are assessed: 1) immediate reproduction, 2) delayed reproduction after interference (a verbal association test can be used as an interfering effect), 3) recognition (the patient is asked to recognize previously presented objects among other images). Failure to remember more than half of previously presented images may be considered a sign of severe cognitive dysfunction.