What does high cholesterol mean and threaten in women?
Elevated cholesterol levels in women may be evidence of metabolic syndrome (poor nutrition plus a sedentary lifestyle), simply poor nutrition (prevalence of fatty foods in the diet, but only 20% of cholesterol in the blood depends on nutrition, the rest is synthesized by the liver), obesity and (or ) diabetes mellitus.
Registration of elevated cholesterol levels (or cholesterol is its other name) means that it is necessary, first of all, to reconsider your lifestyle: move more and eat less fatty foods, giving preference to plant foods and lean meats and fish. You may need to take statins.
See also:
Treatment with folk remedies for high cholesterol
Folk remedies for cholesterol plaques
How to fight cholesterol plaques
High cholesterol in women threatens the development of diseases such as atherosclerosis (massive deposition of cholesterol plaques on the internal surfaces of blood vessels - there are no drugs that would break down atherosclerotic plaques), angina pectoris (essentially the same atherosclerosis, only in the coronary vessels, i.e. vessels feeding the heart itself). The development of these two diseases - atherosclerosis and angina - often results in heart attacks and strokes, and they themselves reduce the quality of life, for example, shortness of breath appears, endurance decreases, etc.
What does high cholesterol affect in women?
Elevated cholesterol levels primarily affect the amount of deposits (cholesterol plaques) on the inner surfaces of blood vessels. The process of development of atherosclerosis, of course, is more complex and is influenced not only by the level of LDL - modern medicine rather considers the inflammatory nature as the main one (after all, plaques appear in places where a blood vessel is damaged, as a “patch”).
Is high blood cholesterol dangerous in women?
The hypothesis about the danger to human life of elevated cholesterol levels appeared at the beginning of the 20th century, when N. Anichkov conducted an experiment with the introduction of a saturated and concentrated solution of cholesterol into the digestive system of rabbits. As a result, cholesterol deposits began to appear on the walls of the animals' blood vessels. However, with the return of a normal diet, the condition of the blood vessels also returned to normal. Subsequent experiments on dogs did not confirm this observation, i.e. In herbivores, additional cholesterol was deposited in the blood vessels, while in carnivores it was not. Man is an omnivore, so the results of Anichkov’s experiments are now considered questionable, and the development of atherosclerosis is associated not so much with the level of cholesterol in the blood (although this is a necessary but not sufficient condition), but with the development of inflammatory processes in the arteries.
Hypercholesterolemia - symptoms and treatment
The main goal in treating hypercholesterolemia is to prevent serious complications or at least reduce their risk.[8] This is achieved through the intermediate goal of correcting cholesterol levels in the blood, as well as by influencing other known risk factors for atherosclerosis.
When the cholesterol level in the blood is normalized and its concentration is maintained in the optimal range for a long time, the risk of myocardial infarction, stroke, and death from cardiovascular causes gradually decreases. Therefore, it is so important to maintain an optimal concentration of cholesterol in the blood (primarily “bad”) for as long as possible, ideally for life.
Of course, in many cases, changing lifestyle alone is not enough for this, especially since few people manage to maintain a healthy lifestyle for a long time - there are too many temptations along the way.
If there is a high risk of cardiovascular complications, medications that reduce the level of “bad” cholesterol must be prescribed, regardless of the patient’s intention to improve their lifestyle.
Currently, cardiology has abandoned the concept of “normal cholesterol levels”. Instead, the term “optimal cholesterol level” is used, and what it will be depends on the total cardiovascular risk. Based on the data obtained about the patient, the doctor calculates this risk:
- If the risk is very high (and this is, for example, all patients who already have coronary heart disease or have suffered an ischemic stroke, suffer from diabetes mellitus and a number of other categories), then the optimal level for “bad” cholesterol will be less than 1.8 mmol /l.
- At high risk (if the patient does not yet have atherosclerotic cardiovascular diseases, but he has several risk factors, for example, a smoking hypertensive man of 50 years with a cholesterol level of 6 mmol/l will have a high cardiovascular risk) the optimal value for " bad cholesterol will be less than 2.6 mmol/l.
- For everyone else who is not at high or very high cardiovascular risk, the optimal low-density lipoprotein cholesterol ("bad" cholesterol) value is less than 3.0 mmol/L.
If there is a genetic “damage” behind hypercholesterolemia, then lifestyle changes (diet, physical activity, smoking cessation) can only improve the biochemical composition of the blood to a limited extent, so additional drug therapy must almost always be resorted to.
What lifestyle changes can lower cholesterol and reduce the risk of heart disease?
First of all, this:
- reducing consumption of foods such as fatty meats, fatty dairy products, confectionery and sweets;
- complete cessation of smoking;
- reduction in body weight by at least 10% from the original, if there is overweight and obesity;
- increasing physical activity - fairly intense physical activity at least 4-5 times a week for 30-40 minutes, which requires effort (for example, running, cycling, outdoor sports games, swimming, etc.), including housework in this regard is not considered suitable physical activity.
All of these measures not only change the lipid composition of the blood for the better, but can also significantly reduce the risk of cardiovascular diseases associated with atherosclerosis (myocardial infarction, stroke, angina pectoris and others).
Drug therapy
The main drugs used to reduce cholesterol levels and its associated cardiovascular risks are statins. The first statins were obtained, like the first antibiotics, from mold cultures. The next generations of statins appeared thanks to chemical synthesis.
Statins are perhaps the most well-studied drugs in the history of medicine and also some of the safest.[9] This group of drugs inhibits the synthesis of cholesterol in the liver (yes, most of the cholesterol is formed inside us and does not come from outside). The liver, needing cholesterol primarily for the synthesis of bile acids, begins to more actively extract cholesterol from the blood as part of low-density lipoproteins, as a result of which gradually, over the course of a month or two, the concentration of cholesterol in the blood decreases and can decrease by 50% from the previous level with a sufficient dose of statin. The results of numerous clinical studies involving many thousands of patients provide convincing evidence of the ability of this group of drugs not only to reduce blood cholesterol levels, but also, more importantly, to seriously reduce the risk of myocardial infarction and stroke, and most importantly, to increase the life expectancy of patients with cardiovascular diseases (primarily those who have had myocardial infarction, as well as people with other forms of coronary heart disease).
Using intravascular ultrasound, the ability of statins, when taken regularly for at least two years, has been proven to stop the development of atherosclerosis and even reduce the size of atherosclerotic plaques.
It is important that, if there are indications for their use, treatment with statins is carried out in sufficient doses and for a long time - for a number of years. The usual doses in modern cardiology are 40-80 mg of atorvastatin and 20-40 mg of rosuvastatin. These are the two most effective modern drugs of this class.
The “gold standard” are the original drugs of the development companies - Crestor (rosuvastatin from AstraZeneca) and Liprimar (atorvastatin from Pfizer). The remaining statin drugs containing rosuvastatin or atorvastatin are generic copies and must demonstrate their equivalence to the original drugs in clinical trials. Many generic drugs do not have such confirmation of their effectiveness and safety, and their use can sometimes be disappointing. The advantage of generics is their lower cost.
Another drug that lowers the level of “bad” cholesterol in the blood is ezetimibe. It blocks the absorption of cholesterol in the intestinal lumen and is usually prescribed in addition to statins if they do not allow one to achieve optimal cholesterol levels in monotherapy. Ezetimibe itself allows you to reduce the level of “bad” cholesterol by 15-20% of the original level, i.e. inferior in this regard to statins.
A new class of drugs that has surpassed statins in their ability to lower bad cholesterol is the so-called cumabs, which are antibodies to a regulatory protein responsible for regulating the rate at which cholesterol is absorbed from the blood.[11] True, these drugs are very expensive (treatment costs 30-40 thousand rubles per month). But there are situations when this is literally necessary to save a life, when otherwise the patient may not survive the next five years due to myocardial infarction or stroke. In addition, this new class of drugs is used to treat patients with familial hypercholesterolemia in cases where the maximum dose of statin therapy in combination with ezetimibe is still very far from achieving optimal cholesterol levels.
How to reduce blood cholesterol in women?
The most effective, but not the safest way is to take statins. In high concentrations, the latest generation of drugs can reduce cholesterol levels in women by 50–55%. However, statins have a lot of side effects: from very rare, but extremely dangerous, for example, rhabdomyolysis (destruction of muscle tissue), to simple, but quite common, such as malaise and weakness.
See also:
Cholesterol plaques in blood vessels, their treatment
Aspirin for atherosclerosis
Cholesterol prevention with folk remedies
With relatively low levels of excess LDL cholesterol (5.5 – 6.5 mmol/l), doctors try to prescribe more conservative treatment methods than taking medications: increasing physical activity (reduces LDL levels and increases HDL concentrations, quitting smoking and alcohol abuse (although 1 serving of alcohol - preferably red wine - on the contrary, increases the level of HDL, more details: alcohol and vascular atherosclerosis), changing the diet.
Cholesterol norm
The normal levels of cholesterol in the blood are determined separately for women and men, and also depend on the person’s age. The established standards were adopted on the basis of scientific analysis of the results of laboratory tests of a large number of patients. The cholesterol level can fluctuate in the range of 3.6-7.8 mmol/l. However, doctors say that any cholesterol level above 6 mmol/l is considered elevated. Many patients taking a cholesterol test already have chronic diseases, especially for older people, so only a specialist can determine the individual norm.
A blood test determines:
- High density lipoproteins.
- Low density lipoproteins.
- Total cholesterol level.
- Triglycerides.
What factors influence high cholesterol levels?
If a person did not experience health problems at a young age, this does not mean that they cannot appear after menopause. This condition is more discussed as one of the life cycles of a woman, however, in men there is also an age when the hormonal background changes significantly and the whole body begins to work differently. Therefore, with the onset of your 40th birthday, medicine recommends being more attentive to your body and undergoing timely preventive examinations.
Poor nutrition is the main factor affecting cholesterol levels. The lack of fresh plant foods in the daily diet does not allow the intestines to be cleansed and freed from toxins and other harmful substances. Blood, due to the predominance of fatty and animal foods, becomes thicker, losing its rheological properties. As a result, its ability to nourish tissue cells, including oxygen, decreases. Cholesterol builds up on the walls of blood vessels, trying to block the lumen.
How to lower cholesterol through nutrition?
Cholesterol can be reduced with proper nutrition
If a high concentration of bad cholesterol is detected in the blood, it is necessary to find out the cause of the condition. Sometimes the problem is associated with certain diseases that need to be treated with medication.
If the condition is caused by diet, a healthy diet can help restore lipid balance. When compiling a diet, you should pay attention to substances that indirectly affect cholesterol levels in the body.
The intake of the following substances into the body should be minimized:
- Trans fats. Found in snack foods, baked goods, cookies, crackers, chips, margarine and some processed foods.
- Salt. The body cannot function without salt, but abuse of this supplement negatively affects the state of the cardiovascular system.
- Sugar. Simple carbohydrates are a source of energy for cells, but their intake must meet the body's needs. Excess sugar in the body increases the risk of obesity and diabetes.
- Other substances, on the contrary, reduce the content of bad cholesterol in the body, so foods containing them should be included in the diet.
Beneficial substances include:
- Omega-3 fatty acids. These substances have a positive effect on the lipid profile.
- Soluble dietary fiber. These substances bind bad cholesterol and remove it from the body along with the stool.
The following products contain the listed substances:
- Fish: salmon, trout and tuna.
- Nuts, seeds and beans.
- Fruits: oranges, peaches, tangerines, apples.
- Green vegetables.
- Natural vegetable oils: olive oil, avocado oil.
- Oats and oat bran.
- Flaxseeds.
- Brussels sprouts.
- Soy products.
There are also drinks that can help lower cholesterol. These drinks include:
- Green tea. It contains antioxidants known as polyphenols. These substances help reduce the concentration of low-density lipoproteins in the blood. In addition, polyphenols stimulate the excretion of bad cholesterol in the stool.
- Berry juice. The most beneficial juices are those made from blackberries, cherries, red raspberries, blueberries and strawberries.
- Ginger tea. Regular consumption of this drink not only has a positive effect on the lipid profile, but also improves the condition of the digestive system.
Studying product labels before purchasing them will help determine the content of beneficial and harmful substances.
What to do if you have high cholesterol
Depending on how high the cholesterol level has become, the doctor determines treatment tactics. In the initial stages, it is recommended to adjust the daily diet and add mandatory physical activity. Morning exercises are not an active pastime. It is important to go for a run every day. It's better if it's jogging in the fresh air. If it is not possible to do physical education classes on the street, you can organize full-fledged classes in an apartment. But they will definitely have to be supplemented with a walk. When getting to work, you can walk a couple of public transport stops - this will be an excellent alternative to jogging.
Overweight people should strive to bring their body mass index back to normal. To do this, it is necessary to adjust the daily menu, supplemented by restrictions on portion sizes. People at risk, for example, those suffering from diabetes, may be prescribed medication as an addition to mandatory lifestyle correction.
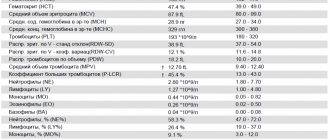
Diagnostics and tests
To establish why cholesterol has increased, a comprehensive examination of the body is necessary. To determine the level of lipophilic alcohol, after collecting anamnesis, auscultation and measuring blood pressure, the following laboratory diagnostic methods are prescribed:
- blood chemistry;
- lipid profile study;
- immunological analysis.
If you want to identify a genetic defect that may be causing high cholesterol, you may need to donate blood to test the patient's relatives.
Why is high cholesterol dangerous?
An increased level of “bad” cholesterol in the blood contributes to the formation of atherosclerotic plaques and the development of atherosclerotic damage to the walls of blood vessels. With the development of atherosclerosis, the main function of the vessels that deliver blood to each cell is disrupted, providing nutrition to the whole body. The consequences depend on the location of the largest accumulation of plaques:
- Cerebral vessels - a violation of cerebral circulation, which leads to stroke and cognitive impairment.
- Heart vessels - angina pectoris, heart attack, hypertension.
- Renal vessels – chronic renal failure.
- Retinal vessels – decreased vision.
- Intestinal vessels - thrombosis, colic.
- Vessels of the lower extremities - gangrene, necrosis.
People at risk include:
- Those with a genetic predisposition (close relatives with atherosclerosis and cardiovascular diseases).
- Overweight.
- With high blood pressure.
- With type 2 diabetes.
- Leading a sedentary lifestyle.
- Eating “junk” food.
- Having bad habits - smoking, alcohol.
- Men over 35 years old.
- Women who have been taking hormonal contraceptives for a long time and women in menopause.
Changes in cholesterol levels over the years in men
Men are naturally protected from atherosclerosis less than women. They do not have a high level of estrogen in the body, but they have a higher craving for bad habits that increase the risk of dangerous diseases.
Norms of total cholesterol in men:
- up to 5 years: from 2.95-5.25 mmol/l;
- 5-10 years: from 3.13 to 5.25 mmol/l;
- 10-15 years: from 3.08 to 5.23 mmol/l;
- 15-25 years: from 2.93 to 5.59 mmol/l;
- 25-35 years: from 3.44-6.58 mmol/l;
- 35-40 years: from 3.78-6.99 mmol/l;
- 40-50 years: from 3.91 to 7.15 mmol/l;
- 50-60 years: from 4.09 to 7.17 mmol/l;
- 60-70 years: from 4.12 to 7.15 mmol/l
- 70 years or more: from 3.73 to 7.86 mmol/l.
The closer the cholesterol level is to the lower limit of normal, the safer it is for blood vessels and the heart. Regular levels exceeding 5–6 mmol/l signal the need to prevent atherosclerosis. It is especially important to monitor indicators for men over 50 years of age. From this age their growth accelerates.