Hypercholesterolemia is a disease in which the level of cholesterol in the blood rises to pathological levels. From the point of view of normal physiology, this compound is important and useful. Normally, most of it is produced by the body (up to 80%). Cholesterol ensures the stability of cell membranes and is involved in the synthesis of vitamins, bile acids, and hormones. However, with hypercholesterolemia, its level increases, it is deposited on the walls of blood vessels, affects metabolic processes and leads to the development of serious complications, including heart attack, stroke, hypertension, etc.
Classification
Most often in clinical practice, the Frederickson classification of hypercholesterolemia is used, which is based on the division according to the predominance of one or another cholesterol fraction:
- Type I – increased concentration of chylomicrons (CM).
- Type IIa – increased levels of low-density lipoproteins (LDL).
- Type IIb – high content of low and very low density lipoproteins (VLDL and LDL).
- Type III – increased levels of intermediate density lipoproteins (IDL).
- Type IV – increased VLDL values.
- Type V – high level of VLDL and cholesterol.
Based on its origin, hypercholesterolemia is divided into:
1. Primary
. This form is in turn divided into:
- Polygenic. The most common variety. Caused by a combination of genetic predisposition and exposure to exogenous factors (diet, smoking, etc.).
- Family. Caused by various hereditary disorders of lipid metabolism due to genetic mutations.
2. Secondary
. High levels of cholesterol in the blood, which develops against the background of certain diseases, endocrine disorders, or taking medications.
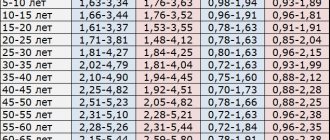
Based on the degree of increase in blood cholesterol levels, the following are distinguished:
- Mild hypercholesterolemia
– from 5.0 to 6.4 mmol/l. - Moderate hypercholesterolemia
– from 6.5 to 7.8 mmol/l. - High hypercholesterolemia
– 7.9 mmol/l and above.
Pathogenesis
The pathogenesis of dyslipidemia depends on its type - primary or secondary. It has been established that familial dyslipidemia (primary) is based on genetically determined factors (mutations in the genes encoding LDL receptor proteins), inherited in an autosomal dominant manner and causing homozygous/heterozygous hypercholesterolemia . The accumulation of LDL is caused by a decrease in the activity of the receptor, which is responsible for the excretion of lipoproteins. It is their accumulation in the subendothelial space that underlies the formation of atherosclerotic plaques. Moreover, the higher the LDL level, the higher the intensity of the process. When inherited, gene mutations can cause overproduction (high levels of LDL) or underproduction/overexcretion of HDL. LDL is especially poorly excreted in individuals with homozygous hypercholesterolemia, since the mutation is present in two paired genes, which significantly reduces the functionality of the receptor and is poorly corrected by drug treatment and dietary nutrition. In cases of heterozygous type hypercholesterolemia, only one gene is defective, that is, half of the receptors retain their functions, therefore, despite the increase in LDL, clinical manifestations are absent for a long time.
The pathogenesis of secondary hypercholesterolemia is based on excessive intake of cholesterol from high-calorie foods or an increase in the concentration of LDL, due to its increased synthesis in various diseases ( obesity , endocrine pathologies , kidney diseases , etc.) or taking various medications.
Causes of hypercholesterolemia
Physiological
Cholesterol values can also exceed normal levels in healthy people. For example, changes in the balance of female sex hormones during pregnancy cause an increase in cholesterol levels. After childbirth, the indicators return to normal. In case of improper preparation before taking a biochemical blood test (eating fatty foods on the eve of blood donation), cholesterol turns out to be higher than normal.
Hereditary disorders of lipid metabolism
This group of diseases is called “hereditary (familial) hypercholesterolemia.” They are caused by mutations in genes encoding the expression of lipoprotein receptors (LDLR, ApoB-100, PCSK9) or the lipoprotein lipase enzyme. This leads to disruption of catabolism and absorption of lipoproteins by cells, as a result of which the concentration of cholesterol in the blood begins to increase significantly.
A distinctive feature of familial forms of hypercholesterolemia is the detection of very high levels of cholesterol (in homozygous patients it can reach 20 mmol/l) already from early childhood (5-7 years). All this is associated with the rapid progression of atherosclerosis and the development of serious cardiovascular complications already at 20-25 years of age. Aggressive lipid-lowering therapy is required to normalize cholesterol levels.
Xanthelasma on the eyelids is a sign of hypercholesterolemia
Obesity
Excess weight ranks first among the etiological factors of hypercholesterolemia and accounts for more than 90% of all its cases. The pathogenesis of the effect of excess weight on cholesterol levels is as follows. Adipocytes secrete a large amount of biologically active substances that reduce the sensitivity of cells to insulin, and insulin resistance is formed.
As a result, lipolysis and the release of free fatty acids (FFA) are activated. From excess FFA entering the liver, a large amount of VLDL, one of the cholesterol fractions, is synthesized. Hypercholesterolemia increases slowly and is directly proportional to the degree of obesity; it can gradually return to normal with weight loss, but over a long period of time it becomes irreversible.
Kidney diseases
The cause of hypercholesterolemia can be kidney diseases accompanied by nephrotic syndrome: the initial stage of glomerulonephritis, diabetic or hypertensive nephropathy, nephropathy with multiple myeloma. An increase in cholesterol levels is associated with the loss in urine of carrier proteins and enzymes involved in lipid catabolism (lecithin-cholesterol acetyltransferases, lipoprotein lipases).
The severity of hypercholesterolemia correlates with the degree of proteinuria. After specific therapy for the underlying disease and relief of nephrotic syndrome, cholesterol levels usually normalize, but in some cases they remain elevated for a long time, which may require additional therapeutic measures to prevent the progression of atherosclerosis.
Endocrine disorders
Diseases of the endocrine system occupy a special place in the structure of the causes of hypercholesterolemia. Insufficiency or excess production of a particular hormone causes significant changes at different stages of lipid metabolism.
- Diabetes mellitus type 2.
The most common cause among endocrine diseases. The mechanism of development of hypercholesterolemia is the same as in obesity (relative insulin deficiency, increased synthesis of VLDL). The degree of increase in cholesterol corresponds to the severity of diabetes. To normalize indicators, both antidiabetic and lipid-lowering therapy are necessary. - Hypothyroidism.
Thyroxine and triiodothyronine stimulate the formation of VLDL receptors and regulate the activity of cholesterol-7-alpha-hydroxylase, the main enzyme in the synthesis of bile acids. A decrease in the concentration of thyroid hormones in hypothyroidism leads to a slowdown in the catabolism of VLDL and the conversion of cholesterol into bile acids. Hypercholesterolemia is moderate, completely reversible. Disappears along with other symptoms of the disease after hormone replacement therapy. - Cushing's disease/syndrome.
Primary and secondary hypercortisolism increase cholesterol levels both directly (adrenocortical hormones and glucocorticosteroids reduce the number of VLDL receptors) and indirectly (through the development of steroid-induced diabetes mellitus). Hypercholesterolemia is more pronounced and more persistent than with hypothyroidism.
Cholestasis
An increase in serum cholesterol levels can be observed in diseases of the liver and biliary tract, accompanied by intra- or extrahepatic cholestasis (stagnation of bile). Hypercholesterolemia is caused by impaired utilization of cholesterol for the production of bile acids. Its degree correlates with the severity of cholestasis.
The highest rates are observed in primary sclerosing cholangitis, primary and secondary biliary cirrhosis, less pronounced in parenchymal liver diseases (alcoholic, viral hepatitis, fatty liver). Elimination of cholestasis leads to a fairly rapid normalization of cholesterol.
Other reasons
- Autoimmune diseases:
systemic lupus erythematosus, hypergammaglobulinemia. - Metabolic disorders:
gout, storage diseases (Gaucher disease, Niemann-Pick disease). - Mental illness:
anorexia nervosa. - Taking medications:
oral contraceptives, beta-blockers, thiazide diuretics.
Prevention
The main measures for the primary prevention of hypercholesterolemia include:
- Normalization of weight to the norm corresponding to gender and age.
- Dietary food with a reduced fat content, enriched with fiber/vitamins and a reduction in salt intake to 5 g/day.
- Increasing the level of physical activity (selected individually).
- Refusal/minimization of alcohol intake and avoidance of smoking.
- Limiting overloads in the psycho-emotional sphere.
- Maintain normal blood pressure/blood glucose levels.
- Timely treatment of diseases that contribute to the development of dyslipidemia ( diabetes mellitus , liver, thyroid, kidney diseases).
Diagnostics
Laboratory hypercholesterolemia is detected by examining venous blood. In addition to the concentration of total cholesterol, the determination of its fractions and triglycerides is of great information. For differential diagnosis, the patient’s age and other anamnestic data are important - taking medications, the presence of close relatives with a confirmed familial form of hypercholesterolemia. To clarify the etiological factor, the following examination is carried out:
- Routine laboratory tests.
The content of liver transaminases (ALT, AST), markers of cholestasis (alkaline phosphatase, gamma-glutamyl transpeptidase), and glucose are measured. If nephrotic syndrome is suspected, a general urinalysis, analysis for microalbuminuria, and daily proteinuria are performed. - Hormonal studies.
The concentration of TSH and thyroid hormones (free T4 and T3) is determined. To confirm hypercortisolism, the level of cortisol in the blood is checked after performing small and large dexamethasone tests. - Immunological tests.
Tests are performed for markers of viral hepatitis (HBsAg, HCV), antimitochondrial (AMA), antineutrophil (ANCA) antibodies. - Ultrasound.
An ultrasound of the abdominal organs may reveal gall bladder stones, wall thickening, and signs of fatty infiltration in the liver. - Genetic research.
If hereditary hypercholesterolemia is suspected, mutations in the LDLR, PSCK-9, and ApoB-100 receptor genes are detected using the polymerase chain reaction.
For drug correction of hypercholesterolemia, different groups of drugs are prescribed
List of sources
- Diagnosis and treatment of familial hypercholesterolemia (Russian recommendations) / M.V. Ezhov, I.V. Sergienko, T.A. Rozhkova [and others] // Bulletin of modern clinical medicine. - 2021. - T. 10, issue. 2. - P.72-79.
- Bubnova M.G., Kukharchuk V.V. Recommendations of the European Society of Cardiology and the European Society of Atherosclerosis for the diagnosis and treatment of dyslipidemia: main provisions // Cardiology. - 2021. - No. 3. - P. 85-59.
- Practical lipidology with methods of medical genetics: a guide / V.A. Koshechkin, P.P. Malyshev, T.A. Rozhkova. - M.: GEOTAR-Media, 2015. - 112 p.
- Low and very low density lipoproteins: pathogenetic and clinical significance / V.N. Titov, I.A. Vostrov, S.I. Kaba et al. // Clinical medicine. - 2013. - No. 1. - With. 20-27.
- Familial hypercholesterolemia: screening, diagnosis and treatment of children and adult patients: clinical guidelines prepared by the expert group on familial hypercholesterolemia at the National Lipid Association of the USA // Atherosclerosis and dyslipidemia - 2012 - No. 1.
Correction
Conservative therapy
If hypercholesterolemia is detected, it is imperative to consult a doctor to find out the cause of this laboratory phenomenon and select appropriate treatment. Much attention is paid to the fight against the underlying disease (immunosuppressive therapy for nephrotic syndrome, hormone replacement therapy for hypothyroidism, choleretic therapy for cholestasis), since its elimination can lead to normalization of cholesterol levels without additional intervention.
Non-drug methods for correcting hypercholesterolemia include complete smoking cessation and limiting alcohol consumption. Also, in order to reduce body weight, obese patients must follow a diet with a decrease in the proportion of animal fats in the diet (butter, fried meat, sausages) and an increase in vegetable fats (vegetables, seafood), fruits and whole grains, and regularly perform various physical exercises.
For the drug correction of hypercholesterolemia, the following drugs are used:
- Statins
(atorvastatin, rosuvastatin). The most effective and frequently prescribed means to reduce cholesterol levels. The mechanism of action is based on the suppression of cholesterol synthesis in the liver. - Fibrates
(clofibrate). These drugs stimulate the activity of the LPL enzyme, thereby accelerating the degradation of the drug. They reduce not only cholesterol, but also triglycerides, so they often become the drugs of choice for patients suffering from diabetes. - Ezetimibe
. Inhibits the absorption of cholesterol in the intestine. Used in combination with statins. - PCSK9 inhibitors
(alirocumab). These are monoclonal antibodies that bind to LDL receptors in the liver, which stimulates the breakdown of lipoproteins. Prescribed when statins are ineffective. - Bile acid sequestrants
(cholestyramine, colestipol). They are ion exchange resins that suppress the absorption of bile acids in the intestine. Depletion of FA reserves activates their synthesis from cholesterol in the liver. Used in patients with cholestasis. - A nicotinic acid
. This drug reduces the flow of fatty acids into the liver, which suppresses the synthesis of lipid. It has a weak hypocholesterolemic effect, therefore it is used as an addition to other drugs. - Omega-3 fatty acids
. Eicosapentaenoic acid and docosahexaenoic acid are components of fish oil. These substances bind to the nuclear PPAR receptors of liver cells, which leads to a decrease in serum lipid levels.
Surgery
One of the prerequisites for the effective treatment of hypercholesterolemia is normalization of body weight. For patients with morbid obesity (body mass index above 40), especially in combination with type 2 diabetes mellitus, if conservative methods are unsuccessful, bariatric surgery is indicated - gastric banding, gastric bypass or resection.
If hypercholesterolemia is caused by cholestasis due to cholelithiasis, surgical removal of the gallbladder (cholecystectomy) is performed. Patients with Cushing's disease undergo endoscopic transnasal adenomectomy (removal of the pituitary adenoma). For Itsenko-Cushing syndrome, bilateral adrenalectomy is used.
Diet
Diet for high cholesterol
- Efficacy: therapeutic effect after 2 months
- Terms: 2 months or more
- Cost of food: 1700 - 1800 rubles per week
If LDL cholesterol is elevated, this means that, along with drug therapy, it is necessary to organize proper nutrition, since diet therapy is one of the most important conditions for the qualitative/quantitative correction of lipid metabolism disorders. It has been established that an increase in cholesterol intake in a ratio of 100 mg per 1000 kcal/day increases the concentration of cholesterol in the blood by 12%. Limits on dietary intake of exogenous cholesterol should range from 250 to 500 mg/day depending on the type of hyperlipidemia. According to NOPH recommendations, for severe hypercholesterolemia, the amount of cholesterol in the diet should not exceed 200 mg/day, and for moderate hypercholesterolemia, 300 mg/day. For this purpose, products containing a lot of cholesterol are excluded from the diet - fish caviar, brains, fatty cheeses, internal organs of animals, egg yolk, butter, etc.).
The fat content in the daily diet should not exceed 30% of its calorie content (70–80 g/day). At the same time, the share of saturated fatty acids should account for 8–10% (sausages, fatty fish/meat, dairy products, etc.); polyunsaturated acids - 7-9% (butter) and monounsaturated acids - 10-15% (vegetable oils - olive, sunflower, cottonseed, corn, etc.).
It is extremely important to use PUFAs of the omega-3 family in the diet - various fatty sea fish (water herring, mackerel, halibut, sardines, etc.) containing eicosapentaenoic/docosahexaenoic long-chain fatty acids, which take part in the production of leukotrienes, prostaglandins, which have anti-inflammatory, antiplatelet, hypotensive effect.
Phospholipids, which have a hypolipidemic effect and reduce the absorption of cholesterol in the intestine, are also extremely necessary in the diet. Their main source is unrefined vegetable oils. They can also be introduced into the diet in the form of dietary supplements (for example, Vitol ).
In addition to the fat component in the diet, soy protein/isoflavones, as well as dietary fiber, have a significant effect on lipid metabolism. Sources of vegetable protein can be legumes (especially soybeans and products based on it), baked goods, and cereals. Soy isoflavones have a positive effect: consuming 25 g of soy protein daily significantly reduces blood cholesterol levels. An obligatory component of the diet is dietary fiber (pectin, cellulose, hemicellulose), which is achieved by including grains, wheat bran, vegetables, and fruits in the diet, which allows you to fully meet the daily requirement for them (30–50 g).
It is equally important to control the intake of carbohydrates into the body. It has been established that the consumption of refined carbohydrates contributes to an increase in the concentration of low-density lipoproteins/triglycerides in the blood, while the consumption of complex carbohydrates contributes to a decrease in the concentration of atherogenic lipoprotein fractions in the blood serum, excess body weight, and blood pressure levels. And in general, the consumption of refined carbohydrates contributes to an increase in calorie content, an increase in body weight and endogenous cholesterol synthesis (increases by 20 mg/kg of excess body weight).
A number of micronutrients play an important role in the regulation of lipid metabolism:
- Iodine - has a hypocholesterolemic effect, affects the function of the thyroid gland, and prevents the formation of atherosclerotic plaque. Its main sources are seafood: seaweed, sea fish, mussels, shrimp.
- Chromium is involved in lipid metabolism and prevents the process of lipid deposition in the vascular wall. Sources of chromium: legumes, wholemeal wheat/rye flour, baker's yeast, meat, corn/pearl barley.
- Selenium - has antioxidant activity, reduces the risk of atherosclerosis , normalizes blood clotting.
- Vitamins with antioxidant effects - vitamin E (vegetable oils, legumes, nuts, seeds); vitamin A (eggs, liver, chum salmon caviar, butter) and beta-carotene (its precursor (green onions, carrots/red peppers, spinach, sorrel, tomatoes, sea buckthorn, rowan); vitamin C (vegetables/fruits); group vitamins B (milk, meat, fish, liver, seafood, soybeans, beans, buckwheat, millet, cauliflower, green onions, yeast, cauliflower).
Flavonoids contained in vegetables/fruits, legumes, Rosaceae, buckwheat and Asteraceae have biological activity in relation to fat metabolism, which is due to their antioxidant effect. The antioxidant/hypolipidemic effect of squalene, which is contained in amaranth seed oil and shark liver oil, is also known.
Of significant interest are phytosterols/phytostanols, which are contained in rapeseed coconut, soybean oil, seeds, nuts, and coniferous seed oil, which have a mild effect on lipid metabolism.
To reduce the fat/calorie content of the diet, you should use the correct cooking technology (boiling, baking, stewing).
The possibility of using alcohol to influence the lipid profile should be done with caution (assuming that the patient will comply with the recommended dose) - vodka/cognac/whisky at a dose of 45–50 ml/day, table wine (red/white) at a dose of 150 ml per day day.
Can dietary supplements increase cholesterol levels? If you follow the instructions, no, they can’t; at the same time, if they are abused, side effects can develop. For example, long-term use of dietary supplements containing fiber in doses of more than 60 g/day can cause disruption of the absorption of microelements/vitamins.
Forecast
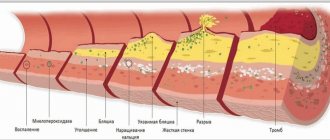
Hypercholesterolemia leads to the deposition of cholesterol on the walls of arterial vessels, the formation of atherosclerotic plaques, narrowing of the lumen and deterioration of blood supply to organs and tissues. This is of primary clinical importance for the coronary and cerebral arteries. Therefore, a long-term increase in cholesterol concentration is an unfavorable prognostic factor for cardiovascular diseases and is associated with such serious complications as acute myocardial infarction and acute cerebrovascular accident.
Symptoms
Hypercholesterolemia, in itself, is predominantly asymptomatic, however, as already indicated, it can cause vascular damage, which is manifested by clinical symptoms of coronary heart disease , peripheral artery disease, and stroke . Symptoms of hypercholesterolemia are present in a minority of patients. Most often these are tendon xanthomas, which are compactions of cholesterol in the form of nodules that can be felt over the tendons.
With high levels of LDL against the background of familial hypercholesterolemia in the homozygous form a corneal arch (arc-shaped opacification of the cornea), as well as characteristic xanthomas of the knee, elbow, Achilles tendon and tendons in the area of the carpophalangeal joints, may appear. Another manifestation may be xanthelasmas, which are cholesterol deposits under the skin of the eyelids in the form of yellow plaques located in the medial part of the eyelids.
In advanced cases, mosaic symptoms of damage to internal organs develop (at the stage of development
of atherosclerosis ).
Menu (Power Mode)
It is necessary to organize 5 meals a day. If you feel hungry in the evening before going to bed, you can eat apples, oranges, carrots or drink kefir. The menu for three days might look like this:
The first day
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
Second day
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
Day three
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
Below is a table of products on the basis of which you can create a varied diet for the whole week.
| Products name | Featured | Prohibited |
| Meat | Turkey, chicken, veal, rabbit, lean beef (twice a week). Poultry without skin; additionally remove fat from meat. | Pork, fatty beef, lamb, duck and goose meat, all sausage products, pates, sausages, sausages, liver, kidneys, brains. |
| Eggs | Up to 3 pieces per week. | Egg yolk. |
| Fats | Unrefined sunflower, corn, olive or soybean oils up to 2.5 tablespoons per day in all dishes. | Margarine, lard, animal fat, palm and coconut oil, butter. |
| Fish | Lean sea fish (hake, blue whiting, pollock, navaga, pollock, haddock) and pike three times a week. | Fatty species: salmon, mackerel, sardine, eel, mackerel, tuna, herring, oysters, caviar, shrimp, processed fish, limited river fish. |
| Dairy | Skim milk or 1% fat, low-fat kefir, natural yogurt, “Grace” or “Fitness” cheeses, 20% low-fat cottage cheese. | Full-fat cottage cheese, cream, sour cream, ice cream, curd mass and glazed sweet cheeses, processed cheeses, condensed milk. |
| Vegetables | All fresh and frozen vegetables, legumes, corn. | French fries and chips. |
| Fruits | All fruits except banana and grapes, dried fruits. | Candied fruits, peanuts, pistachios and hazelnuts. |
| Cereals | Brown rice, oatmeal, durum and whole grain pasta, whole grain bread. | White rice, semolina, limit buckwheat. |
| Bakery | Oatmeal cookies, bread and fitness cookies. | Biscuits, rolls, pastries, cakes, puff pastry products. |
| Sweets | Low-fat puddings, sugar-free jellies, popsicles, frozen juice. | Chocolate, pastry cream, toffee, marmalade, pastille, sugar, syrups, glucose and fructose. |
| Beverages | Juices without sugar, tea, weak coffee, still mineral water. | Cocoa, coffee with cream and milk, alcoholic and sweet carbonated drinks. |
Authorized Products
The diet for hypercholesterolemia involves the consumption of vegetarian soups, as well as soups prepared in secondary broth. To do this, boil beef or chicken for 10 minutes in a small amount of water. The first water is drained, the meat is washed and refilled with water and cooked until cooked. In the secondary broth, you need to carefully skim off the fat. This way you can cook cabbage soup and borscht. Potatoes are added in minimal quantities. Initially, lean meat and poultry are chosen - it could be beef, chicken or turkey.
When cooking poultry, the skin should not be used, and fat from the meat, if present, must be trimmed off. It is better to boil, bake or steam meat for main courses. You can serve with a small amount of porridge (oatmeal, buckwheat and brown rice), but preferably vegetable side dishes (all types of cabbage, carrots, eggplant, zucchini, pumpkin, beets) or salads of fresh vegetables and green peas. All kinds of vegetable oils are used to season ready-made dishes. The oils are exclusively virgin and unrefined.
Most of the meals should be made from sea fish, not meat. The best dietary varieties are: hake, blue whiting, pollock, navaga, pollock, river haddock - pike. Bread made from rye, as well as from grain flour and with bran is allowed.
You can bake your own low-fat cookies from oatmeal or soy flour, as well as unsweetened bread from whole grain flour with the addition of bran and flax seeds and use them instead of bread. Milk and fermented milk products are consumed with low fat content, and eggs are allowed up to 2-3 per week (boiled or omelettes).
Tea and weak coffee with the addition of skim milk, vegetable juices, natural berry or fruit juices without sugar are allowed.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| eggplant | 1,2 | 0,1 | 4,5 | 24 |
| beans | 6,0 | 0,1 | 8,5 | 57 |
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| broccoli | 3,0 | 0,4 | 5,2 | 28 |
| Brussels sprouts | 4,8 | 0,0 | 8,0 | 43 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| corn | 3,5 | 2,8 | 15,6 | 101 |
| green onion | 1,3 | 0,0 | 4,6 | 19 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| squash | 0,6 | 0,1 | 4,3 | 19 |
| salad pepper | 1,3 | 0,0 | 5,3 | 27 |
| parsley | 3,7 | 0,4 | 7,6 | 47 |
| salad | 1,2 | 0,3 | 1,3 | 12 |
| beet | 1,5 | 0,1 | 8,8 | 40 |
| celery | 0,9 | 0,1 | 2,1 | 12 |
| soybeans | 34,9 | 17,3 | 17,3 | 381 |
| asparagus | 1,9 | 0,1 | 3,1 | 20 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| Jerusalem artichoke | 2,1 | 0,1 | 12,8 | 61 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
| dill | 2,5 | 0,5 | 6,3 | 38 |
| beans | 7,8 | 0,5 | 21,5 | 123 |
| garlic | 6,5 | 0,5 | 29,9 | 143 |
| lentils | 24,0 | 1,5 | 42,7 | 284 |
Fruits | ||||
| avocado | 2,0 | 20,0 | 7,4 | 208 |
| oranges | 0,9 | 0,2 | 8,1 | 36 |
| pomegranate | 0,9 | 0,0 | 13,9 | 52 |
| grapefruit | 0,7 | 0,2 | 6,5 | 29 |
| pears | 0,4 | 0,3 | 10,9 | 42 |
| lemons | 0,9 | 0,1 | 3,0 | 16 |
| mango | 0,5 | 0,3 | 11,5 | 67 |
| tangerines | 0,8 | 0,2 | 7,5 | 33 |
| nectarine | 0,9 | 0,2 | 11,8 | 48 |
| peaches | 0,9 | 0,1 | 11,3 | 46 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Berries | ||||
| gooseberry | 0,7 | 0,2 | 12,0 | 43 |
| Red currants | 0,6 | 0,2 | 7,7 | 43 |
| black currant | 1,0 | 0,4 | 7,3 | 44 |
Nuts and dried fruits | ||||
| nuts | 15,0 | 40,0 | 20,0 | 500 |
| almond | 18,6 | 57,7 | 16,2 | 645 |
| flax seeds | 18,3 | 42,2 | 28,9 | 534 |
| fenugreek seeds | 23,0 | 6,4 | 58,3 | 323 |
| sunflower seeds | 20,7 | 52,9 | 3,4 | 578 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| oat groats | 12,3 | 6,1 | 59,5 | 342 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| wheat bran | 15,1 | 3,8 | 53,6 | 296 |
Raw materials and seasonings | ||||
| basil | 2,5 | 0,6 | 4,3 | 27 |
| honey | 0,8 | 0,0 | 81,5 | 329 |
Dairy | ||||
| kefir 0% | 3,0 | 0,1 | 3,8 | 30 |
| kefir 1% | 2,8 | 1,0 | 4,0 | 40 |
Cheeses and cottage cheese | ||||
| cottage cheese 0.6% (low fat) | 18,0 | 0,6 | 1,8 | 88 |
| curd tofu | 8,1 | 4,2 | 0,6 | 73 |
Meat products | ||||
| beef | 18,9 | 19,4 | 0,0 | 187 |
Bird | ||||
| chicken fillet | 23,1 | 1,2 | 0,0 | 110 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Eggs | ||||
| eggs | 12,7 | 10,9 | 0,7 | 157 |
Fish and seafood | ||||
| fish | 18,5 | 4,9 | 0,0 | 136 |
| seaweed | 0,8 | 5,1 | 0,0 | 49 |
Oils and fats | ||||
| grape seed oil | 0,0 | 99,9 | 0,0 | 899 |
| linseed oil | 0,0 | 99,8 | 0,0 | 898 |
| olive oil | 0,0 | 99,8 | 0,0 | 898 |
| sunflower oil | 0,0 | 99,9 | 0,0 | 899 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| * data is per 100 g of product | ||||
Meaning of the term
Before looking at hypercholesterolemia, it is important to understand what cholesterol is. It is one of the many chemical compounds present in the human body that falls under the category of fatty substances or lipids. The word cholesterol consists of two Greek words “chole” - bile, “steros” - solid, which translates as “hard bile”. The substance is a natural fatty alcohol, which is why in many sources it is called “cholesterol”.
Cholesterol, from the point of view of the physiology of the body, is one of the necessary and very important components of cell membranes, which are responsible for their stability. More precisely, each cell membrane consists of cholesterol, and it is this that determines its permeability and rigidity. The described substance is part of bile acids, ensuring normal digestion, and also participates in the synthesis of vitamins and hormones (sex and adrenal).
Reference! In fact, the human body is capable of independently synthesizing the amount of cholesterol necessary for life. This function is performed by the main gland – the liver. In the body of a healthy person, 80% of cholesterol is produced by the liver and only 20% comes from the outside, that is, from food.
Since cholesterol is a fatty substance, it cannot but mix with blood, the main part of which is water, and dissolve in it. To ensure the possibility of circulation in the bloodstream, the substance is covered with a kind of shell formed by protein molecules - proteins. Lipids that have a protein shell are called lipoproteins.
At the same time, substances in this group are characterized by significant differences. Lipoprotein particles can be of four types: very low density (VLDL), low density (LDL), intermediate density (LDL) and high density (HDL). The first three listed varieties contain “bad” cholesterol, which can be deposited on the vascular walls, forming atherosclerotic plaques. And HDL contains “good” cholesterol.
They collect cholesterol from the walls of blood vessels and transport it to the liver. Then, as part of bile, it is excreted from the liver into the gastrointestinal tract. This is how the “good” form of cholesterol, which HDL contains, prevents the development and progression of atherosclerosis.