Of all types of injuries, TBI is perhaps the most common, especially in childhood, when “adult” proportions have not yet been determined, and when a fall occurs, the head pulls the body down and suffers first. Any blow to the head is perceived as a serious injury, even if at first glance everything is in order. People near a fallen child immediately begin to look for signs of a concussion in the child, so that if necessary, they can quickly call an ambulance.
A concussion can also be caused by landing on the buttocks, so TBI is often accompanied by other injuries to the body.
(chest, lower leg, pelvis) and are less often isolated. The only question here is which organ needs to be saved first? But the head is always important, therefore:
Even a mild concussion requires a thorough examination in a hospital setting in order to determine the real harm to health and prevent possible consequences.
Concussion is one of the forms of TBI
Usually, by concussion, people mean any traumatic brain injury, and this, of course, cannot be reproached, since all these TBIs are the competence of doctors. In medical circles, a concussion is a mild form of traumatic brain injury.
which is not characterized by focal neurological symptoms, there are no signs of vascular damage, and the functional disorders that follow the injury are reversible. However, taking into account the readers’ interest not only in this form of pathology, we will try to stop and explain the essence of those head injuries that are popularly considered to be a concussion, since everyone interprets this term in their own way and is often confused with the concept of a brain contusion or the formation of an intracranial hematoma from compression.
As experience shows, each of us may find ourselves in a situation where determining the degree of damage becomes very important, since not only a person’s life, but also its quality in the future often depends on it. Symptoms of a concussion can range from few to very varied, depending on the force of impact or the strength of the person's head.
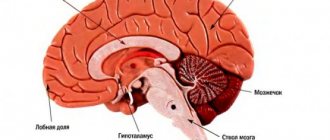
Thus, a concussion is the result of the shaking of a soft substance and its impact on the hard skull,
within which it is located. As the brain moves to the bones of the skull, the cells (their processes) stretch and experience some discomfort, which affects their functional abilities, which are temporarily lost.
Doctors have still not come to a consensus on what actually happens in the head at the moment of impact, so there are several versions of possible events that throw the central nervous system out of its normal rut:
- Neurons lose connection with each other.
- Disturbances in the nervous tissue of the brain occur at the molecular level.
- A sharp spasm of microcirculatory vessels makes it difficult to nourish the brain.
- Imbalance of interaction between the cortex and other brain structures.
- Changes in the chemical composition of cerebrospinal fluid.
- Short-term increase in intracranial pressure due to physicochemical disorders and colloid imbalance.
- Disruption of the movement of cerebrospinal fluid, which, upon impact, leaves the cavities of the ventricles of the brain and is directed into the interventricular spaces.
Which of these hypotheses is probably correct is probably not for us to judge, but the important thing is that they all agree on one thing - with SHM, reversible functional disorders occur, but the brain structures do not suffer, and no morphological changes are noted in them. The veracity of this statement is also evidenced by data from computed tomography, which is usually prescribed for head injuries.
Diagnostic methods
To determine the nature and extent of disorders, methods such as CT and MRI are used. During a diagnostic CT study, abnormalities are detected - areas of hemorrhage, damage to parenchyma (nervous tissue), fractures of the bone structures of the skull. Computed tomography is considered the most informative method for identifying indications for emergency surgery.
Other advantages of CT: the ability to examine patients in a state of psychomotor agitation, and quick results. Neuroimaging is mandatory for patients:
- Children under 16 years of age.
- Patients with signs of intoxication.
- Patients with a blurred, erased clinical picture.
- Patients taking anticoagulants on an ongoing basis (as part of a program for the treatment of chronic vascular pathologies).
With a mild concussion, changes in the structure of the brain matter are detected in 15% of cases. If, during the initial examination of the patient, neurological symptoms of a focal type are observed, morphological changes in the nervous tissue are detected with a frequency of 50% of cases.
An MRI study is more sensitive to detecting axonal damage of a diffuse type, changes in the structure of the parenchyma, and hematomas of subdural (under the dura mater) localization. MRI reveals hemorrhagic disorders that are associated with axonal damage.
Danger can lurk at every step
In adults, a concussion often occurs against the background of alcohol intoxication: either he lost his balance, or he actively got involved in a fight, or he got into an accident. Alcohol in such cases becomes a factor that aggravates the patient’s condition and complicates early diagnosis,
because it obscures the clinical signs of the underlying pathology. It is difficult to figure out: lethargy and other manifestations are a consequence of intoxication or indicate the development of symptoms of a concussion. True, there are other options when an adult, completely sober person receives a TBI in transport, on the road, or at work due to circumstances beyond his control.
Head bruises often plague children and teenagers in games due to carelessness (slamming a book or briefcase on the head, other fun) or overestimation of capabilities when spending leisure time, because you really want to show off your adult prowess by riding an “iron horse” or jumping on roofs and fences.
Meanwhile, I would like to remind you that a concussion can occur without a blow. Sharp braking of a vehicle or attempts to maintain balance in winter ice sometimes also result in a known diagnosis.
Everyone knows that there are frequent cases of TBI and injury to other parts of the body among those for whom “sport is their life.” Chess does not sharpen an athletic figure and does not add physical strength, but “a person strives for perfection”, so he searches for new types of sports exercises, borrowing them from his peers overseas. What this could lead to - further.
The signs of a concussion in a child who can already speak and knows his “I” are practically no different from those in adults. But recognizing the symptoms of a concussion in infants can be very difficult even for a healthcare worker,
unless he is a pediatric neurologist, therefore, if this pathology is suspected, it is better for parents not to try to take responsibility and make a diagnosis on their own. The baby should be immediately shown to a doctor who is able to distinguish the normal behavior of the baby from the behavior of a sick child.
How to recognize a concussion in young children?
In general, a concussion in infants is a rather rare phenomenon; everything in them is so soft and elastic that the risk of getting a concussion is very small, and, as the saying goes: “A child falls, God lays down the straw.” However, there is still no need to relax too much; parents should be constantly on alert and know the main signs of a concussion in a child:
- Frequent regurgitation, refusal to eat, which, however, can be caused by other reasons (intestinal colic, weather change, ARVI).
- Increased excitability, anxiety or, conversely, lethargy and drowsiness also do not mean much.
- Twitching of the muscles of the limbs.
- Unnatural paleness or redness of the face.
You should especially pay attention to the appearance of unusual signs if the child hit his head the day before.
More often this happens to children who have learned to roll over, sit and crawl, but have not yet acquired a sense of danger. Such a fiend needs an eye and an eye, but he already has more symptoms of concussion than very small ones, for example:
- The child hit himself, was silent, and then began to cry bitterly (he may have lost consciousness for a few seconds).
- In such “big” children, it is easier to distinguish vomiting from regurgitation and notice sleep disturbances, since the time of play and wakefulness has increased.
In a word, with children who have emerged from the newborn state it is already possible to somehow “agree” and understand the cause of the anxiety.
Unfortunately, there are often cases when a visit to the doctor is postponed or even canceled, time passes and everything seems to return to normal, but the harm to health caused by a seemingly insignificant blow can be significant, and the consequences are not comforting:
- Intense headaches following a concussion many years ago can last a lifetime.
- Vegetative-vascular disorders.
- Disorder of thinking processes, poor assimilation of the school curriculum.
- Convulsive syndrome.
Clinical picture of mild traumatic brain injury
Signs of TBI are not always present all together and give a clear clinical picture. In general, the symptoms of a concussion depend on the severity of the condition and include:
- Lethargy, confusion, stupor, lack of concentration.
- Possible (but not obligatory) loss of consciousness lasting from a few seconds to hours and days. Moreover, according to Western experts, the duration of a comatose state should not exceed 6 hours, only then can one count on a favorable prognosis.
Otherwise, it becomes obvious that there was some damage to the brain tissue, and this is a different diagnosis and other consequences. - Nausea, which is often accompanied by vomiting.
- Dizziness, headaches, tinnitus, impaired coordination of movements.
- Paleness of the skin of the face, followed by hyperemia (“vasomotor play”).
- Brady or tachycardia.
- Pain in the eyes, especially when moving the eyeballs, unpleasant sensations in the temporal areas.
- Amnesia (memory loss), when a person cannot remember the events preceding the blow, the strength of which determines the duration of the period lost from memory. This symptom is not very common, and sometimes requires a long recovery.
Considering that a diagnosis such as a concussion, in itself, is the first and mildest degree of serious pathology, united under the general name “traumatic brain injury,” the modern classification does not provide for dividing this form according to severity separately. However, we can agree that not all blows and bruises occur in the same way, so there are certain varieties that make it possible to determine and convey (rather verbally) the degree of damage, which is sometimes used by doctors and quite often patients:
- A mild concussion
is avoided without loss of consciousness and amnesia; signs of trouble in the head (lethargy, nausea, severe headache) usually disappear within a quarter of an hour. - In grade 2
, loss of consciousness is usually absent, but stupor, memory loss and other symptoms occur. - A severe
concussion may be characterized by memory loss and loss of consciousness in combination with the entire set of objective clinical manifestations of pathology, since the patient can make complaints only upon returning to real life (restoration of consciousness).
The damage to health caused by TBI can be significant and depends on what kind of injury the person received: a mild concussion in an adult, with timely first aid and adequate further treatment, can pass and be forgotten. However, it only seems so. Attacks of headaches after a concussion are a common and understandable phenomenon, but the patient himself rarely connects these events with each other, believing that too much time has passed. As for a brain contusion, depending on the severity, it can leave the most serious consequences.
Treatment methods
A neurologist will tell you how to treat a mild concussion. Usually the patient is under medical supervision in the hospital for several days, then he is sent home. The patient is prescribed bed rest. In the acute period, symptomatic treatment is carried out. In most patients, regression of symptoms (head pain, dizziness) occurs without treatment within a few days. In some cases, the recovery period takes longer – several weeks.
The speed of recovery correlates with the severity of the injury, the age and general health of the patient. In young patients whose duration of loss of consciousness was no longer than a few seconds, complete recovery usually occurs within 1-2 weeks. In patients over 50 years of age, recovery processes are slow, and recovery may be incomplete. Factors influencing the recovery process:
- History of somatic diseases and mental disorders.
- Alcohol abuse.
- Rental attitudes (readiness to receive benefits associated with an unfavorable situation - insurance, disability benefits, medical care, increased attention from loved ones).
Medical observations show significant heterogeneity in clinical manifestations in patients who have suffered an episode of mild concussion. A head injury is a significant stress factor that can cause serious consequences in the future.
Drug therapy
Therapy for a minor concussion involves eliminating symptoms - headaches, sleep disturbances, irritability and anxiety. An important therapeutic direction is the restoration of brain functions. Treatment for mild concussion includes taking pharmaceutical medications:
- Analgesics (to relieve pain).
- Vestibulolytics (to eliminate vestibular disorders - dizziness, impaired motor coordination).
- Tranquilizers, antidepressants (to combat anxiety disorders and depression).
- Anticonvulsants (to eliminate seizures).
- Hypnotics (to combat sleep disorders).
The doctor will determine what medications the patient should take, due to the need for complex therapy taking into account clinical manifestations. Psychotherapy refers to auxiliary methods of treatment.
What consequences can be expected from TBI?
Why, when collecting anamnesis to establish any diagnosis that is not related to the brain, does the doctor never forget to inquire about the presence of traumatic brain injuries in the past? And all because TBI in any form and severity often has far-reaching consequences:
- Increased sensitivity to alcoholic beverages or pathogens of infectious diseases, which, in turn, can lead to mental disorders, for example, the development of psychosis due to influenza or alcohol intoxication.
- Severe vegetative-vascular disorders, manifested by surges in blood pressure, dizziness and headache, hot flashes, sweating and fatigue.
- Irritability, psycho-emotional instability, increased excitability, aggression, but quick resignation (the person understands, but cannot do anything, so he asks for forgiveness for his actions, and then commits them again).
- A convulsive syndrome that looks like epilepsy, depriving you of the right to drive a car and access to certain professions (at heights, near water, near fire, etc.).
- Depressive states, neuroses, fears and phobias, sleep disturbances.
- The most common and severe consequence of a concussion is considered to be post-concussion syndrome,
which develops after a certain period of time (days, weeks, months) after a head injury and torments a person throughout his life with constant attacks of intense headaches, dizziness, nervousness, and insomnia. Often patients lose the ability to perform even simple work and receive a disability group. However, the worst thing is that conventional analgesics, psychotherapy, physiotherapeutic procedures and sanatorium-resort treatment in this case are ineffective, and the prescription of narcotic medications threatens the formation of addiction.
The consequences of any form of TBI, even the mildest, can be very serious, so it is useful for every person to know what to do in case of a concussion and to be able to provide first aid.
Lay down, watch and wait
It is unlikely that a victim in a state of inhibition can quickly orient himself and independently assess the situation. It should be noted that the first symptoms of TBI in the case of a concussion and in the case of a brain contusion or hemorrhage may be identical, so first aid in this situation is to monitor the behavior of the patient who needs to be put down, since excessive activity can cause additional harm to health.
What to do if you have a concussion? To do this, you need to be sure that this is still a concussion, and not another, more severe, form of TBI,
therefore, at the slightest sign of a traumatic brain injury (the clinic is described above), the person should be shown to a doctor.
If the accident took place at home, the patient did not lose consciousness, the condition did not change for the worse within half an hour and is assessed as completely satisfactory, then you should consult a neurologist at your place of residence. Unfortunately, patients often let everything go “on the brakes” and don’t go anywhere, and then wonder where the causeless headaches come from? After a concussion, of course, which was not diagnosed in time. Loss of consciousness or its absence, nausea and vomiting, deterioration of a condition
that initially did not cause much concern are alarming symptoms that require immediate medical intervention. Such patients require hospitalization, but there is no need to try to transport the patient yourself unless there is an urgent need (lack of communications, remote area). Meanwhile, having decided on independent transportation, if there is no other way out, you need to keep in mind that the victim, in addition to the head, may have other organs damaged (the spine, for example), so all actions should be as gentle as possible, but quickly.
You should not offer a person medicine at your own or (even worse) his discretion if he is conscious. You just need to lay the patient down, provide first aid, call an ambulance and wait for it to arrive.
The actions of a random witness to the incident who happens to be nearby and is trying to help in some way should look like this:
- Carefully place him in a horizontal position, but if the person is unconscious, then vomiting cannot be ruled out in case of a head injury, so it is better to turn the patient onto his right side, bending his arm and leg on the left side.
- Unbutton the collar, loosen the tie, in general, remove unnecessary accessories and allow the victim to breathe freely.
- Apply cold to the bruised area, treat wounds, bandage, stop the bleeding.
- Monitor your pulse (frequency, filling, tension) and blood pressure, if possible.
- If breathing stops, begin cardiopulmonary resuscitation (artificial respiration, chest compressions).
Unfortunately, life is full of surprises, sometimes very unpleasant, and the situations in which concussions sometimes occur can be so different...
First aid for concussion
- If one or more symptoms are present, immediately call an ambulance or take the victim to a doctor.
- Treat a wound on the head if it appears as a result of an impact.
- For an hour or until the doctor arrives, it is important not to fall asleep, but to remain at rest.
- If you lose consciousness, lay the person on his side, bend his knees, and put his hands under his head.
- If symptoms of a concussion do not immediately appear, it is recommended to rest and not begin vigorous activity.
Diagnosis and treatment is the task of the hospital
As a rule, a neurologist will suspect a mild TBI, that is, a concussion, even based on 2-3 signs.
However, in order to properly treat the patient, it is necessary to establish an accurate diagnosis by conducting a series of studies:
- Craniography (survey R-graphy of the skull) to exclude skull fractures;
- Examination of the blood vessels of the fundus (consultation with an ophthalmologist);
- Lumbar (spinal) puncture to study the composition of cerebrospinal fluid;
- Magnetic resonance imaging (MRI) or computed tomography (CT);
- Electroencephalography (EEG);
- Dopplerography of the vessels of the head (ultrasound, ultrasound).
The patient is in the hospital mainly for the purpose of monitoring him, where he is given preventive and symptomatic treatment:
- Analgesics (baralgin, sedalgin, ketorol).
- Sedatives (tinctures of valerian and motherwort, tranquilizers - Relanium, phenazepam, etc.).
- For dizziness, bellaspon, bellataminal, and cinnarizine are prescribed.
- Magnesium sulfate is good for relieving general tension, and diuretics are helpful for preventing cerebral edema.
- It is advisable to use vascular drugs (Trental, Cavinton), nootropics (Nootropil, Piracetam) and B vitamins.
The victim, if everything goes well and manages only a concussion, will spend about a week in the hospital, but this does not mean that all questions are closed, and he can consider himself completely healthy. He will be observed by a neurologist for another whole year, visiting the clinic every quarter and receiving treatment prescribed by the doctor.
Thus, it is not recommended to treat a concussion on your own or take any medications.
Moreover, often patients, reacting to all external influences (people’s voices, light, etc.), become even more irritated and lose the ability to correctly assess their condition. They have a negative attitude towards hospitalization and believe that they themselves know how best to cope with an unexpected problem. This should be taken into account by relatives or people who happen to be nearby.
Brain contusion and other TBIs
At the beginning of the article, it was noted that not all TBIs are concussions, but all concussions are traumatic brain injuries. What does it mean? People often consider all injuries, including bruises, compression of the brain, and intracranial hematoma, to be a “concussion.” Traumatic brain injury is an umbrella term. With a TBI, in addition to a concussion, brain structures, cranial nerves, the pathways along which cerebrospinal fluid moves, as well as vessels that deliver nutrients and oxygen with blood can be damaged.
In addition, it should be borne in mind that not only the blow itself, when the brain is damaged at the site of application, can be dangerous for the victim, but also the counter-shock coming from the vibration of the cerebrospinal fluid
or from effects on the processes of the dura mater. Thus, not only the cerebral hemispheres may be damaged, but also the trunk, in which the centers responsible for the activities of many important organs and systems are localized, and metabolic processes will be disrupted. To help the reader correctly assess the situation and navigate such diagnoses if necessary, we will try to briefly dwell on other TBIs:
- Brain contusion,
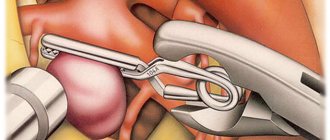
which, unlike a concussion, in addition to general cerebral symptoms, gives local and focal symptoms, depending on the location of the contusion. Brain contusion has 3 degrees of severity, victims with mild and moderate severity are sent to neurosurgical departments, and with grade 3 they are subject to hospitalization in hospitals with intensive care, resuscitation and neurosurgery departments. - Compression of the brain,
as a rule, occurs against the background of severe contusion of the brain and is usually a consequence of the formation of an intracranial hematoma. It manifests itself as psychomotor agitation, an increase in cerebral symptoms, and the development of convulsive syndrome. - An intracranial hematoma
requires urgent surgical intervention in the neurosurgery department. It can manifest itself some time after the injury, which is why seemingly well-being after a TBI does not actually give grounds for peace of mind. It is this symptom, called the light gap, that is considered an important and insidious sign of a hematoma, and its underestimation is fraught with the development of life-threatening consequences for the victim.
Of course, the therapeutic approach to conditions of this kind is markedly different from the treatment of concussion:
The victim requires not only emergency hospitalization, but also the immediate start of all measures, including surgery, if an intracranial hematoma is diagnosed, which can “deceive” both those around him and the doctor of the arriving ambulance team.
often misleading.
(the person came to his senses and claims that he feels normal). The thing is that post-traumatic intracranial hematoma can occur at the initial stage without much suffering to the brain, especially if the source of bleeding is venous (when bleeding from an arterial vessel, the light interval lasts minutes). An intense increase in symptoms of respiratory and vascular disorders, the development of mental disorders, and a decrease in heart rate against the background of increased blood pressure increase suspicions of an intracranial hematoma, so the patient should under no circumstances be left without hospitalization.
typical areas of hemorrhage and hematoma formation due to head injuries or hemorrhagic strokes
Traumatic brain injury is a common occurrence in our lives, because there are so many dangers around. Often it is limited to a mild degree - a concussion, which, however, does not allow you to relax. You should always keep in mind the possibility of hidden damage and the development of serious complications. Ignorance and underestimation of the insidiousness of TBI can become a tragic mistake that interrupts someone’s life, therefore, in all cases of head injuries, the patient should not be left without attention and help, even if he confidently claims that everything is fine.
Recommendations for the treatment of concussions
If hospitalization is not required, with the permission of a doctor, a mild concussion can be treated at home:
- Bed rest and rest are required, no work. Long sleep is very important.
- You cannot read, watch TV, play computer games or use gadgets.
- Under no circumstances should you play sports.
- You are allowed to listen to music, but not through headphones.
- You can use herbal sedative drops or herbal infusions.
- In your diet, you should give preference to dairy and plant products, limit salt intake - to prevent increased pressure, including intracranial pressure.
If the patient seeks medical help in a timely manner and all recommendations are followed, recovery will occur quickly and without complications.