High-density lipoproteins are compounds consisting of lipids (fats) and proteins. They ensure the processing and removal of fats from the body, which is why they are called “good cholesterol”.
Synonyms Russian
HDL, high density lipoprotein, HDL, HDL cholesterol, alpha cholesterol.
English synonyms
HDL, HDL-C, HDL Cholesterol, High-density lipoprotein cholesterol, High-density lipoprotein, Alpha-Lipoprotein Cholesterol.
Research method
Colorimetric photometric method.
Units
mmol/l (millimoles per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress and do not smoke for 30 minutes before the test.
General information about the study
Cholesterol (CH, cholesterol) is a fat-like substance vital to the body. The correct scientific name for this substance is “cholesterol” (the ending -ol indicates that it belongs to alcohols), however, the name “cholesterol” has become widespread in the popular literature, which we will use later in this article. Cholesterol is formed in the liver and also enters the body with food, mainly meat and dairy products. Cholesterol is involved in the formation of cell membranes of all organs and tissues of the body. Hormones are created on the basis of cholesterol, which are involved in the growth, development of the body and the implementation of the reproduction function. Bile acids are formed from it, thanks to which fats are absorbed in the intestines.
Cholesterol is insoluble in water, so to move around the body it is “packed” into a protein shell consisting of special proteins - apolipoproteins. The resulting complex (cholesterol + apolipoprotein) is called lipoprotein. Several types of lipoproteins circulate in the blood, differing in the proportions of their components:
- very low density lipoproteins (VLDL),
- low density lipoproteins (LDL),
- high density lipoproteins (HDL).
High-density lipoproteins consist mainly of protein and contain some cholesterol. Their main function is to transport excess cholesterol back to the liver, from where it is excreted as bile acids. Therefore, HDL cholesterol (HDL-C) is also called “good cholesterol.” HDL makes up about 30% of the total cholesterol (cholesterol) in the blood.
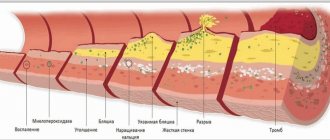
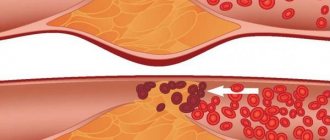
If a person has a genetic predisposition to high cholesterol or eats too much fatty foods, the level of cholesterol in the blood may rise so that the excess is not completely eliminated by high-density lipoproteins. It begins to be deposited in the walls of blood vessels in the form of plaques, which can limit the movement of blood through the vessel and also make the vessels more rigid (atherosclerosis), which significantly increases the risk of heart disease (coronary artery disease, heart attack) and stroke.
High levels of HDL cholesterol reduce the risk of developing plaques in blood vessels, as they help remove excess cholesterol from the body. A decrease in HDL cholesterol, even with normal levels of total cholesterol and its fractions, leads to the progression of atherosclerosis.
What is the research used for?
- To assess the risk of developing atherosclerosis and heart problems.
- To monitor the effectiveness of a low-fat diet.
When is the study scheduled?
- An HDL test is performed during routine preventive examinations or when total cholesterol is elevated as part of a lipid profile. It is recommended that all adults over 20 years old have a lipid profile at least once every 5 years. It may be prescribed more frequently (several times a year) if the patient is prescribed a diet limited in animal fats and/or is taking cholesterol-lowering medications. In these cases, it is checked whether the patient achieves the target level of HDL cholesterol and total cholesterol and, accordingly, whether his risk of cardiovascular diseases is reduced.
- With existing risk factors for developing cardiovascular diseases: smoking,
- age (men over 45 years old, women over 55 years old),
- increased blood pressure (140/90 mm Hg and above),
- cases of high cholesterol or cardiovascular diseases in other family members (heart attack or stroke in the closest male relative under 55 years old, female relative under 65 years old),
- existing coronary heart disease, previous myocardial infarction or stroke,
- diabetes,
- excess body weight,
- alcohol abuse,
- eating large amounts of food containing animal fats,
- low physical activity.
What do the results mean?
Reference values
Men: > 1.0 mmol/l.
Women: > 1.2 mmol/l.
The concept of “normal” is not entirely applicable to the level of HDL cholesterol. For different people with different numbers of risk factors, the HDL level will be different. To determine the risk of developing cardiovascular disease more accurately for a specific person, it is necessary to evaluate all predisposing factors. In general, we can say that a reduced level of HDL predisposes to the development of atherosclerosis, and a sufficient or high level prevents this process.
According to clinical guidelines1, when assessing cardiac risk, a level of > 1.0 mmol/L for men and > 1.2 mmol/L for women indicates low risk.
“Diagnostics and correction of lipid metabolism disorders for the purpose of prevention and treatment of atherosclerosis. Russian recommendations, VII revision. 2020".
"2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk."
Reasons for low HDL levels:
- heredity (Tangier disease),
- cholestasis - stagnation of bile, which can be caused by liver disease (hepatitis, cirrhosis) or gallstones,
- severe liver disease,
- untreated diabetes mellitus,
- chronic inflammation of the kidneys leading to nephrotic syndrome,
- chronic renal failure.
Causes of elevated HDL levels:
- hereditary predisposition,
- chronic liver disease,
- alcoholism,
- frequent intense aerobic exercise.
What can influence the result?
HDL cholesterol levels may change from time to time. A single measurement does not always reflect the “usual” amount of cholesterol, so sometimes you may need to retake the test after 1-3 months. Sometimes HDL cholesterol levels may be higher or lower for a short period of time. This phenomenon is called biological variation and reflects normal fluctuations in cholesterol metabolism in the body.
Reduces HDL levels:
- stress, recent illness (after which you need to wait at least 6 weeks),
- anabolic steroids, androgens, corticosteroids.
Increases HDL levels:
- pregnancy (lipid profile should be taken at least 6 weeks after the birth of the child),
- statins, cholestyramine, phenobarbital, fibrates, estrogens, insulin.
Lipid profile parameters
The laboratory measurement value for total cholesterol and its fractions is mmol/l. Indicators included in the lipid profile:
Normal blood cholesterol levels
- OX (Cho);
- HDL;
- LDL;
- VLDL;
- HM;
- TG;
- KA (IA).
TC – total cholesterol level. KA – coefficient (otherwise, index) of atherogenicity. When assessed by electrophoretic method, fractions are divided:
- alpha lipoproteins or HDL;
- beta lipoproteins – LDL;
- prebeta lipoproteins – VLDL.
The CA value is a laboratory marker that reflects the degree of danger of atherosclerotic changes in blood vessels. It is calculated using the formulas: KA = (LDL + VLDL) / HDL or IA = (Cho – HDL) / HDL.
Normal lipid status
The norms for total cholesterol do not depend on gender. For men and women from 20 to 45 years old, the indicators should fall within the range of 3.2-5.2 mmol/l. If the result is equal to or greater than 6.7 mmol/l, then the patient is diagnosed with hypercholesterolemia.
At values below the norm of 3.2 mmol/l – hypocholesterolemia. Both disorders are considered pathologies. Reference values for high-density and low-density lipoproteins differ by gender and age category.
Normal indicators
The values of triglycerides and very low density lipoproteins for men and women are identical:
- TG – 0.41-1.8 mmol/l;
- VLDL – 0.26-1.04 mmol/l.
For the atherogenicity coefficient, only inflated values are of diagnostic value. The higher the KA, the higher the risk of atherosclerosis.
CA norm table
How to increase good cholesterol if HDL is low
A person may have a different percentage of HDL cholesterol at different times. Therefore, a single blood test is not an indicator of the “usual” amount of cholesterol. This indicates the need to check the level of the substance regularly if there is a fear of an increase. Changes can occur over a short period of time, this is called fluctuations in cholesterol metabolism. To increase your HDL level you should:
- exclude corticosteroids, anabolic steroids, androgens;
- avoid stressful situations;
- take statins, fibrates, cholestyramine, phenobarbital, insulin, estrogens.
Find out more about LDL - what it is, how to get tested.
Functions
Lipoproteins play an important role in the human body. Thanks to transport proteins, cholesterol dissolves in the blood plasma and begins to move throughout the body. Cholesterol enters the body not only from food. Almost 80% of the fat metabolism component is produced in the liver.
Cholesterol takes an active part in the synthesis of sex hormones and has a strengthening and protective effect on cell membranes. In addition, the fat metabolism component contributes to the restoration of cell membranes and the production of vitamin D.
Results
HDL and LDL are the most important participants in cholesterol metabolism, the amount of which in the blood must meet certain standards. Low-density lipoproteins supply the body's cells with cholesterol, which is produced by the liver. High-density lipoproteins cleanse blood vessels of excess fat, preventing the development of atherosclerosis.
Dyslipidemia, otherwise an imbalance of LDL and HDL, accompanies a number of chronic diseases or is a consequence of unhealthy eating behavior, bad habits, and physical inactivity. You can check your fat metabolism levels by donating blood for a special test - a lipid profile.
What reduces HDL levels
There are genetic reasons for reducing HDL, but it is worth paying attention to the possibilities that can be controlled and bring HDL to a healthy norm.
Consumption of artificial trans fats
Artificial trans fats, found in margarine and many processed foods, are inflammatory and harmful to our health.
A study of 27 young women found that consuming partially hydrogenated soybean oil resulted in a 10% reduction in HDL levels compared to consuming palm oil. []
A study of 40 healthy adult women compared the effects of consuming trans fatty acids from natural sources with the effects of consuming industrial fats. The result of this comparison was the conclusion that industrially produced trans fats contributed to a decrease in the amount of HDL in the blood. []
Smoking
Cigarette smoking has undoubtedly been shown to be a significant factor in increasing the risk of heart disease. Smoking cigarettes reduces high-density lipoprotein (HDL) levels, and cigarette smoke itself can directly damage the HDL molecule, making it impossible for the molecule to protect the heart and blood vessels from cholesterol and inflammation. []
Diseases
Several health disorders that fall under the category of metabolic syndromes are associated with low levels of HDL in the blood. These disorders include type 2 diabetes , insulin resistance, central obesity (excess belly fat), high blood pressure and high triglycerides. []
In addition, most autoimmune diseases: rheumatoid arthritis, lupus, psoriasis, as well as periodontal disease and any infectious diseases reduce HDL levels. []
Preparing to donate blood for a lipid profile
Preliminary preparation for analysis is necessary to obtain accurate results. 2-3 days before the prescribed procedure, it is recommended to refuse foods rich in animal fats and alcoholic beverages (including weak alcohol), and stop taking any medications other than those necessary for medical reasons.
The day before the procedure:
- reduce physical activity;
- limit sugar intake.
Blood sampling is performed strictly on an empty stomach. The fasting regime should be at least 8 hours.