Anemia
or
“anemia”
- a decrease in the concentration of hemoglobin in the blood below established standards, most often, with a simultaneous decrease in the total volume of red blood cells (red blood cells that carry oxygen). Anemia, as a secondary symptom, can accompany various diseases, causing the development of oxygen starvation of tissues. The patient experiences chronic fatigue and weakness, constant drowsiness and loss of strength, dizziness and shortness of breath.
Anemia in men and women
Anemia is one of the most common diseases among the adult population of the Earth today. Risk groups for developing anemia include:
- lovers of vegetarian cuisine.
- patients suffering from large blood losses due to the physiological characteristics of the body or a number of chronic diseases.
- pregnant women.
- professional athletes.
Anemia in men is diagnosed in the presence of malignant neoplasms or hidden bleeding of the gastrointestinal tract, peptic ulcer, hemorrhoids and other pathologies. A decrease in the level of hemoglobin in a woman’s blood can be associated with heavy menstruation, pregnancy and lactation, and a period of hormonal changes during menopause. Varying degrees of anemia also appear in children due to lack of adequate nutrition, impaired absorption of iron in the gastrointestinal tract, gastritis or parasitic diseases, limited exposure to fresh air and physical inactivity.
Detailed description of the study
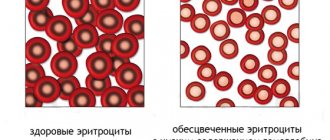
Anemias are conditions that occur when the number of red blood cells - red blood cells - and the concentration of hemoglobin in a person's blood are significantly reduced.
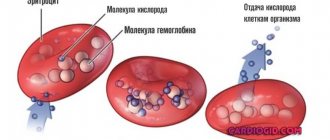
Hemoglobin is a complex iron-containing protein found in red blood cells and is essential for transporting oxygen from the lungs to the tissues.
The main causes of anemia include:
- Impaired or decreased production of red blood cells, which may be associated with deficiency of iron or B vitamins, the presence of certain cancers, inhibition of the hematopoietic function of the bone marrow;
- Significant loss of red blood cells after massive bleeding (posthemorrhagic anemia);
- Increased breakdown (hemolysis) of red blood cells (hemolytic anemia).
Anemia can be acute or chronic. Chronic anemia, as a rule, accompanies other diseases (diabetes mellitus, cancer, chronic renal failure) and in most cases is asymptomatic or with minimal clinical manifestations.
The main clinical symptoms of anemia:
- Increased fatigue;
- Dyspnea;
- Dizziness;
- Tachycardia - rapid heartbeat;
- Pale skin.
Anemia is a fairly common condition diagnosed in both men and women. However, some factors increase the risk of developing pathology:
- Diet low in iron source foods (vegetarianism);
- Acute and chronic kidney diseases;
- Some autoimmune diseases (diabetes mellitus);
- Oncological diseases;
- Inflammatory bowel diseases;
- Genetic predisposition;
- Chronic infectious diseases (tuberculosis);
- Conditions after injuries and surgical interventions;
- Chronic bleeding.
To diagnose anemia, a number of laboratory parameters are determined. This comprehensive laboratory test includes all the necessary tests to diagnose anemia and determine the causes of its development.
General blood test extended with leukocyte formula and reticulocytes.
The analysis allows you to determine the concentration of hemoglobin, estimate the number of blood cells, as well as a number of other important indicators (color index, normoblasts).
This test evaluates three types of blood cells:
- Red blood cells (erythrocytes and reticulocytes) Erythrocytes are the most numerous group of all the formed elements of blood. They contain iron-containing protein - hemoglobin and together with it transport oxygen throughout the body. A decrease in hemoglobin concentration is the main indicator of anemia. Reticulocytes are immature red blood cells. The number of reticulocytes reflects their production by the bone marrow. The study of this parameter allows us to assess the hematopoietic function of the bone marrow.
- White blood cells (leukocytes) Leukocytes are cells that are constantly present in the blood, lymphatic system and tissues, and are an important part of the body's natural defense (immune) system. They provide protection against infections and also participate in the formation of inflammation and allergies. The number of leukocytes in the blood is relatively stable. A change in the number of leukocytes occurs in response to a change in the state of the body (infectious disease, inflammation, etc.).
- Platelets Platelets are blood cells that circulate in the blood and are necessary for its normal clotting. When a vessel wall is damaged, platelets help stop bleeding by adhering to the site of injury and forming a temporary plug. Diseases or conditions that are associated with low platelet levels (thrombocytopenia) or decreased platelet function increase the risk of developing anemia.
Also, with anemia, normoblasts, the precursors of reticulocytes, can be found in the blood. Normally, these cells can only be found in the bone marrow; their appearance in the bloodstream is a sign of pathology.
- ESR according to Westergren (venous blood) Erythrocyte sedimentation rate (ESR) is an indicator that depends on the ratio of protein fractions in the blood and the number of red blood cells. A change in ESR may indicate the presence of an inflammatory, autoimmune or oncological disease, which may cause the development of anemia. An increase in ESR is normally observed in any acute or chronic inflammatory process.
- Transferrin, ferritin and THC These indicators reflect the metabolism of iron in the body. This trace element is mainly included in the hemoglobin of red blood cells and is necessary for their normal production by the bone marrow. A person gets iron from foods (liver, red meat, spinach, legumes). When iron is absorbed in the intestine, it is transported by transferrin. Determining the level of transferrin reflects the total “reserves” of iron in the body. TIBC (total iron-binding capacity of serum) is an indicator that reflects the amount of iron that can be bound by transferrin. In healthy people, part of the iron entering the body is contained in hemoglobin. The other part is stored in tissues in combination with ferritin or hemosiderin. Ferritin is a protein complex that acts as the main “storage” of iron in the body. A small portion of ferritin is present in the blood; by measuring this indicator, iron reserves can also be assessed. These studies allow us to indirectly assess the amount of iron in the body in order to diagnose its deficiency and determine the cause of anemia.
- Folates and vitamin B12 Vitamin B12 and folic acid (vitamin B9) are representatives of the B vitamins, which are necessary for the body to produce red blood cells, white blood cells, and the synthesis of nucleic acids. Vitamin B12 also ensures the functional activity of cells in the central nervous system. Folates are salts of folic acid, a natural form of vitamin B9.
Vitamin B12 and/or folic acid deficiency reflects a chronic lack of one or both of these vitamins. Long-term deficiency of vitamin B12 or folic acid can lead to macrocytic anemia. In this case, the production of red blood cells by the bone marrow decreases, while they increase in size, and their ability to transport oxygen is significantly reduced, which causes hypoxia (oxygen deficiency in tissues).
Characteristic clinical signs of B12 deficiency anemia include:
- Constantly increasing weakness, apathy;
- Rapid heartbeat, heart pain;
- Weakness in the legs, “numbness” of the limbs;
- Swelling and pale complexion.
The most common cause of vitamin B12 deficiency is impaired absorption in the intestine. This may be due to chronic inflammatory diseases of the intestinal mucosa (atrophic gastritis), surgical removal of part of the organ, or some hereditary absorption pathologies.
Most anemia is a complication of other diseases, so in order to choose the right treatment tactics, it is necessary to find out the cause of the anemia. The studies included in this complex make it possible to assess the qualitative and quantitative composition of cells and biochemical parameters of the blood system, as well as to identify disturbances in its functioning. Based on the test results, it is possible to carry out a primary diagnosis of anemia, as well as a differential diagnosis of the types of disease.
A detailed description of the studies and reference values are presented on the pages with descriptions of individual studies.
Principles of classification of anemia
There are several types of classifications of anemia, based on a number of signs - the cause of the disease, the mechanism of its development, stages, symptoms and other parameters. The following groups are distinguished:
Sign up for an anemia screening
Make an appointment
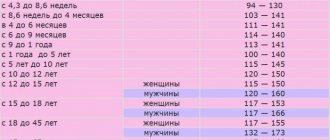
Classification of anemia by severity
The severity of anemia, determined by blood parameters depending on the age and gender of the patient, is conventionally divided into mild, moderate and severe. The mild form is characterized by a decrease in hemoglobin concentration to 90 g/l (the patient may experience general weakness and increased fatigue). The average degree is determined by the range from 70 to 90 g/l (patients complain of shortness of breath, tachycardia, headache, sleep disturbance, tinnitus, loss of appetite), and severe - below the limit of 70 g/l (the main danger of this condition is the development heart failure).
Acute posthemorrhagic anemia
Signs
The signs and severity of acute posthemorrhagic anemia depend on the volume of blood lost.
First of all, signs of collapse appear: pallor of the skin and mucous membranes, palpitations, dizziness, fainting, shortness of breath, nausea, drop in arterial and venous pressure, pointed facial features, cold sweat, cold and pale hands and feet, blue discoloration under the nails. The pulse is weak, frequent (thread-like in case of large blood losses). Vomiting may occur (with stomach bleeding - with scarlet blood or the color of coffee grounds). The condition of patients worsens in an upright position. When moving to horizontal, dizziness intensifies, vision becomes dark, and loss of consciousness is possible. An important sign of internal bleeding is sudden dryness in the mouth. But the severity of these symptoms cannot be used to judge the degree of blood loss, since they are often signs of injury that caused blood loss. In addition to signs of collapse, those associated with the underlying disease resulting from anemia may also appear. For example, acute abdominal pain is observed with intussusception (the insertion of one part of the intestine into the lumen of another). And if the pain is accompanied by hemorrhagic (in the form of red dots or spots of various sizes and shapes) rashes on the skin of the lower extremities and pain in the joints, then this is the result of hemorrhagic vasculitis (Henoch-Schönlein disease). Epigastric pain occurs during exacerbations or perforation of gastric or duodenal ulcers. Pain in the lower abdomen with signs of acute blood loss can signal an ectopic pregnancy, ruptured ovarian cysts, or renal colic. Lower back pain is due to hemorrhages in the perinephric tissue. Retrosternal and interscapular pain - about dissecting aortic aneurysm and myocardial infarction; acute short-term pain in the chest with severe shortness of breath - hemothorax or pneumothorax.
Description
Acute blood loss can occur due to injury, surgery, internal bleeding (stomach, duodenum), ectopic pregnancy and other gynecological pathologies, lung diseases, from dilated veins of the esophagus, etc.
It can be triggered by destructive tumors, as well as vascular lesions (hereditary or acquired) such as angiomas, arteriovenous aneurysms and other vascular dysplasias, bacterial and immune vasculitis.
The cause may be hemorrhages (leakage of blood from the vessels) of the female genital organs and bleeding of various locations associated with hemorrhagic diathesis - for example, thrombocytopenia, hemophilia, etc.), as well as long-term use of anticoagulants.
First aid
It is necessary to call an ambulance as quickly as possible, and before it arrives, take measures to stop the bleeding: applying a tourniquet or pressure bandages, pressing the bleeding vessels, nasal tamponade, etc. These are mechanical methods. There are also chemical drugs that locally stop bleeding: hemostatic sponge or fibrin film (with or without thrombin), bioglue, 5% aminocaproic acid (it is used to irrigate the bleeding site), 0.025% adroxon solution (up to 5 ml).
Diagnostics
When making a diagnosis, information about the acute loss of a large amount of blood due to external bleeding is taken into account. If the bleeding is significant, the diagnosis is based on clinical signs in combination with laboratory tests (Gregersen, Weber), an increase in the level of residual nitrogen in bleeding from the upper gastrointestinal tract.
In the first hours of acute posthemorrhagic anemia, the severity of blood loss can be judged by a decrease in the volume of circulating blood, which can be determined (rather approximately) by the shock index, which shows the ratio of the pulse rate to the level of systolic blood pressure. With significant blood losses, this index exceeds one, and with large ones - 1.5.
Treatment
In case of acute posthemorrhagic anemia, the patient is sent to the hospital, and only in a lying position in an insulated transport, preferably in a specialized car that can provide infusion therapy during transportation.
In the hospital, the bleeding is finally stopped. If surgical intervention is necessary, intensive infusion and transfusion therapy is first performed. After stopping bleeding and stabilizing the patient's condition, treatment for iron deficiency anemia with iron preparations is started. For severe anemia - intravenously, for milder anemia - orally. Sometimes intravenous or intramuscular administration of iron preparations is combined in the first 3-4 days, followed by oral administration. Transfusion of freshly prepared canned blood or red blood cells is resorted to only in case of severe anemia and only until the hemoglobin content in the blood increases above 60-70 g/l. For posthemorrhagic anemia, vitamin B12, folic acid and other hematopoietic stimulants, which are used for other types of anemia, are contraindicated.
Prevention
Treatment of the underlying disease and prevention of bleeding. If this fails, timely detection of the source of blood loss is important.
© Dr. Peter
Classification of anemia by color index
The color index determines the level of saturation of red blood cells with hemoglobin. It is calculated during a laboratory blood test using a special formula. Depending on the results obtained, there are:
Introduction
Anemia is a clinical and hematological syndrome that is characterized by a decrease in the number of red blood cells, hemoglobin and/or hematocrit relative to the normal reference range.
In accordance with the recommendations of the World Health Organization, a hemoglobin level of 130–160 g/l is considered normal for men, and 12–150 g/l for women [1–3]. Anemia develops in a variety of diseases and conditions, both physiological (periods of rapid growth, pregnancy, lactation, etc.) and pathological. With pathology of the digestive organs, anemia is not uncommon. It is impossible to use information about its true prevalence in real practice, since official statistics take into account only the underlying disease, and anemia, as a rule, acts as a complication or concomitant pathology [1, 3].
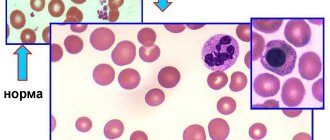
In practice, a doctor of any specialty needs to not only assess the level of red blood cells and hemoglobin, but also analyze red blood cell indices, which will help build a primary diagnostic concept.
MCH is the average hemoglobin content in a red blood cell, normally 27–31 pg. This indicator corresponds to the previously determined color indicator. Increased MCH indicates hyperchromic anemia, decreased MCH indicates hypochromic anemia.
MCV is the average volume of an erythrocyte, normally 8–100 fl. According to its values, anemia is divided into macro-, micro- and normocytic.
RDW is the red blood cell distribution width, an indicator that indicates how much red blood cells vary in size. If both large and small red blood cells are present in the blood, the width of the distribution will be higher than normal and this condition is called anisocytosis - this is a sign of anemia.
For a practicing physician, the classification of anemia by erythrocyte volume is of great importance, according to which macrocytic (in most cases this is B12-folate deficiency anemia), microcytic (most often iron deficiency) and normocytic anemia are distinguished. Thus, based on the MCV indicator, it is possible to suggest the most likely cause of anemia, build a differential diagnostic search, and prescribe appropriate therapy [1–4].
In diseases of the digestive system, the causes and type of anemia are diverse [4, 5]. Posthemorrhagic anemia occurs against the background of bleeding of varying intensity from varicose veins of the esophagus and/or rectum with cirrhosis of the liver, from ulcerative defects of various parts of the digestive tube. It can develop over a fairly short period of time or form gradually, as with enteropathy caused by taking non-steroidal anti-inflammatory drugs, or with malabsorption syndrome. Deficiency anemias are formed during atrophic processes in the upper parts of the gastrointestinal tract (GIT), such as chronic atrophic gastritis and duodenitis, during resection of the stomach, duodenum and initial parts of the small intestine, and less often with inflammatory bowel diseases. Hemolytic anemia often serves as a companion to the pathology of the hepatobiliary zone. Anemia of chronic diseases develops with inflammatory bowel diseases, liver and a number of others [2, 4, 5].
As has been repeatedly emphasized, anemia is most often associated with other diseases. It can be a symptom of oncological pathology [4, 5], which is revealed precisely during the diagnostic search. As an example, we give one of our own observations.
Clinical case 1
Patient B. 53 years old. Body weight – 132 kg. Suffers from gastroesophageal reflux disease, cholelithiasis, and coronary heart disease. Since July 2021, in order to lose weight, I have sharply changed my diet, incl. completely abandoned animal food. Over the course of 4 months, I lost 16 kg, began to notice weakness, decreased tolerance to physical activity, and increased shortness of breath.
A progressive decrease in hemoglobin was noted in the blood to 111, and then to 85 g/l. Against this background, a paroxysm of atrial fibrillation developed, for which he was hospitalized.
During an examination to clarify the cause of anemia, a colon tumor was identified (Fig. 1).
Anemia reduces the quality of life, worsens the course of other existing diseases, aggravates the prognosis during planned (and even more so emergency!) surgical interventions, etc. [3, 6–8].
Clinical manifestations of anemia, such as sideropenic, hypoxic syndromes and metabolic intoxication syndrome, are quite fully described in the literature [1, 2, 4–6]. Moreover, the symptoms of anemia with the same hemoglobin levels are more pronounced in men than in women. The same can be said about age: symptomatic anemia is more common in the elderly than in young people.
L. Balducci and C. Beghe (2005) emphasize that the hemoglobin level in an elderly person should not be allowed to fall below 100 g/l, because this can lead to a loss of functional independence for the patient and the need for care.
The nature of nutrition plays an important role in the formation of anemia. It is known that there are a number of foods richer in iron. It is necessary to remember that iron is contained in food in two forms: non-heme - in vegetables, fruits, cereals, the percentage of its digestibility ranges from 1 to 7, and heme - in meat, which is absorbed by 17-22. And vegetarianism, which has recently gained popularity, is not always justified. As an example, we give our own observation.
Clinical case 2
Patient T., 70 years old. Since his youth he has suffered from gastritis, periodically he is bothered by heaviness in the epigastrium after errors in diet, and belching air. For this reason, he was not examined or treated. She is being seen by a cardiologist for coronary heart disease and hyperlipidemia. All my life I worked at a meat processing plant and ate mostly fatty meat foods. Over the past 2 years, I decided to completely give up animal products in order to “unload the body and normalize cholesterol” and independently stopped taking statins.
According to the outpatient card, initially hemoglobin was 142 g/l. Heart rate (HR) while taking β-blockers remained within the target value of 60 beats per minute. Over the next 2 years, on a strict vegetarian diet, hemoglobin decreased to 90 g/l. The level of ferritin, a marker of depletion of iron stores in the depot [2, 4], was only 5 μg/ml, and other indicators of iron metabolism were also significantly reduced. At the same time, the heart rate increased to 80 beats/min, which is a negative factor for a cardiac patient. During that period, extrasystole and paroxysms of atrial fibrillation were recorded several times, and exercise tolerance decreased. It is worth noting that the patient’s cholesterol level did not decrease (Fig. 2).
Discussion
The main method of treating anemia is replacement therapy. However, blood transfusions should be used only for strict indications.
According to the order of the Ministry of Health of the Russian Federation “Rules for the clinical use of donor blood and its components,” No. 183n dated 14/02/2013 and its earlier version No. 363 dated November 26, 2002, the indications for blood transfusion are [9, 10]:
- acute anemia due to massive blood loss when the hemoglobin concentration decreases to less than 70–80 g/l, hematocrit to 25% and the occurrence of circulatory disorders;
- chronic anemia - only (!) for the correction of the most important symptoms caused by anemia and not amenable to basic pathogenetic therapy.
Pathogenetic therapy includes the use of iron supplements. There are quite a large number of them in both tablet and parenteral form.
The route of administration of the iron preparation is determined by the specific clinical situation. The state of the gastrointestinal tract, which limits the absorption of ingested iron, must be taken into account. Iron should not be prescribed orally for acute pathology of the upper gastrointestinal tract. In inflammatory bowel disease and malabsorption syndrome, the effectiveness of the oral delivery route is also very questionable [2, 5]. Parenteral drugs do not serve as a first-line treatment, but in some situations it is necessary to start with them.
In the order of the Ministry of Health of the Russian Federation “Rules for the clinical use of donor blood and its components”, No. 183n dated 02.14.2013 and its earlier version No. 363 dated 25.11.2002, it is noted that anemia in inflammatory bowel diseases, with malabsorption syndrome (gastrectomy, impaired iron absorption in the intestines) anemia associated with a tumor, incl. and with a gastrointestinal tumor, serves as an indication for parenteral administration of iron preparations [9, 10].
Of the parenteral iron preparations currently existing on the domestic pharmaceutical market, iron carboxymaltose is becoming increasingly popular. This high-molecular complex provides a slow and physiological release of iron and has the least immunogenic potential [6–8]. According to some studies, iron carboxypolymaltose was more effective compared to other intravenous drugs [6, 11]. This can be a decisive argument in favor of this drug, especially in situations where it is necessary to normalize hemoglobin levels as quickly as possible and replenish iron reserves in the depot. In addition, the ease of administration of the drug is attractive, which allows it to be used not only in a 24-hour hospital, but also in day care hospitals and on an outpatient basis - in the treatment room of a clinic.
In accordance with the instructions, a test dose is not required; up to 1000 mcg of iron can be administered at a time. The calculated course dose of iron can be administered intravenously drip into 100–250 ml of physiological solution quickly (from 15 minutes per infusion!) or intravenously as a stream. 1000 mg of iron is given intravenously once a week once a week or in two doses if the patient needs a larger dose. No more than 4 ml (200 mg) per day is administered as a bolus and no more than 3 times a week [12]. Once the iron deficiency has been corrected (calculated using the formula for each patient), further oral administration is not required. This significantly increases adherence to this treatment.
Subsequently, if the source of blood loss has been eliminated, then additional infusions of iron carboxymaltose are usually not required. If the source of blood loss cannot be eliminated, it is necessary to monitor indicators of iron metabolism, primarily ferritin, MCH, MCV, RDW. At initial signs of iron deficiency, the administration of iron carboxymaltose is repeated (usually once every 3–4 months).
The most important criterion for effectiveness is an increase in hemoglobin levels of >10 g/l over 4 weeks [2]. An increase in ferritin levels >100 mcg/L with regular monitoring of oral iron therapy indicates adequate iron stores in the body. In the case of parenteral administration of iron supplements, serum ferritin levels are assessed 4–6 weeks after the last intravenous dose of iron supplementation.
Let's return to clinical case 2.
During the examination, patient T. was diagnosed with chronic gastritis, duodenitis with elements of atrophy, confirmed morphologically. No pathology was found in other organs of the gastrointestinal tract. Ferric carboxymaltose therapy was proposed, which the patient refused. He began eating animal products and took ferrous sulfate orally on his own for two months. During this time, I began to feel subjectively better; my hemoglobin increased by 9 g/l. Taking into account the low level of ferritin, the presence of atrophic changes in the stomach and duodenum, and insufficient response to oral iron therapy, the question of administering iron carboxymaltose was again raised. The calculated course dose was 1500 mg. Two infusions were given: 1000 mg in the first week and 500 mg in the second. During the therapy, clinical and laboratory remission was achieved (Fig. 3).
Conclusion
Thus, anemia in gastrointestinal pathology occurs quite often and is heterogeneous in nature. Its timely recognition and correction can improve the patient’s quality of life. Iron deficiency anemia necessarily requires not only replenishment of functional iron in erythrocytes, but also replenishment of the depot, the marker of which is ferritin. Iron carboxymaltose allows you to quickly solve these problems and is easy to use, incl. in a day hospital and treatment room. The absence of the need to take iron supplements orally after its administration increases adherence to therapy.
Classification of anemia according to the mechanism of development of the pathological process
The following states are distinguished:
Iron-deficiency anemia
– the name indicates the cause of the pathology. Due to a deficiency of an important microelement, hemoglobin synthesis in the body is disrupted. The supply of oxygen to tissue cells, the stability of redox processes, and the functioning of the immune, nervous and cardiovascular systems depend on the level of iron. Clinical manifestations of iron deficiency anemia are dizziness, fainting, weakness and lethargy, shortness of breath with any exertion, palpitations. Pallor of the skin, brittle nails, thinning hair, and cracks in the corners of the lips are also typical for this disease.
Hemolytic anemia
occurs as a result of the accelerated destruction of erythrocytes (red blood cells) and the rapid accumulation of their breakdown products in the body. The main manifestations are an increased amount of indirect bilirubin in the blood. The patient experiences the development of anemic and icteric syndromes with an enlarged spleen and liver, as well as characteristic staining of feces and urine.
Posthemorrhagic anemia
– hematological changes that appear after acute or prolonged chronic blood loss as a result of external or internal bleeding (trauma, heavy menstruation, hemorrhagic diseases, gastrointestinal and pulmonary bleeding). The main manifestations of posthemorrhagic anemia are palpitations, shortness of breath, severe dizziness, darkening of the eyes, and lethargy. In severe cases - loss of consciousness.
Sideroblastic (sideroachrestic) anemia
occurs as a result of a violation of iron synthesis, causing its deficiency in red blood cells. Due to a failure in the processes of getting this microelement into the hemoglobin molecule, iron in the cells is replaced by sideroblasts (red blood cell precursor cells interspersed with iron in the form of a ring). This condition can be congenital or acquired. Experts believe that the main reason for the development of such anemia is a lack of the substance protoporphyrin. This organic component, combining with iron, turns into heme - part of the hemoglobin molecule. The main symptoms of the disease are disturbances in the functioning of the heart and blood vessels, indigestion, pale skin, dizziness, and memory loss. There is a danger of iron accumulation in various organs, which contributes to the occurrence of serious complications (liver cirrhosis, diabetes mellitus).
B12 deficiency anemia
– a disorder of hematopoiesis as a result of a lack of vitamin B12 in the human body. The main reasons for the development of such anemia are lack of adequate nutrition, impaired absorption of B12 due to inflammatory processes in the gastrointestinal tract, alcoholism, and hereditary predisposition. The pathology develops gradually, causing damage to the digestive organs and disturbances in the functioning of the nervous system.
Publications in the media
Anemia is a decrease in the Hb content per unit volume of blood, often with a simultaneous decrease in the number of red blood cells (or the total volume of red blood cells). The term “anemia” without detail does not define a specific disease, but indicates changes in blood tests, i.e. anemia should be considered one of the symptoms of pathological conditions. Frequency. 157 per 100,000 population in 2001
General signs • Hb content <100 g/l, erythrocyte count <4.0´1012/l, serum iron content <14.3 µmol/l • The isolated existence of one symptom or their combination is possible. For example, thalassemia is not characterized by a decrease in the number of red blood cells.
Classification criteria • Based on the morphology of erythrocytes, microcytic, normocytic and macrocytic anemias are distinguished (-cytic indicates the size of erythrocytes). An objective evaluation criterion is the average erythrocyte volume (MEV); normal is 80–94 femtoliters (fl) • Based on the degree of saturation of erythrocytes Hb (or serum iron content), hypochromic, normochromic and hyperchromic anemias are distinguished (-chromic indicates the color of erythrocytes). An objective assessment criterion is the average Hb content in the erythrocyte (ASGE); Normal is 27–33 picogram (pg).
Based on the combination of the first and second criteria, anemia is distinguished: •• Hypochromic microcytic (low SER and SSGE) •• Macrocytic (increased SER) •• Normochromic normocytic (SER and SSGE within normal limits) • Based on the degree of erythrocyte regeneration, anemia is distinguished between hyporegenerative (regenerative) and hyperregenerative. Determined by the number of blood reticulocytes or reticulocyte index • By the degree of hematopoietic effect of erythropoietin. Both the content of erythropoietin and the sensitivity of immature erythroid cells to it are taken into account.
Pathogenetic classification • Anemia due to impaired Hb synthesis and iron metabolism (hypochromic microcytic) •• Iron deficiency anemia (IDA) •• Thalassemia •• Sideroblastic anemia •• Anemia in chronic diseases (60% normochromic normocytic) • Anemia due to impaired DNA synthesis (hyperchromic macrocytic with megaloblastic type of hematopoiesis) •• Pernicious anemia and other B12-deficiency anemias •• Folate deficiency anemia • Other pathogenetic mechanisms (usually normochromic normocytic anemia) •• Anemia combined with a decrease in the bone marrow response to erythropoietin ••• Aplastic anemia • •• Disorders characterized by cellular infiltration of the bone marrow (myelophthisic anemia) ••• Anemia due to erythropoietin deficiency •• Hyperregenerative anemia ••• Acute posthemorrhagic anemia ••• Hemolytic anemia.
Abbreviations • SSGE - average Hb content in erythrocytes • SEV - average erythrocyte volume.
ICD-10 • D50–D53 Nutrition-related anemias • D55–D59 Hemolytic anemias • D60–D64 Aplastic and other anemias
APPLICATIONS
Congenital dyserythropoietic anemia • Type I (*224120, 15q, CDAN1, r gene). Clinical picture: moderate developmental delay, macrocytic dyserythropoietic anemia, mild hemochromatosis, bone marrow Gaucher cell-like macrophages. Laboratory tests: N-acetylglucosaminyl transferase II deficiency • Type II (*224100, 20q, CDAN2 gene, HEMPAS, r). Clinical picture: dyserythropoietic anemia, multinucleated erythroblasts, lysis of red blood cells upon serum acidification, bone marrow Gaucher cell-like macrophages. Laboratory tests: N-acetylglucosaminyl transferase II deficiency (EC 2.4.1.138) • Type III (*105600, 15q21, CDAN3, Â, r gene). Clinical picture: congenital dyserythropoietic anemia, macrocytosis, giant multinucleated bone marrow erythroblasts, jaundice; increased risk of myeloma or monoclonal gammopathy. Laboratory findings: hemosiderinuria, abnormal nuclei and intracytoplasmic inclusions in erythroblasts, highly polyploid giant mononuclear erythroblasts, elevated serum thymidine kinase levels. ICD-10 • D64.4 Congenital dyserythropoietic anemia
Megaloblastic thiamine-sensitive anemia (*249270, 1q23.2–q23.3, TRMA gene, r) is combined with diabetes and sensorineural hearing loss. Clinical picture: megaloblastic anemia, sensitive only to thiamine, ring-shaped sideroblasts, diabetes, sensorineural hearing loss, dysphonia, progressive optic atrophy, transposition of internal organs, generalized edema, congenital septal heart defects. Laboratory tests: aminoaciduria, a-ketoglutarate dehydrogenase deficiency, iron accumulation in erythroblast mitochondria. ICD-10. D53.1 Other megaloblastic anemias, not elsewhere classified
Anemia myelophthisis is a normochromic normocytic anemia that occurs when normal bone marrow is replaced by pathological tissue. Etiology • Lymphoma • Leukemia • Multiple myeloma • Tuberculosis • Granulomatosis • Metastasis of a malignant tumor to the bone marrow. Diagnostics. The appearance of immature leukocytes and nucleated red blood cells in the peripheral blood in a disproportionately large number relative to the severity of anemia, metastatic cells (solid tumor metastases). Bone marrow puncture and trephine biopsy confirm the diagnosis. Treatment is etiotropic and symptomatic. Synonyms • Myelopathic anemia • Leukoerythroblastosis. ICD-10 • D61.9 Aplastic anemia, unspecified
Anemia due to erythropoietin deficiency is normochromic (sometimes hypochromic) normocytic hyporegenerative anemia. Erythropoietin deficiency occurs in chronic renal failure when the level of end products of nitrogen metabolism in the blood increases and creatinine clearance is less than 45 ml/min. The severity of anemia usually depends on the severity of renal failure (it is most severe with primary damage to the glomerular apparatus). Etiology and pathogenesis • The synthesis of erythropoietin is suppressed by a high content of uremic toxins (in anemia as a result of chronic diseases, this effect is mediated by cytokines), which leads to the suppression of erythropoiesis • The sensitivity of the bone marrow to erythropoietin is reduced • The lifespan of erythrocytes is shortened (minor hemolysis) • Nutritional deficiency of folic acid is possible acid or iron • Uremic hemorrhagic diathesis; possible hemorrhages in the pleura, pericardium, brain •• When the endothelium of the renal vessels is damaged (malignant arterial hypertension, periarteritis nodosa, acute ischemia), microangiopathic hemolytic anemia occurs with fragmentation of erythrocytes and thrombocytopenia (in children it occurs acutely in the form of hemolytic-uremic syndrome). Treatment is etiotropic and pathogenetic • Recombinant erythropoietin is the drug of choice. Initial dose: 50–100 units/kg IV or SC 3 times a week. After 2–3 months of treatment, the erythrocyte count increases in most patients. It is necessary to monitor the concentrations of iron and folic acid in the blood, because their deficiency can lead to secondary complications • Blood transfusions (use with caution). ICD-10. B63.8 Anemia in chronic diseases classified elsewhere (specify the cause of chronic renal failure)
Microangiopathic hemolytic anemia is a secondary or congenital anemia that develops due to narrowing or obstruction of small blood vessels, which leads to mechanical damage to red blood cells during their interaction with the vascular endothelium. Etiology • Arterial hypertension • Chronic kidney disease • Prosthetic heart valves • Hemolytic-uremic syndrome • Disseminated intravascular coagulation (DIC) • Congenital microangiopathic hemolytic anemia (276850, r): polymorphic symptoms, possible involvement of the central nervous system; occurs due to fibrin deposition or the formation of platelet thrombi in the arterioles and capillaries of most organs; Characterized by thrombocytopenia, episodes of fever and petechial rash, glomerulopathy, megakaryocytosis (bone marrow). The clinical picture is determined by the underlying disease. The diagnosis is confirmed by identifying fragmented red blood cells in a peripheral blood smear in the form of schizocytes, spur cells and other abnormal forms of red blood cells. Treatment is etiotropic and restorative. ICD-10 • D59.4 Other non-autoimmune hemolytic anemias
Acute posthemorrhagic anemia is a normochromic normocytic hyperregenerative anemia that occurs as a result of acute blood loss over a short period of time. The minimum blood loss that poses a danger to the health of an adult is 500 ml. The severity of the clinical picture is determined by the amount of blood lost, the speed and source of bleeding. Etiology • Trauma • Surgical interventions • Ectopic pregnancy • Impaired hemostasis • Various diseases of internal organs accompanied by acute bleeding (for example, peptic ulcer of the stomach and duodenum). Clinical picture • General signs of anemia (tachycardia, shortness of breath, drop in blood pressure and venous pressure, pallor of the skin and mucous membranes). The severity of these changes does not correspond to the severity of anemia, because they often appear in response to a cause of bleeding (such as pain or injury) • Sudden dry mouth is an important sign of acute bleeding. Treatment is aimed at restoring blood volume • Surgical stop of bleeding • Blood transfusions. ICD-10 • D62 Acute posthemorrhagic anemia
Anemia in chronic, infectious and oncological diseases (as a rule, normochromic normocytic hyporegenerative anemia, in 40% of cases - hypochromic microcytic anemia) ranks second in frequency after IDA. Etiology and pathogenesis • Shortening of the period of circulation of mature forms of erythrocytes in the blood • Impaired utilization of iron (its release from the depot is impaired) • Relative deficiency of erythropoietin (the effect is mediated by the suppression of its production by cytokines - b- and g-IFN) • Altered bone marrow response to erythropoietin. The clinical picture is determined by the underlying disease (for example, rheumatoid arthritis, tuberculosis, cancer). Diagnosis • Moderate anemia (Hb concentration 80–100 g/l) • Serum ferritin concentration is normal or slightly increased (unlike IDA) • Fe2+ content in the blood serum is reduced, but TIVR is also reduced (unlike IDA) • Amount reticulocytes are reduced (hyporegenerative anemia). Treatment is etiotropic. ICD-10 • D63* Anemia in chronic diseases classified elsewhere •• D63.0* Anemia in neoplasms (C00-D48+) •• D63.8* Anemia in other chronic diseases classified elsewhere
Reticulocyte index. Calculation method: 0.5´(reticulocyte content´Ht of the patient/normal Ht). The content of reticulocytes is expressed as a percentage of the number of red blood cells; 0.5 — correction factor taking into account the severity of anemia; instead of Ht, you can use the volume of cell mass (BCV).
Cost of consultation for anemia?
| Name of service | Price, rub.) |
| Initial appointment with a cardiologist | 2000 rub. |
| Repeated appointment with a cardiologist | 1500 rub. |
| Primary appointment with a general practitioner | 2000 rub. |
| Repeated appointment with a general practitioner | 1500 rub. |
| Prescription of treatment (drawing up an individual treatment regimen) | 1500 - 3000 rub. |
All our services and prices
Diagnostic measures
To treat anemia, it is necessary to determine its type and cause of development. The main diagnostic method for this disease is laboratory blood tests (general and biochemical).
Changes that are observed in the general blood test:
small red blood cells (microcytosis).
Changes that are observed in the biochemical blood test:
In addition, a visual examination of the patient and a detailed history is required. Among the most common symptoms are pale skin and mucous membranes, cracks in the corners of the mouth, a “glossy” tongue, and an enlarged spleen.
To effectively correct the condition, instrumental examination methods may also be required:
computed tomography of the esophagus, stomach, duodenum. colonoscopy. Ultrasound of the liver, spleen, kidneys, genitals. X-rays of light.
Posthemorrhagic anemia
The main factors in the development of posthemorrhagic anemia are the phenomena of vascular insufficiency, hypovolemia with a decrease in the total volume of plasma and circulating formed elements, in particular, red blood cells that transport oxygen. This process is accompanied by a decrease in blood pressure, blood supply to internal organs and tissues, hypoxemia, hypoxia and ischemia, and the development of shock.
The degree of severity of the body's protective and adaptive reactions is determined by the volume, speed and source of bleeding. In the early reflex-vascular phase of compensation for blood loss (the first day), due to the stimulation of the sympathetic-adrenal system, vasoconstriction and increased resistance of peripheral vessels are observed, stabilization of hemodynamics due to the centralization of blood circulation with primary blood supply to the brain and heart, a decrease in the return of blood to the heart and cardiac output. The concentration of red blood cells, Hb and hematocrit are still close to normal (“hidden” anemia).
The second hydremic phase of compensation (2-3 days) is accompanied by autohemodilution - the entry of tissue fluid into the bloodstream and replenishment of plasma volume. Increased secretion of catecholamines and aldosterone by the adrenal glands and vasopressin by the hypothalamus contributes to the stability of the level of electrolytes in the blood plasma. There is a progressive decrease in red blood cells and Hb (total and per unit volume), hematocrit; the value of the color indicator is normal (posthemorrhagic normochromic anemia).
In the third, bone marrow phase of compensation (4-5 days), due to iron deficiency, anemia becomes hypochromic, the formation of erythropoietin by the kidneys increases with activation of the reticuloendothelial system, bone marrow erythropoiesis, and foci of extramedullary hematopoiesis. In the red bone marrow, hyperplasia of the erythroid lineage and an increase in the total number of normocytes are observed, in the peripheral blood there is a significant increase in the number of young forms of erythrocytes (reticulocytes) and leukocytes. Hb, red blood cell and hematocrit levels are decreased. Normalization of the level of red blood cells and Hb in the absence of further blood loss occurs after 2-3 weeks. With massive or prolonged blood loss, posthemorrhagic anemia becomes hyporegenerative in nature, and shock develops when the body's adaptive systems are depleted.
Treatment of anemia
The course of medical therapy is carried out on the basis of the diagnosis and includes the prescription of a special diet and medications, as well as, if necessary, surgical intervention to eliminate the causes of blood loss.
A balanced diet is of great importance for anemia. It compensates for the lack of iron and microelements involved in hematopoiesis. Nutritionists recommend eating foods rich in vitamin B12, folic acid and iron. The diet must contain meat, offal (liver, heart, tongue), fish, egg yolks, mushrooms, buckwheat, legumes, black currants, pomegranate, strawberries, nuts, apples, rose hip decoction, dried fruits. Vitamin C accelerates the absorption of iron by the body, while strong tea, coffee, and calcium hinder it. Strong alcoholic drinks are harmful to a patient with anemia.
Iron supplements are considered the most effective for combating anemia. They are better absorbed, increase hemoglobin levels faster, restore its reserves in the body, and eliminate weakness and fatigue. Based on blood test data for each patient, depending on a number of indicators (type of anemia, severity of the disease and the cause of its development, age of the patient), an individual daily dose, course duration, and preventive measures are calculated. In severe cases, intramuscular and intravenous administration of ampoule iron preparations in a hospital setting is possible to avoid adverse reactions and allergies.
It is advisable to take iron supplements one hour before meals or two hours after meals. Medicines should not be taken with tea or coffee. These drinks reduce iron absorption. You must use water or juice.
The prognosis for iron deficiency anemia is favorable in most cases. The patients' condition improves significantly, the body's resistance increases, sleep and appetite normalize. The basis for preventing anemia is a balanced diet. Do not get carried away with protein foods and sweets. There should be vegetables, herbs and fruits on the table all year round. Another rule is to maintain a healthy lifestyle, exercise, walks in the fresh air, proper rest and good sleep.
Sign up for an anemia screening
Make an appointment
Anemia - symptoms and treatment
Treatment should first of all be aimed at identifying and eliminating the root cause, so therapy for anemia lasts a long time, often accompanied by several medical specialists.
Indication for treatment
The indication for drug treatment is a decrease in hemoglobin levels to less than 120 g/l in women and below 130 g/l in men.
Basically, treatment involves restoring hemoglobin reserves, increasing the number of red blood cells, and normalizing hematocrit. The main effective method of treating iron deficiency anemia is the use of iron supplements orally or parenterally (intravenously or intramuscularly)
To restore the hemoglobin level in a patient with iron deficiency anemia, the dose of ferrous iron per day (only it is effectively absorbed) must be 100-300 mg, taking into account depleted iron reserves (about 1.5 g).
| Drug name | Components included in the drug | Fe dosage, mg | Dosage form of release | Daily dose, g |
| Conferon | succinic acid | 50 | Pills | 3-4 |
| Heferol | Fumaric acid | 100 | Capsules | 1-2 |
| Hemophere prolongatum | Ferrous sulfate | 105 | Dragee | 1-2 |
| Ferrogradumet | Plastic matrix - gradation | 105 | Pills | 1-2 |
| Aktiferrin | D, L-serine | 113,8 34,8 | Capsules Syrup | 1-2 1 teaspoon per 12 kg body weight |
| Ferroplex | Ascorbic acid | 10 | Dragee | 8-10 |
| Sorbifer Durules | Ferrous sulfate + Ascorbic acid | 100 | Pills | 1-2 |
| Tardiferon | Ferrous sulfate + mucoprotease | 80 | Pills | 1-2 |
| Fenyuls | Ascorbic acid, nicotinamide, B vitamins | 50 | Capsules | |
| Irovit | The same + ascorbic acid, cyanocobalamin, L-lysine | 100 | Capsules | 1-2 |
| Irradian | Ascorbic acid, folic acid, cyanocobalamin, L-cysteine, D-fructose, yeast | 100 | Dragee | 1-2 |
It is more effective to prescribe drugs with a higher content of ferrous iron; they should be taken orally (by mouth) 1-2 times a day. This is the most convenient approach for patients, and therefore their adherence to therapy increases. Many dosage forms of iron include ascorbic and succinic acids, fructose, cysteine, etc., they help the best absorption of iron in the gastrointestinal tract. Iron supplements are best tolerated if taken with food.
Treatment of iron deficiency anemia with parenteral forms of iron supplements
There are clear indications for such therapy:
- with impaired absorption from the intestine (absorption deficiency syndrome, resection of the small intestine, enteritis, etc.);
- exacerbation of chronic diseases of the gastrointestinal tract, such as peptic ulcer of the stomach or duodenum, Crohn's disease, ulcerative colitis;
- poor tolerance to iron-containing drugs when taken orally;
- if you need to quickly replenish iron reserves in the body.
For parenteral administration, iron preparations are used, such as Ferinject (intravenous), Ektofer (intramuscular), Ferbitol (intramuscular), Ferrum Lek (intramuscular, intravenous), Ferkoven (intravenous) [2].
Regarding the treatment of postpartum anemia, there are no clear conclusions about methods. Studies have shown that oral iron does not have a significant benefit over intravenous iron or placebo. However, oral iron does not cause life-threatening allergic reactions like intravenous iron. The clinical value of blood transfusion remains uncertain, in part because of the risks involved. This method can be used to treat postpartum anemia in cases of acute or severe bleeding during childbirth. However, it is not recommended after minor to moderate bleeding in stable patients with mild or asymptomatic anemia. In any case, it is necessary to assess the severity of anemia and consider the use of an iron-rich diet as a method of prevention and adjunct to treatment [7].
Iron deficiency anemia is the most common type of anemia. However, treatment for other types of anemia differs from treatment for IDA. With other types of anemia, to normalize blood counts, it is necessary, for example, to replenish vitamin B12, folic acid, control concomitant chronic diseases and other factors that were the root cause of anemia. To do this, you need a timely visit to a doctor who will diagnose and determine management tactics.
How to improve treatment. Diet
For all types of anemia, the diet should include foods high in iron: pork and beef liver, veal, beef, buckwheat, green apples, pomegranates, mushrooms, cabbage, beans and other legumes, dark chocolate, etc.
You need to eat 4-6 times a day. For normal digestion, food should be at room temperature; too cold or too hot food irritates the gastric mucosa, which prevents the absorption of beneficial elements. The amount of water you drink per day is 30 ml per 1 kg of weight, including tea, juice, soup, etc. Drinking alcohol and smoking are strictly prohibited. Alcohol not only negatively affects the health of the gastrointestinal tract, but also washes out beneficial components in the urine, which is harmful even for healthy people. Smoking increases stomach acidity, which can cause gastritis or ulcers. In this case, the absorption of beneficial microelements will be impaired.
For iron deficiency anemia, it is necessary to include fermented foods (kefir, kvass, sauerkraut, etc.). The acid contained in such products easily comes into contact with iron and prevents the formation of poorly absorbed iron phytates, resulting in improved penetration of iron into enterocytes (cells lining the inner surface of the intestine). The formation of iron phytates is also reduced if plant products are crushed or cooked [10].
Daily iron supplementation in menstruating women is an effective clinical public health strategy for alleviating anemia and iron deficiency, as well as increasing hemoglobin and iron stores. Daily iron supplementation also improves physical performance in women. In addition, there is evidence that iron supplementation reduces fatigue [8].
Daily oral iron and folic acid supplementation of 30–60 mg elemental iron and 400 μg (0.4 mg) folic acid is recommended for pregnant women to prevent anemia, puerperal sepsis, preterm birth, and low birth weight [9].
Contraindications for anemia
For anemia, strict diets are contraindicated; the diet should include foods high in iron, vitamin B12 and folic acid. The development of anemia is also possible while taking certain medications (antitumor drugs, a number of antibacterial, antiprotozoal, antiviral, anti-inflammatory, antirheumatic, antiepileptic and antipsychotic drugs). Therefore, taking this group of drugs for anemia should be under the supervision of a specialist.
Is it possible to treat anemia with folk remedies?
To date, there are no effective folk remedies for treating anemia, because correction of iron deficiency cannot be achieved only by changing diet or using any herbs, decoctions and juices. The reason for this is that the absorption of iron from food is limited (no more than 3-5% from plant foods), and in medications it is contained in higher concentrations.