Atherosclerosis disability
Atherosclerosis is one of the most common diseases. Among the causes of death, it occupies a leading place in the world. Atherosclerosis refers to diseases that are caused by the influence of several unfavorable factors on the body at once, and therefore, the name is a polyetiological disease. This disease is characterized by generalized damage to the inner wall of blood vessels with the formation of atherosclerotic plaques.
Its danger lies in the fact that with existing atherosclerosis, patients become disabled due to complications that inevitably develop in the absence of treatment.
The risk of developing complications is determined by the individual characteristics of the body, hereditary predisposition and the presence of combined risk factors. In the absence of medical supervision and appropriate treatment and prevention, the natural result is progression of the disease. In atherosclerosis, disability is determined by the following diseases: transient (micro-strokes) and persistent disorders of cerebral circulation (stroke), acute disorders of the coronary blood supply (myocardial infarction), obliterating atherosclerosis, stenosis and aortic aneurysm. Each of the above diseases is complex, difficult to treat and can severe cases lead to disability.
With strokes, the patient acquires disability associated with paresis and paralysis, impaired movement in the limbs, and decreased mental abilities. Myocardial infarction is no less dangerous disease. A patient who has suffered a massive heart attack cannot perform normal physical activities, and in severe cases, discomfort occurs even at rest. Progressive heart failure does not allow one to lead the same lifestyle; often such patients require outside help. Obliterating atherosclerosis affects the vessels of the lower extremities, which can lead to gangrene and amputation.
In order to prevent the development of the disease and its complications, it is necessary to avoid those risk factors that can be influenced independently. Namely: exclude from the diet foods containing excess amounts of animal fats and cholesterol, lead a healthy lifestyle (exclude smoking, control body weight, lead an active lifestyle). The main thing in developing the concept of a healthy lifestyle is to understand those problems that lead to life-threatening complications.
Features of the disease
The insidiousness of atherosclerosis of the vessels of the lower extremities lies in the fact that this disease has no pronounced manifestations. There are no specific symptoms that would prompt immediate medical attention, with the exception of increased leg fatigue.
This circumstance allows the disease to develop unhindered over a long period. But there are manifestations that should alert every person:
- change in skin color on the legs - bluishness, pallor or purplishness;
- frequent numbness;
- spasms of the lower extremities;
- pain after physical exertion.
Manifestations can occur in the form of rare “bells” or all together (in a pre-infarction or pre-stroke state).
The progression of the disease leads to strokes, paralysis, paresis (partial limitation of mobility), and changes in intellectual capabilities. All these violations give the right to acquire a degree of disability.
A person suffering from atherosclerosis and having had a heart attack is unable to continue working. In some cases, physical discomfort is observed even at rest. Due to heart failure (occurs in every fifth patient with atherosclerosis), a person needs outside help and care.
Attention! At the last stage, trophic ulcers and gangrene form on the lower extremities. In case of gangrene, amputation of the limb is indicated.
A medical and social examination prescribes disability and selects a comprehensive program that will stop the development of the disease.
Registration of disability
When registering disability, the characteristics of the patient’s condition are taken into account, including complications due to the loss of a limb, in which a decrease in working capacity is inevitable. Particular attention is paid to rehabilitation.
To assign a degree of disability, the following data will be required:
- age, duration of the disease;
- information about the nature of professional activity;
- ability to move independently;
- degree of vascular damage;
- pain at rest;
- stage of ischemia;
- associated lesions;
- complications.
Those suffering from obliterating atherosclerosis of the vessels of the lower extremities, who did not have a disability before the removal of the leg, are assigned temporary disability until the completion of the prosthesis. Subsequently, they will have to undergo medical examination and, as a rule, receive disability group III.
For such patients, there are prohibitions on holding positions that involve:
- heavy or moderate work;
- actions that involve staying in one position for a long time;
- activities in stressful situations and the need to react quickly;
- work in low temperature conditions and/or with high moisture content;
- interaction with poisons or work in a radiation zone.
When is it necessary to undergo ITU?
A referral for a medical and social examination requires a number of indications:
- development of therapeutic measures for patients with a positive prognosis as a result of reconstructive surgery;
- employment with lower qualifications and less work;
- assignment of II and I disability groups with a negative labor prognosis;
- ineffective treatment or unsuccessful surgery when circulatory disorders persist;
- identification of indications for obtaining special vehicles;
- identifying the cause of disability.
For review by medical examination specialists, you will need to pass standard tests:
- urine, general and biochemical blood tests;
- on blood clotting;
- rheovasogram;
- Dopplerometry.
Indications for assignment of a disability group
Disability group III is determined when the patient is forced to leave his job:
- chronic atherosclerosis of the legs has been identified, and professional activity presupposes conditions that are unacceptable for this disease;
- there is a prosthetic limb stump and chronic atherosclerosis of the first degree;
- underwent surgery with subcompensation of blood circulation and atherosclerosis of I and II degrees.
The second disability group is assigned if there is:
- widespread chronic atherosclerosis of the lower extremities of III and IV degrees;
- stump on one limb and chronic atherosclerosis of degree II on the other;
- short stump of the femur of the lower limb;
- non-prosthetic stump of the lower limb;
- femoral stump and atherosclerosis of cerebral vessels;
- suppuration at the junction of the stump and the prosthesis.
Patients are defined as the first disability group if there is a loss of any ability to work and the ability to self-care, and the following occurs:
- atherosclerosis of both lower extremities;
- removal of one and chronic atherosclerosis of the other limb;
- stumps at the level of the thighs of both lower extremities;
- severe combined disorders;
- severe septic complications during operations.
Read more: Job description of a beauty salon massage therapist
Disability for obliterating atherosclerosis of the vessels of the lower extremities is assigned because this disease is characterized by an inevitable complication of the condition with loss of the ability to self-care.
Obliterating atherosclerosis of the lower extremities is a severe damage to the arteries, accompanied by the formation of lipid plaques that narrow the vascular lumen until the blood flow completely stops. In severe stages of the disease with an irreversible course, patients are assigned disability based on the results of a medical and social examination.
As you know, in order to receive a group, patients have to make a lot of effort and go to several doctors’ offices.
Let's consider the information on the topic “atherosclerosis of the lower extremities - is it a disability status” in more detail.
Medical and occupational examination for cerebral atherosclerosis
Among vascular diseases of the brain, atherosclerosis of cerebral vessels, as a cause of persistent decline in working capacity, ranks second after hypertension (read more in the article Medical and occupational examination for hypertension). The combination of hypertension with atherosclerosis of cerebral vessels, which is observed quite often, significantly worsens the clinical and work prognosis.
Atherosclerosis of cerebral vessels develops due to a violation of lipid metabolism. Disorders of lipid metabolism are usually combined with disorders of carbohydrate, water-salt and protein metabolism. Neuropsychic stress, improper work and lifestyle with the exception of physical exercise and poor nutrition (systemically introducing large amounts of fats and cholesterol-containing substances), past infections and intoxications, and smoking contribute to the development of atherosclerosis.
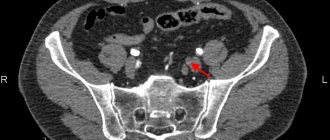
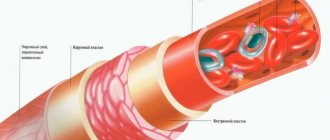
The atherosclerotic process proceeds sequentially: in the initial stage of the disease, deposits of lipid substances, mainly cholesterol, and its esters occur in the inner lining of blood vessels with the formation of atheromatous plaques (the primary infiltrative phase of the process), then a reactive proliferation of connective tissue occurs, and gradually these plaques become sclerotic (vascular atherosclerosis ). Sclerotic vessels lose their elasticity, the physiological reactivity of the vessels is disrupted or even distorted, and a pathological tendency to their spasm appears. Impaired nutrition of nerve cells leads to their degenerative changes and gradual atrophy of the brain matter, especially the cerebral cortex. Violation of the vessel wall causes the formation of miliary aneurysms. With severe atheromatosis and a sudden increase in blood pressure, rupture of the vessel wall may occur. The deposition of atheromatous plaques leads to a gradual narrowing of the lumen of the vessel and the formation of a wall thrombus, especially when the blood flow slows down and the overall blood pressure decreases. The vessels of the base and large (middle, anterior, posterior) cerebral arteries are most affected in the brain. Plaques occur especially often where arteries branch, where blood flow is slow.
It has now been proven that cerebral circulatory disorders are often caused by atherosclerosis of the main extracranial vessels, primarily the internal carotid, and less commonly, the basilar and vertebral arteries.
N. K. Bogolepov identified the following symptoms of dyscirculatory disorders on the part of the internal carotid artery as “carotid dyscirculatory syndrome”: fainting, short-term disturbances of consciousness or orientation, transient phenomena of muscle weakness and hypotonia, anisoreflexia, unclear pathological reflexes (on the side opposite to the lesion), pain in the parietal region, paresthesia in the extremities, sometimes mild gnostic and aphasic disorders (with left-sided localization of the vascular process), increased blood pressure. For transient circulatory disorders in the main artery, N.K. Bogolepov established the following symptoms: a feeling of lightheadedness, noise and heaviness in the head, transient double vision or paresis of gaze, impaired convergence, nystagmus, staggering when walking, vomiting, hiccups, short-term difficulty swallowing , dysarthria, dizziness, vasomotor disorders, sweating, pain and tenderness in the occipital region.
When there is blockage or a sharp narrowing of the lumen of the main artery, loss or a sharp decrease in vision, double vision, short-term loss of voice, dysarthria, choking, systemic dizziness, weakness or paresthesia in the legs and arms, and alternating syndromes are noted. Repeated crises involving the same arterial system are often characteristic of thrombosis of the carotid or basilar arteries. Clinically, they are distinguished: initial cerebral atherosclerosis, moderate atherosclerosis and severe cerebral atherosclerosis.
Initial atherosclerosis is subjectively manifested in a feeling of heaviness in the head, dull headaches, tinnitus, sometimes dizziness, short-term states expressed in “lightness”, “darkening in the eyes”, sleep is often upset, which becomes superficial, intermittent, increased irritability appears, fatigue, sometimes tearfulness, memory impairment. Objectively, premature graying is detected, sometimes very mild scattered organic neurological symptoms (narrowness of the pupils, weakening of their reaction to light, reflexes of oral automatism, etc.), narrowing of blood vessels in the fundus; changes in the psyche manifest themselves in the form of increased irritability, absent-mindedness, emotional instability, decreased memory, patients forget first and last names, have great difficulty remembering new things, but remember the past well, begin to resort to recording errands, telephone numbers, etc. Sometimes they It can be difficult to immediately remember the date of an event from public or personal life, but after a certain period of time they name it correctly. At first, memory impairments are episodic in nature, especially worsening with physical fatigue and emotional stress. Typically, such memory disorders are so shallow that only the patients themselves notice them, while those around them either do not notice these disorders at all or do not attach much importance to them. Gradually, memory disorders increase: it is increasingly difficult to assimilate new things, repeated repetitions are required to retain newly acquired knowledge and experience in memory. For a minor reason, patients experience a sharp emotional reaction in the form of incontinence, short temper, irritability, and anger. Weakness appears: patients become hypersensitive over every trifle (with good news, cheerful music, they begin to cry, etc.). Plasma hypercholesterolemia is noted. Strict parallelism between atherosclerosis of cerebral vessels and atherosclerosis of the cardiovascular system, as a rule, is not observed. In some cases, initial atherosclerosis must be differentiated from a neurasthenic syndrome of another etiology. In favor of atherosclerosis are the elderly age of patients, characteristic memory disorders, weakness, the presence of mild organic neurological symptoms in the form of positive reflexes of oral automatism, sometimes pathology in the fundus, and increased cholesterol in the blood. Despite the fact that atherosclerosis of cerebral vessels tends to have a slowly progressive course, with the necessary treatment, diet therapy, proper organization of regimen and rest, the process can be delayed in development for a long time and even the reverse development of a number of pathological symptoms is possible. In case of progression, the next stage develops—moderate atherosclerosis. It is characterized by an increase in memory disorders: it is increasingly difficult to assimilate new things, repeated repetitions are required to retain newly acquired knowledge and experience in memory. Efficiency decreases, more and more time is spent on performing one’s duties than it was before the illness. Emotional disturbances and weakness are increasing. At this stage, the process is still relatively compensated, but deterioration of the condition is periodically noted due to fatigue and anxiety. Malnutrition of brain cells due to the sclerotic process gradually causes a deterioration in intellectual functions and a decrease in criticism. Sclerotic changes in blood vessels are noted in the fundus. Neurological organic symptoms increase: reflexes of oral automatism are expressed, bilateral pyramidal signs appear.
Severe atherosclerosis of cerebral vessels is characterized by the presence of gross organic changes in cerebral vessels, leading to chronic cerebral vascular insufficiency, which also causes a more severe clinical picture of the disease. There are significant disorders of memory and the emotional sphere, behavioral disorders are becoming more and more pronounced. Patients become verbose, obsessive, picky, selfish, they begin to get stuck on little things, and their range of interests gradually narrows. Patients find it difficult to perform even their usual duties, and the development of a new stereotype becomes impossible. Debility sharply increases, criticism decreases, the range of needs and interests decreases, and the ability to work is permanently impaired. Objectively, organic symptoms of a scattered nature are detected, when the subcortical nodes are involved in the process, and extrapyramidal symptoms appear. Repeated transient disorders of cerebral circulation often occur, in some cases ending in a stroke (usually ischemic), after which persistent focal or general cerebral disorders and sometimes a combination of both remain.
In the initial stage of atherosclerosis of the cerebral vessels, due to the difficulty of switching attention, slowing down of mental processes, and increased fatigue, patients are unable to work associated with significant and constant neuropsychic stress, work of large volume, requiring quick decisions, frequent switching of attention. Due to the vascular nature of the process, significant physical stress, exposure to high temperatures, and intense thermal radiation are contraindicated.
Due to their extensive professional experience and skills, patients often cope with their usual work and rarely have sick leave. However, in order to prevent the progression of the disease, it is advisable for them to create easier working conditions in the form of a reduction in the amount of work, freedom from additional loads, and night shifts. A rational regime of work and life, cessation of smoking and alcohol abuse are of great importance. Spa treatment is recommended. In the initial stage of cerebral atherosclerosis, indications for referral to VTEC rarely arise; a work recommendation should be issued by the medical unit or medical institution.
With atherosclerosis of moderate severity, when significant memory disorders, mental rigidity, and severe emotional disorders are detected, the patients’ ability to work is significantly limited. Work that requires a fast pace, a large amount of attention, and significant and even unstable neuropsychic stress is inaccessible to them. However, in these cases, the restructuring of the dynamic stereotype is especially difficult, and therefore it is recommended to leave patients at their previous work while creating significantly easier work conditions: a significant reduction in the amount of work, changing the work regime with the possibility of arbitrary breaks for rest, liberation from additional loads, reducing the number of serviced units, exemption from night shifts, travel, business trips. With extrapyramidal tremors, work that requires subtle and precise movements is not possible. These contraindications are often the basis for establishing disability group III.
With severe atherosclerosis of the cerebral vessels, patients are usually unable to work, either due to pronounced organic changes in the psyche, or due to the severe consequences of a cerebral stroke (More details in the article Medical and labor examination for cerebral stroke).
What to pay attention to
When atherosclerosis is diagnosed, disability does not occur immediately. The insidiousness of the disease is that in its first stages, patients feel quite well and do not feel discomfort. The onset of pathology will help to identify:
- Biochemical blood test containing data on excess triglycerides and LDL (low-density lipoproteins).
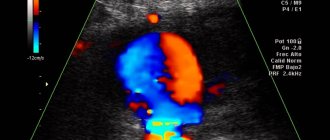
- Hardware ultrasound examination of blood vessels, which reveals fatty streaks on the inner walls of the arteries.
Later, as the vascular lumen becomes clogged with atherosclerotic plaques, patients come to doctors with complaints of the following symptoms:
- Changes in skin color on the injured leg, paleness, and sometimes a bluish tint.
- Reduced temperature of the diseased limb, the leg clearly feels colder to the touch than the healthy one.
- Loss of sensitivity, goosebumps, as if the patient had a leg injury.
- At night, patients experience cramps.
- After walking or other physical activity, pain in the legs begins, which goes away after rest, and in chronic stages it does not disappear even at night.
A person may be bothered by some of the listed symptoms or all of them together. The latter option is more common when the patient is already on the verge of a stroke or heart attack.
With severe development of vascular atherosclerosis, associated with a heart attack, stroke or irreversible changes in the vessels of the extremities, patients lose the ability to work and normal life, which means permanent disability. As a rule, they cannot care for themselves and need household and medical care.
Considering the severity and irreversibility of the disease, patients are interested in an important question: when diagnosed with atherosclerosis, is a group given?
We hasten to reassure you: the ITU (medical and social examination), having established the degree of development of the disease, will give a disability group and determine the directions of therapy most suitable for maintaining a stable condition of the patient and stopping further progression of the disease.
Disability due to cerebrosclerosis
This disease is considered the most common in our time. And with atherosclerosis of the cerebral vessels, the entire body suffers. The main danger of such a disease is that it is asymptomatic, as a result of which it is not always possible to identify the disease in the early stages and prevent disability of the patient.
In addition, among the causes of death, cerebral atherosclerosis occupies one of the first places in the world. With this pathological condition, the patient becomes disabled not because of the vascular damage itself, but due to the development of complications, which, in the absence of appropriate treatment and prevention, very soon begin to appear.
The patient may become disabled if vascular stenosis is detected, in which even the slightest overexertion can lead to a stroke and other serious consequences. The likelihood of such a development will depend on the state of the patient’s immune system, genetic predisposition and existing risk factors. If the patient is not under constant medical supervision, the disease will only progress.
With the development of cerebrosclerosis, a disability group is assigned in the following cases:
- with the development of a microstroke;
- in case of development of acute coronary blood flow disorder;
- in case of aortic stenosis and aneurysm.
Each of these diseases is difficult to treat and, in its advanced form, leads to disability of the patient. After a stroke, the patient becomes unable to work due to paralysis of the limbs, decreased activity, and reduced brain capacity. Disability registration for patients is carried out based on the results of a medical and social examination.
Group registration procedure
In case of atherosclerosis of the vessels of the lower extremities, disability is given based on the patient’s condition, the nature and degree of deterioration of his health during the development of the disease, including after amputation of a limb.
To assign a person disabled status, doctors study a combination of the following data:
- Duration of illness.
- Age parameters.
- Ability to move without assistance.
- The degree of arterial occlusion and ischemic damage to the extremities.
- The presence of other chronic ailments and possible complications.
Those patients from whom a limb was taken away due to gangrenous changes caused by atherosclerosis are given disability even before the prosthesis is ready. In the absence of other complications, such patients are assigned to the third group.
Atherosclerosis of the legs and disability
In case of disability due to atherosclerosis of the lower extremities, several groups are possible. And this development of complications of the disease is provoked by the lack of timely treatment.
But we cannot write off the fact that the patient who has such individual characteristics of the body and genetic predisposition is at risk of getting disability and complications. If the condition of a sick person is not controlled by the attending physician, then further development of the pathology cannot be avoided. And this is fraught with the most serious consequences. With the development of the disease, such pathologies as microstroke and stroke, obliterating atherosclerosis, myocardial infarction, aneurysm and aortic stenosis make it possible to determine disability.
In turn, with the development of a stroke, the patient may become disabled due to obliterating atherosclerosis. The latter implies paralysis or paresis of the lower extremities as a result of damage to the vessels of the lower extremities. If you do not treat the disease and ignore its symptoms, it can ultimately lead to leg amputation.
Labor restrictions
Patients who have suffered severe atherosclerosis of the extremities, including those associated with amputation, are prohibited from working in positions that involve:
- Heavy or moderately difficult working conditions.
- Work that requires a long static position.
- Conditions associated with prolonged psycho-emotional or energy stress.
- Work in rooms/areas with high humidity or low temperature climate.
- Harmful production, constant work with toxic chemicals or in radioactive conditions.
Need to assign a group
Patients, when it is determined that a disability can be assigned, are referred for the following types of research:
- General and biochemical blood tests to identify the inflammatory process and the ratio of “good”, “bad” cholesterol in the blood and some other indicators.
- Rheovasography.
- Doppler scanning of blood vessels.
- Coagulogram is a blood test that reveals its increased coagulability.
MSE is carried out in the following cases:
- If the patient has undergone surgery, the prognosis is encouraging and it is necessary to determine the further direction of therapy.
- The patient needs to be transferred to an easier job.
- The prognosis for the further development of the disease is negative, the patient needs to be assigned disability group 1 or 2.
- When conservative or surgical therapy does not bring the expected results and the patient’s condition continues to deteriorate.
- The patient is provided with a specialized car.
- It is necessary to put the patient under examination to establish the cause of such a serious condition.
Carotid artery surgery reviews
In the future, constant medical observation is necessary for the rehabilitation of the patient. As well as control examinations for the recurrence of atherosclerotic plaques or stenosis. The examination is carried out at least twice a year. Blood pressure of patients who have undergone such surgery must be measured every day.
Surgery for pathological tortuosity is performed under local anesthesia or general anesthesia. The choice of anesthesia method in our clinic depends on the volume of the upcoming operation. We prefer to perform this operation under local anesthesia, as it makes it possible to determine the brain's response to temporary compression of the carotid artery.
In these cases, patients are recommended to change their place of work to reduce the negative impact on the nervous system and the body as a whole.