Low-density lipoproteins are the main carriers of cholesterol (cholesterol) in the body. The cholesterol they contain is considered “harmful”, since its excess increases the risk of plaques appearing in the arteries, which can lead to blockage and cause a heart attack or stroke.
Synonyms Russian
LDL, low-density lipoprotein, LDL, LDL-C, low-density lipoprotein cholesterol, beta-lipoprotein cholesterol, beta-lipoprotein, beta-LP.
English synonyms
LDL, LDL-C, low-density lipoprotein cholesterol, Low-density lipoprotein.
Research method
Colorimetric photometric method.
Units
mmol/l (millimoles per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress and do not smoke for 30 minutes before the test.
General information about the study
Cholesterol (CH, cholesterol) is a fat-like substance vital to the body. The correct scientific name for this substance is “cholesterol” (the ending -ol indicates that it belongs to alcohols), however, the name “cholesterol” has become widespread in the popular literature, which we will use later in this article. Cholesterol is involved in the formation of cell membranes of all organs and tissues of the body. Cholesterol is used to create hormones that are necessary for the development of the body and the reproduction function. Bile acids are formed from cholesterol, with the help of which fats are absorbed in the intestines.
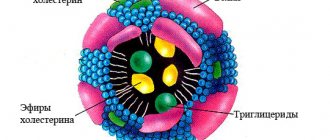
Cholesterol is insoluble in water, so to move around the body it is “packed” into a protein shell consisting of apolipoproteins. The resulting complex (cholesterol + apolipoprotein) is called lipoprotein. Several types of lipoproteins circulate in the blood, differing in the proportions of their components:
- very low density lipoproteins (VLDL),
- low density lipoproteins (LDL),
- high density lipoproteins (HDL).
LDL cholesterol is considered “bad” because when it is in excess, plaques appear in the walls of blood vessels, which can restrict the movement of blood through the vessel, which threatens atherosclerosis and significantly increases the risk of heart disease (coronary artery disease, heart attack) and stroke.
The liver produces enough cholesterol for the body's needs, but some of it comes from food, mainly fatty meat and fatty dairy products. If a person has a genetic predisposition to high cholesterol or eats too much animal fat, LDL levels in the blood can rise to dangerous levels.
What is the research used for?
- To assess the likelihood of atherosclerosis and heart problems (this is the most important indicator of the risk of developing coronary disease).
- To monitor the effectiveness of a diet with a reduced amount of animal fats.
- To monitor lipid levels after taking cholesterol-lowering medications.
When is the study scheduled?
An LDL test is usually part of a lipid profile, which also includes the determination of total cholesterol, VLDL cholesterol, HDL cholesterol, triglycerides and atherogenicity coefficient. A lipidogram may be prescribed during routine preventive examinations or when the concentration of total cholesterol increases, in order to find out which fraction is responsible for the increase.
In general, a lipid profile is recommended for all people over 20 years of age at least once every 5 years, but in some cases even more often (several times a year). First, if the patient is prescribed a diet limited in animal fats and/or is taking cholesterol-lowering medications, then it is checked whether he achieves the target level of LDL and total cholesterol and, accordingly, whether his risk of cardiovascular disease is reduced diseases. And, secondly, if the patient has one or more risk factors for developing cardiovascular diseases in his life:
- smoking,
- certain age (men over 45, women over 55),
- high blood pressure (from 140/90 mm Hg),
- high cholesterol or cardiovascular disease in family members (heart attack or stroke in a close male relative under 55 years of age or a female relative under 65 years of age),
- coronary heart disease, previous myocardial infarction or stroke,
- diabetes,
- excess body weight,
- alcohol abuse,
- eating large amounts of food containing animal fats,
- low physical activity.
If a child in the family had cases of high cholesterol or heart disease at a young age, then it is recommended that he take a lipid profile for the first time between the ages of 2 and 10 years.
What do the results mean?
Reference values:
The concept of “normal” is not entirely applicable to the level of LDL cholesterol. Different people with different numbers of risk factors in their lives will have different LDL levels. LDL cholesterol testing is used to determine the risk of cardiovascular disease, but to accurately determine it for any person, all factors must be taken into account.
Elevated LDL cholesterol levels may be the result of a hereditary predisposition (familial hypercholesterolemia) or excess dietary intake of animal fats. In most people with high cholesterol, both factors are involved to some extent.
According to clinical guidelines1, the level
“Diagnostics and correction of lipid metabolism disorders for the purpose of prevention and treatment of atherosclerosis. Russian recommendations, VII revision. 2020".
"2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk."
Possible causes of elevated LDL cholesterol levels:
- cholestasis - stagnation of bile, which can be caused by liver disease (hepatitis, cirrhosis) or gallstones,
- chronic inflammation of the kidneys leading to nephrotic syndrome,
- chronic renal failure,
- decreased thyroid function (hypothyroidism),
- poorly treated diabetes mellitus,
- alcoholism,
- obesity,
- prostate or pancreatic cancer.
Reduced LDL cholesterol levels are not used in diagnosis due to low specificity. However, its reasons may be:
- hereditary hypocholesterolemia,
- severe liver disease,
- oncological diseases of the bone marrow,
- increased thyroid function (hyperthyroidism),
- inflammatory joint diseases,
- B12 or folate deficiency anemia,
- common burns,
- acute diseases, acute infections,
- chronic obstructive pulmonary disease.
What can influence the result?
Cholesterol concentrations may change from time to time, this is normal. A single measurement does not always reflect normal levels, so sometimes it may be necessary to retake the test after 1-3 months.
Increases very low-density lipoprotein cholesterol levels (VLDL cholesterol):
- pregnancy (lipid profile should be done at least 6 weeks after birth),
- long fasting,
- donate blood while standing,
- anabolic steroids, androgens, corticosteroids,
- smoking,
- eating food containing animal fats.
Reduce VLDL cholesterol levels:
- being in a lying position,
- allopurinol, clofibrate, colchicine, antifungal drugs, statins, cholestyramine, erythromycin, estrogens,
- intense physical activity,
- a diet low in cholesterol and saturated fatty acids and, conversely, high in polyunsaturated fatty acids.
Simvastatin and ezetimibe
The first fixed combination of a statin and ezetimibe was a combination based on simvastatin. Simvastatin 10–40 mg/day reduces LDL-C levels by 18–41% less than atorvastatin or rosuvastatin [17], which limits its use in cases where achieving current LDL-C targets is required. The bioavailability of simvastatin is about 5%, the half-life is approximately 1–3 hours [18]. In general, the drug is well tolerated; increased levels of liver transaminases occur in 1% of patients [19].
Ezetimibe lowers LDL-C levels by blocking the absorption of cholesterol in the small intestine and increasing the excretion of cholesterol into the bile. Many studies have repeatedly demonstrated the synergistic effect of prescribing statins and ezetimibe [22–24].
The effectiveness of therapy with ezetimibe and simvastatin was shown in the randomized, double-blind, placebo-controlled study IMProved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT). The study design was based on a comparison of simvastatin monotherapy (40 mg) and combination therapy of simvastatin and ezetimibe (40+10 mg) in patients after myocardial infarction. In the combination therapy group, the achieved LDL-C level was significantly lower (53.7 mg/dL versus 69.5 mg/dL in the monotherapy group). A reduction in the number of heart attacks and strokes in the combination therapy group was also demonstrated (p < 0.05) [25]. Also interesting are the results of a 2017 study, which showed that the protective effect of combination therapy was higher in the group with GFR less than 45 ml/min/1.73 m2 [26].
Concomitant use of simvastatin and ezetimibe did not increase the risk of developing side effects of statins—myopathy and increased levels of hepatic transaminases [27]. Moreover, the combination was shown to not increase the risk of developing type 2 diabetes, which is sometimes observed with high-dose statin therapy [28, 29].
Atorvastatin and ezetimibe
Atorvastatin at a dose of 10–80 mg/day reduces LDL-C levels by 37–51%, reduces the risk of cardiovascular and cerebrovascular complications, and has demonstrated its effectiveness in both primary and secondary prevention in a series of clinical studies and meta-analyses [30 ].
A meta-analysis including 17 studies showed that combination therapy with atorvastatin and ezetimibe reduced LDL-C and triglyceride levels and increased HDL-C levels (p < 0.05) [31]. Combination therapy has demonstrated a reduction in coronary atherosclerosis, as assessed by intravascular ultrasound, compared with atorvastatin monotherapy [32]. Studies have shown comparable rates of adverse reactions with combination therapy with atorvastatin and ezetimibe and monotherapy with atorvastatin or ezetimibe, with isolated cases of increased liver transaminases, the development of myopathy, or bowel irritation [33].
Prospects for combination therapy using ezetimibe
Bempedoic acid is a new generation lipid-lowering drug that can reduce LDL-C levels by 40%. Bempedoic acid is a prodrug that is converted in the liver to bempedoic acetyl-coenzyme A, which is an inhibitor of the enzyme ATP-citrate lipase. According to its mechanism of action, this drug not only reduces LDL-C levels, but also blocks the synthesis of fatty acids [40–42].
The combination of bempedoic acid (120 or 180 mg/day) and ezetimibe (10 mg/day) in patients with statin intolerance and in those who could receive statin therapy led to a decrease in LDL-C levels by 43.1% and 47.7 % respectively, depending on the dosage of the drug. Monotherapy with bempedoic acid reduces LDL-C levels by 27.5% and 30.1% (corresponding to the indicated dose) and is well tolerated [43]. In a phase III clinical trial, adding this drug to statin and ezetimibe therapy in patients at high and very high CVD risk reduced LDL-C levels by 28% and CVD risk by 33% [44]. The combination of bempedoic acid and ezetimibe continues to be investigated as a promising combination.