When should you pay due attention to your health?
Everyone, without exception, is required to make an appointment with a doctor at least once a year to undergo a medical examination, including a general blood test.
For the reasons for the development of anemia, iron deficiency anemia occupies the leading positions - approximately 12% of the entire population of our planet suffers from this phenomenon.
What explains the spread of iron deficiency anemia? The reason may be a common deficiency of iron in food, impaired penetration of iron into the gastrointestinal tract and chronic bleeding.
The most common causes of bleeding are:
- Chronic hemorrhoids.
- Hemorrhoidal thrombosis.
- Failure of the menstrual cycle in females, which is reflected in intense and prolonged menstruation.
However, iron deficiency anemia may be one of the primary indicators of neoplasm development processes. Let's give an example: colon cancer - areas of tumor decay release blood into the intestinal lumen, but the person himself simply cannot notice this!
is anemia treatable?
Symptoms of anemia
Lack of hemoglobin leads to oxygen starvation, manifested by symptoms typical of anemia such as:
General weakness
With anemia, muscle tissue does not receive sufficient nutrition. The patient feels constantly tired, he does not have enough strength for normal life activities.
Drowsiness
The body lacks strength, which means it needs additional rest. Drowsiness develops. A person suffering from anemia is almost never alert; as a rule, he wants to sleep.
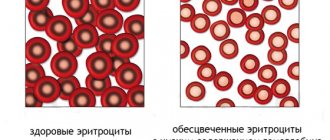
Pallor
Pale skin due to anemia is caused by a decrease in the number of red blood cells (erythrocytes) in the blood.
Dizziness
With anemia, the brain also receives insufficient nutrition. This may cause dizziness.
flickering
The flickering of “flies” before the eyes is caused by insufficient nutrition of the structures of the visual apparatus.
Fainting
If the decrease in hemoglobin is significant, fainting is possible - episodes of loss of consciousness.
Headache
With anemia, headaches are often observed.
More about the symptom
Cardiopalmus
You may experience palpitations with little physical activity or at rest.
More about the symptom
Dyspnea
Shortness of breath with anemia is caused by the fact that the body tries to compensate for the lack of oxygen by increasing its supply. Breathing becomes more frequent.
More about the symptom
What are the dangers of the anemia being studied?
It should be understood that even mild anemia can significantly harm the human body. Prolonged lack of oxygen causes metabolic disorders, accumulation of harmful substances in the body, and excessive stress on internal organs. Many people, unfortunately, today do not even know whether anemia can be treated .
In order to prevent the development of numerous chronic diseases, it is necessary to follow basic instructions:
Undergo regular medical examination - a healthy person in this case, as a rule, takes a general blood and urine test, does fluorography, makes an appointment with a therapist, gynecologist and dentist.
If you notice signs of chronic ailments that may subsequently lead to anemia, you must immediately consult a doctor for appropriate treatment.
is it possible to cure anemia
For the most part, this applies to representatives of the fairer sex with problems in the field of gynecology. Often women simply do not pay attention to heavy and painful menstruation and believe that this is in the order of things! It is worth noting that this is an erroneous opinion, since after therapy it is possible to restore the normal course of the menstrual cycle. In addition, long and intense menstruation in women after 40 years of age can be the primary symptom of cancer! Therefore, do not forget to ask yourself: is it possible to cure anemia and how to do it correctly.
Modern approaches to the treatment of iron deficiency anemia in patients with gynecological pathology
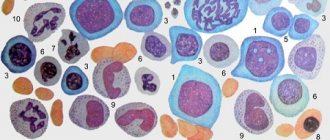
Anemia is a pathological condition characterized by a decrease in hemoglobin concentration and often accompanied by a decrease in the number of red blood cells per unit volume of blood [1]. According to the Ministry of Health of the Russian Federation, over the past 10 years, the frequency of anemia has increased 6.3 times, with iron deficiency anemia (IDA) being the most common (about 90% of all anemia). IDA is a hypochromic microcytic anemia that occurs as a result of a decrease in iron content in the body and is an independent nosological form [2].
In clinical practice, the most common classification of anemia is:
1) anemia caused by acute blood loss (posthemorrhagic); 2) anemia due to impaired erythrocyte production (aplastic, iron-deficient, megaloblastic, sideroblastic, etc.); 3) anemia due to increased destruction of red blood cells (hemolytic).
Depending on the severity of the decrease in hemoglobin levels, three degrees of severity of anemia are distinguished:
- mild - hemoglobin level above 90 g/l;
- average - hemoglobin within 90–70 g/l;
- severe - hemoglobin level less than 70 g/l.
The prevalence of iron deficiency conditions (IDC) in women of childbearing age in some regions of the Russian Federation reaches 30–60%, and according to the World Health Organization, the total number of people with iron deficiency in the world is about 600 million people [3]. VDNs cause increased susceptibility to acute respiratory viral infections and decreased performance.
In gynecology, there are three stages of VDS in the body:
- Prelatent iron deficiency is a hidden iron deficiency; the body accumulates iron with the help of ferritin, an iron-containing protein. If its indicator is low, then they speak of the presence of prelatent iron deficiency.
- Latent iron deficiency - at this stage, along with ferritin, tissue reserves of iron are depleted with optimal hemoglobin levels, no clinical symptoms of iron deficiency are observed, a compensatory increase in iron absorption occurs in the intestine, and the activity of iron-containing enzymes gradually decreases.
- Explicit iron deficiency is characterized by a decrease in the number of erythrocytes and a decrease in the level of hemoglobin, which is part of erythrocytes and is a substance that transports oxygen to the body tissues from the lungs, the development of dystrophic changes in organs and tissues, as well as an increased amount of protoporphyrin in erythrocytes [2, 4] .
The high prevalence of anemia among women is due to the fact that the female body always experiences a lack of iron due to regular blood loss. The human body is designed in such a way that it can recover only 2 mg of this mineral per day from food, subject to proper nutrition (eating enough vegetables and meat) [2]. Thus, menstrual blood loss, despite its “objectivity,” can cause the development of iron deficiency in a woman’s body. During menstruation, normal blood loss is 30–50 ml, and the body loses 15 mg of iron [4, 5]. And if menstruation is heavy and lasts more than 7 days, then iron loss is more than 50 mg. As a consequence, in such cases the need for iron increases many times [6].
Iron deficiency occurs more often in women aged 30–40 years. As a rule, this occurs during pregnancy and breastfeeding (both the fetus and the infant directly receive iron from the mother). We also must not forget about blood loss during childbirth. Women may not be aware that they have a similar problem, although they regularly undergo blood tests during pregnancy. Iron deficiency in the body is diagnosed, unfortunately, only at the third stage. Most women get tired quite quickly and feel overwhelmed even with a slight decrease in ferritin levels. When the body lacks iron, dizziness and headaches occur.
In order to replenish iron reserves and restore blood loss during normal erythropoiesis, the iron contained in food is sufficient. During hormone replacement therapy with erythropoiesis-stimulating drugs, adequate intake of iron into the body optimizes the prescribed treatment. It should be noted that in many cases, the intravenous route of iron administration is more effective than the oral route, as it provides the ability to quickly saturate the body with the iron it needs [7]. This is especially important in the treatment of anemia occurring against the background of chronic diseases. The intravenous route of iron administration helps to overcome the blockage of iron absorption from the gastrointestinal tract (GIT) and create its reserve in the body.
IDA is currently a social disease with a fairly wide prevalence. In pregnant women, it is a condition caused by a reduction in iron content in the bone marrow and blood serum due to its high costs for the formation of the fetoplacental complex, as well as redistribution in favor of the fetus. A natural consequence of iron deficiency is a disturbance in the formation of hemoglobin with the development of both hypochromic anemia and trophic tissue disorders.
IDA remains a serious pathology in modern gynecology, as the frequency of this disease does not decrease. In pregnant women, the incidence of anemia varies between 15–80%, and in 98% of women, anemia during pregnancy is of a pronounced iron deficiency nature [2, 8].
Only iron-containing preparations can balance the iron content in the female body.
A lack of enzymes containing iron can cause various trophic changes in the body of a pregnant woman. Along with these changes, cracks appear in the corners of the mouth, yellowness of the palms, nails become brittle, hair falls out, etc. This disease is sometimes manifested by “exotic” gastronomic preferences. In a severe form of iron deficiency, a decrease or increase in blood pressure, swelling, palpitations, and heart failure may occur. The volume of circulating blood increases, the need for oxygen increases, and, as a result, iron deficiency complicates the course of pregnancy and childbirth, which in turn has an extremely negative effect on the development of the fetus.
The main risk factors for the occurrence and development of IDA in pregnant women include the presence of chronic diseases or anemia before pregnancy, chronic diseases of internal organs or infectious diseases, multiple pregnancy, early toxicosis, hemoglobin level less than 120 g/l in the first trimester, duration of menstruation for several years before pregnancy more than 5 days [9].
Every day a woman consumes from 10 to 20 mg of iron with food, of which less than 2 mg is completely absorbed, and during menstruation, up to 75% of healthy women lose from 20 to 30 mg of iron [10, 11]. This amount of iron cannot be absorbed even with its high content in food. Thus, an imbalance occurs, leading to the development of anemia.
During pregnancy, childbirth and breastfeeding, the cumulative loss of iron is approximately 1 g, and it takes approximately 4 years for the female body to replenish its iron supply exclusively from dietary sources. Consequently, if a woman gives birth again during this period, she will inevitably develop iron deficiency [5].
Modern clinical recommendations include the need for all pregnant women to take iron-containing medications in the second and third trimesters of gestation. For adult non-pregnant women, the daily dose (18 mg of iron) is rarely covered solely by diet [4, 9]. That is why, by the beginning of pregnancy, almost half of all women have minimal iron reserves.
According to modern data, at the end of the gestational process, iron deficiency develops without exception in all pregnant women, both in latent and overt form. This is mainly due to the fact that pregnancy is always accompanied by additional iron losses: 320–500 mg of iron is spent on increased cellular metabolism and an increase in hemoglobin, 50 mg of iron for an increase in the size of the uterus, 100 mg of iron for the construction of the placenta, 400–500 mg iron - to the needs of the fetus [6].
As a result, the fetus, taking into account the reserve fund, is provided with sufficient amounts of iron, but pregnant women often develop VHD of varying severity. To assess whether the iron supply corresponds to the norm, the level of serum ferritin is determined, which, if its values are less than 30 μg/L, is considered reduced.
Reduced prenatal hemoglobin concentration (especially iron deficiency) is a risk factor for postpartum hemorrhage, correlating with the severity of the woman’s condition against her background. By using intravenous iron supplements during the prenatal period to correct IDA, doctors strive to minimize both the risk of bleeding and the need for blood transfusions during the perinatal period. In the postnatal period (from 0 to 6 months), iron deficiency is observed in 13% of mothers, and 10% of women are diagnosed with anemia. Oral forms of iron supplements act rather slowly and often do not provide the required effect [2, 11].
Intravenous iron is clearly a safe alternative, reducing both the need for and the volume of blood transfusions. Treatment with intravenous iron supplements can achieve a significant increase in iron stores and significantly increase the concentration of hemoglobin in the blood.
With the exception of severe cases, IDA is treated during pregnancy on an outpatient basis. To treat it, doctors prescribe medications containing this element. As a rule, they are used for a long time (from 15 weeks to 6 months). The level of hemoglobin in the blood rises smoothly, no earlier than the third week from the start of treatment. The indicator returns to normal approximately 2 months after the start of therapy [9, 11]. At the same time, the woman’s health and well-being improves. However, it is important not to interrupt the course of treatment, since as the gestational age increases, the fetus also grows and its iron needs, accordingly, also increase.
We should not forget about the woman’s upcoming birth, which, in turn, entails a significant waste of energy and blood loss. Next comes the period of breastfeeding the baby, which also causes a lack of iron. Therefore, experts recommend continuing maintenance treatment with iron supplements for another 6 months during the postpartum period [11, 12]. In order to determine the lack of iron in the female body in time, the symptoms should be considered both in combination and individually.
Modern studies have shown a high need for transfusions of blood components in patients with severe uterine bleeding, which increases the cost of hospitalization and reduces the overall quality of life. Oral administration of iron-containing drugs to eliminate VDN in women with menorrhagia allows avoiding red blood cell transfusions in all known cases, except for a pronounced drop in hemoglobin levels, when oral forms cannot fully compensate for iron loss [12].
Today in Russia, unfortunately, medications containing large amounts of iron per tablet are widely used. The toxic effects of therapy that manifest themselves in this case were considered inevitable, and in order to prevent them, it was usually recommended to take the drug with food to bind free iron ions and thereby prevent their negative effect on the gastrointestinal tract. The paradox is obvious: significant doses of iron were recommended, but the binding of iron by food proteins at the same time reduced its intake many times over. The resulting therapeutic effect did not depend in any way on the high dose of iron in the drug [5, 6].
When choosing an iron supplement, there are a number of factors to consider. Since ionized iron from the gastrointestinal tract is absorbed exclusively in divalent form and ascorbic acid plays a huge role in this process, its presence in the preparation is extremely important. In hematopoiesis, folic acid is of great importance, which enhances nucleic acid metabolism. Also, cyanocobalamin is important for the normal metabolism of folic acid, which is a key factor in the formation of its active form.
Deficiency of these substances, which occurs quite often with anemia associated with blood loss, leads to disturbances in DNA synthesis in hematopoietic cells, while the inclusion of these components in the drug increases the active absorption of iron in the intestine and its further utilization, and releases additional amounts of ferritin and transferrin [ 13]. As a result, the rate of hemoglobin synthesis increases, and the effectiveness of therapy for both IDA and other IDA increases.
The only iron preparation for intravenous administration in the USSR was Ferrum Lek. In Russia, the following drugs are approved for intravenous replenishment of iron deficiency: Venofer, CosmoFer and Likferr (of which the domestic Venofer). In many countries, new generation drugs with improved characteristics are used - Ferinject (iron carboxymaltose), Ferumoxytol (supermagnetic iron oxide nanoparticles) and Monofer (iron (III) hydroxide oligoisomaltose 1000) [5, 13, 14].
A Danish pharmaceutical company, a global expert in the development of iron-containing drugs, has created a new highly effective iron preparation for intravenous use, with minimal restrictions in its prescription. The organization is working on clinical programs to further confirm the safety, effectiveness and ease of use of Monofer as a modern treatment for IDA.
The drug Monofer (iron (III) hydroxide oligoisomaltose 1000) was created on the basis of matrix structure technology with alternating fragments of oligoisomaltose 1000 and iron (III) hydroxide, which ensures low toxicity of the drug [14, 15]. Due to its low toxicity, Monofer can be prescribed in a high dose, creating the possibility of correcting VSD in just one visit.
The main safety factors of Monofer include: the absence of a test dose, low risk of anaphylactic reactions, minimal risk of toxicity due to the presence of free iron in the drug. The ease of use of Monofer is based on the possibility of high (up to 20 mg/kg) and fast (up to 60 min) infusion rates due to the low toxicity of the drug [15].
The matrix structure of the drug includes tightly bound and stable iron, promoting a slow and controlled release of iron-containing proteins of bioactive iron with minimal risk of toxicity due to the presence of free iron (Fig.) [10].
New generation iron preparations have a lower content of free iron in their composition, in contrast to older iron preparations. Monofer provides for each patient with IDA a convenient dosage range in the form of:
- intravenous drip infusion: 200–1000 mg (prescribed once a week until iron deficiency is completely restored):
a) 11–20 mg/kg – 60 minutes (you must add 100 to 500 ml of sterile NaCl solution 0.9%); b) 6–10 mg/kg – 30 minutes; c) 0–5 mg/kg – 15 minutes;
- intravenous bolus injection: 100–200 mg per week up to 3 times (rate 50 mg/min). Can also be dissolved in 10–20 ml of sterile 0.9% NaCl solution [12].
If the patient's need for iron replenishment exceeds 20 mg/kg, the dose of Monofer must be divided and prescribed with a time interval of at least one week. Infusions of the drug over 1000 mg are prescribed exclusively in hospital settings. The drug should be prescribed to patients with a diagnosis of IDA, confirmed by appropriate laboratory data (results of determining the concentration of hematocrit and hemoglobin, serum ferritin, the number of red blood cells and their parameters - the average content of hemoglobin in an erythrocyte, the average volume of an erythrocyte or the average concentration of hemoglobin in an erythrocyte).
It should be noted that in one syringe Monofer can be mixed exclusively with sterile saline solution. It is prohibited to add other therapeutic drugs and solutions for administration, as there is a risk of not only precipitation, but also other pharmaceutical interactions.
It is important to avoid penetration of the drug into the perivenous space, since its entry beyond the boundaries of the vessel leads to brown discoloration of the skin and tissue necrosis. In case of such complications, to speed up the removal of iron and prevent its deeper penetration into nearby tissues, it is recommended to apply a heparin-containing drug to the injection site (the ointment or gel is applied without rubbing, with light movements) [16].
Contraindications to the use of the drug:
- non-iron deficiency anemia (eg, hemolytic anemia);
- high sensitivity to the active substance and excipients included in the drug;
- the presence of various signs of iron overload (hemosiderosis, hemochromatosis) or disruption of iron utilization processes;
- rheumatoid arthritis in combination with symptoms of inflammatory processes;
- cirrhosis and hepatitis of the liver (stage of decompensation);
- bacteremia;
- children under 18 years of age (due to insufficient proven data on safety and effectiveness) [3].
Iron preparations administered parenterally can cause hypersensitivity reactions, in particular anaphylactic shock, due to the risk of developing allergic reactions in patients with eczema, polyvalent allergies, bronchial asthma, allergic reactions to other parenteral iron preparations, with systemic lupus erythematosus, acute and chronic infectious diseases, rheumatoid arthritis, etc. the use of the drug is limited. Episodes of a sudden significant decrease in blood pressure are also possible with a high rate of administration of Monofer.
Thus, the use of the drug is recommended in clinically justified cases. It is important to carefully evaluate the benefit/risk ratio to decide on the use of Monofer during pregnancy. If the expected benefit to the mother outweighs the risk to the fetus, then treatment can be carried out in the second and third trimesters of pregnancy. The use of the drug in the first trimester of pregnancy is not recommended [3, 17].
The excretion of Monofer into breast milk has not been established to date. Therefore, the drug can be used during lactation.
Monofer should not be prescribed simultaneously with various dosage forms of iron for oral administration, since their combined use helps reduce the absorption of iron from the gastrointestinal tract. Treatment with oral iron supplements begins no earlier than 5 days after the last injection. The drug is well tolerated and has low toxicity. In this regard, the risk of overdose is minimal. However, an overdose can develop due to acute iron overload or iron accumulation and is expressed by symptoms of hemosiderosis. The level of iron in the body is monitored by determining the degree of ferritin concentration.
The obtained research results showed that the prevention of anemia in women with the drug Monofer helps to reduce the incidence of various diseases associated with iron deficiency [18]. In addition, in the absence of IDA, circulatory and hemic hypoxia disappears, which, in turn, prevents the development of metabolic disorders and leads to a decrease in the incidence of complications such as fetoplacental insufficiency, gestosis, premature birth and labor anomalies. The absence of severe side effects of the drug and a convenient dosage regimen indicate that Monofer is well tolerated.
Thus, among the main advantages of Monofer in gynecology are the following: a wide range of indications for use, convenient dosing and a high safety profile. The use of Monofer ensures high effectiveness of both prevention and treatment of IDA.
Today, there is a large evidence base from various clinical studies confirming the effectiveness and safety of intravenous iron administration in a variety of clinical situations associated with various VDNs. Analysis of studies comparing the results of oral and intravenous forms of iron supplementation indicates equal or higher effectiveness of the latter form. Also, modern studies emphasize such disadvantages of the oral form of administration of iron-containing drugs as side effects, non-compliance with doctor’s instructions, low absorption, as well as the impossibility of prompt compensation for iron loss and maintaining its adequate concentration, characteristic of patients with ongoing blood loss.
The introduction into clinical practice of isomaltose hydroxide 1000, which does not require a test dose, with the possibility of parenteral administration in a short time of high doses, brings additional advantages in therapy with intravenous iron preparations. Also, unlike the oral form, it is the intravenous route of administration of iron supplements that allows one to overcome anemia that develops against the background of chronic diseases.
Literature
- Kulikov A. Yu., Skripnik A. R. Pharmacoeconomic analysis of the drug “Monofer” in the treatment of iron deficiency anemia // Pharmacoeconomics: theory and practice. 2021, 4: 183–186.
- Lebedev V. A., Pashkov V. M. Principles of treatment of iron deficiency anemia in gynecological patients // Difficult patient. 2013, 11: 3–7.
- Nordfjeld K., Andreasen H. Pharmacokinetics of iron isomaltoside 1000 in patients with inflammatory bowel disease // Drug. Des. Devel. Therapy. 2012, 6: 43–51.
- Malkoch A.V., Anastasevich L.A., Filatova N.N. Iron deficiency conditions and iron deficiency anemia in women of childbearing age // Attending Physician. 2013; 4:37–41.
- Mubarakshina O. A., Somova M. N., Lyubavskaya S. S. Pharmacological correction of iron and magnesium deficiency during pregnancy. Voronezh State Medical Academy named after. N. N. Burdenko. 2014; 4:52–60.
- Podzolkova N.M., Nesterova A.A. Iron deficiency anemia in pregnant women // Russian Medical Journal. 2003, 5: 326–331.
- Morrison J., Patel ST, Watson W. Assessment of the prevalence and impact of anemia on women hospitalized for gynecologic conditions associated with heavy uterine bleeding // J. Reprod. Med. 2008, 5: 323–330.
- Protopopova T. A. Iron deficiency anemia and pregnancy // Russian Medical Journal. 2012; 17:862–867.
- Chushkov Yu. V. Modern possibilities for correcting iron deficiency in obstetrics and gynecology // Gynecology. 2011; 6:44–47.
- Bhandari S. A hospital-based cost minimization study of the potential financial impact on the UK health care system of introduction of iron isomaltoside 1000 // Clin Risk Manag. 2011, 7: 103–113.
- Dvoretsky L.I. Algorithms for the diagnosis and treatment of anemia // Russian Medical Journal. 2003, 8: 427–433.
- Coyne D. From anemia trials to clinical practice: understanding the risks and benefits when setting goals for therapy // Semin Dial. 2008, 21: 212–216.
- Lebedev V. A., Pashkov V. M. Principles of treatment of iron deficiency anemia in gynecological patients // Difficult patient. 2013, 11: 3–7.
- Gupta DR, Larson DS, Thomsen LL Pharmacokinetics of Iron Isomaltoside1000 in Patients with Stage 5 Chronic Kidney Disease on Dialysis Therapy. 2013, 03: 4172/2157–7609.
- Hildebrant P., Brunn N. et al. Effects of administration of iron isomaltoside 1000 in patients with chronic heart failure. A pilot study. Transfusion Alternatives in Transfusion Medicine // 2010, 11: 131–137.
- Locatelli F. Iron treatment and the TREAT trial // NDT +. 2011, 4: 13–15.
- Pasricha SR, Flecknoe-Brown SC Diagnosis and management of iron deficiency anemia: a clinical update. 2010, 9: 50–62.
- Philip A. Kalra, Sunil Bhandari, Sanjiv Saxena. A randomized trial of iron isomaltoside 1000 versus oral iron in non-dialysis-dependent chronic kidney disease patients with anemia // Nephrol Dial Transplant. 2015, 3: 1–10.
A. Z. Khashukoeva*, 1, Doctor of Medical Sciences, Professor M. I. Agaeva* M. Z. Dugieva*, Doctor of Medical Sciences T. N. Sukhova** L. I. Abdurakhmanova*
* Federal State Budgetary Educational Institution of the Russian National Research University named after. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow ** OSP RGNKTs Federal State Budgetary Educational Institution of Higher Education Russian National Research Medical University named after. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
1 Contact information
Modern approaches to the treatment of iron deficiency anemia in patients with gynecological pathology / A. Z. Khashukoeva, M. I. Agaeva, M. Z. Dugieva, T. N. Sukhova, L. I. Abdurakhmanova
For citation: Attending physician No. 12/2017; Issue page numbers: 23-29
Tags: women, iron, intravenous drugs
Prevention of anemia
The main measures to prevent the disease are:
- proper nutrition - avoiding fast food and other junk food, introducing foods rich in iron and vitamins (especially group B) into the diet;
- rejection of bad habits;
- timely treatment of diseases that can lead to anemia;
- normalization of work and rest regimes;
- regular sanitation of foci of chronic infection in the body;
- avoiding excess vitamin C in the body;
- prevention of helminthiases, and if they occur, then timely treatment;
- giving up a sedentary lifestyle - physical exercise, regular walks in the fresh air;
- avoidance of stress and other psycho-emotional disorders;
- use of personal protective equipment when working in hazardous industries;
- additional intake of iron supplements during heavy periods, with chronic or acute bleeding;
- refusal of uncontrolled use of medications, all medications should be prescribed only by the attending physician, self-medication is unacceptable;
- timely consultation with a doctor when the first suspicious symptoms appear - this will allow you to diagnose anemia at an early stage, which will significantly facilitate subsequent treatment and improve the prognosis of the disease.
How to diagnose ACD?
● Hemoglobin is reduced.
● Red blood cell size (MCV) is normal, less often reduced (unlike iron deficiency anemia).
● The hemoglobin content in erythrocytes (MCH) is normal, less often below normal. *Thus, most often anemia of chronic diseases is normocytic normochromic anemia.
● An important feature that distinguishes iron deficiency anemia from ACD is a decrease in ferritin. In ACD, the ferritin level remains normal or increases as an acute phase protein of inflammation/infection or a tumor marker in cancer.
● When diagnosing ACD, one must answer the question: “Is iron deficiency absolute (true) or functional (redistribution)?” Treatment tactics will be different: in the first case, prescribing iron supplements will lead to rapid compensation of the deficiency and recovery, in the second, taking them will be useless.
Homemade recipe for anemia
Homemade raw beet smoothie recipe.
To prepare it you will need the following products:
- Beets as a source of folic acid, potassium, sodium. Beets perfectly cleanse the intestines, removing putrefactive bacteria from it. Raw beets are especially useful, as they contain a large amount of fiber.
- Peeled orange.
- Four dates.
- Black currant – 70 g.
- Peeled almonds.
The beets are finely chopped, placed in a blender, and nuts and dates, berries and pitted orange are added there. Pour everything into 0.5 cups of water and grind in a blender. The smoothie for raising hemoglobin is ready.
Video recipe for beetroot and berry smoothie:
Freshly squeezed juices in the treatment of anemia
This traditional method of treating anemia has been tested by many people. One of the readers was in the hospital, and after she was discharged, she could not come to her senses for a long time. I read that you can drink a vitamin cocktail. I started making it and drinking it. The level of hemoglobin in the blood normalizes in the body, and the general condition of the body improves. Then she talked with other people who also confirmed that this recipe works and, most importantly, does absolutely no harm to the sick person. Only benefit.
Freshly squeezed juices can be a great help in the fight against anemia. For this purpose, you can use a vitamin cocktail, which contains pomegranate, lemon, apple and carrot juice. Be sure to add honey to the drink.
The proportions should be as follows:
- Pomegranate juice – 0.2 l.
- Apple juice – 0.1 l.
- Carrot juice – 0.1 l.
- Lemon juice – 0.1 l.
- Honey – 70 g.
It is better to start drinking juice with 2 tablespoons to check the body’s reaction. If the body responds well, then increase the dosage up to a full glass 1-3 times a day.
Factory juices cannot be used to prepare cocktails. They must be freshly pressed. When all the components of the drink are ready, you just need to mix them.
Useful information: if any ingredient does not suit you, you can exclude it or replace it with any other vegetable or fruit. Just remember that you can’t drink a lot of fruit juices because of the high sugar content!
Video recipe:
Other folk remedies
To treat anemia, you can use the following recipes:
- Boiled or pickled beets. It is eaten in its pure form and added to various dishes. You can also squeeze juice from the vegetable, leave for 3-4 hours and drink 1/4 or 1/3 glass 3-4 times a day. The course of treatment is 3-4 weeks. The juice cannot be stored; it is prepared every day.
- 100 g of raw chopped carrots with the addition of butter or sour cream can also be eaten to treat anemia.
- You can pour a tablespoon of crushed Jerusalem artichoke flowers into three glasses of boiling water. Cover the pan with a towel and leave for 8 hours, then filter and consume 1/2 cup 3-4 times a day 15 minutes before meals.
- You need to eat garlic every day, which helps get rid of anemia.
- It is beneficial to eat fresh cucumbers every day without peeling them. It is also good to drink a glass of cucumber juice a day.
- Pumpkin is useful for treating anemia. It is consumed 4-5 times a day, 150-200 g each. You can eat pumpkin pulp raw or boiled.
- You can get rid of anemia with milk and dill. Pour the greens or plant seeds into a glass of milk and bring to a boil. Then reduce the heat and simmer for another 10 minutes. Take 1/3 cup 3 times a day.
- It is useful for anemia to eat greens and celery root every day. It is also good to take 1-2 teaspoons of freshly squeezed celery juice 20 minutes before meals.
- Spinach, which is added to salads, is an excellent remedy for anemia. You cannot store prepared salad with this plant, as it produces toxic substances. However, whole leaves can be kept in the refrigerator for 30 days.
- Zucchini helps prevent the development of anemia. They are eaten fresh without peeling.
You can learn more than 100 traditional medicine recipes from the video below:
How to treat anemia of chronic diseases?
1. Treatment of the underlying disease.
The pathogenesis of anemia is discussed above - to understand that in case of ACD, the underlying disease must first be treated . By reducing the activity of the inflammatory process in the body, we enable iron to be absorbed from the gastrointestinal tract if it is deficient. There are situations when this is not possible. The only consolation is that ACD develops slowly and is often of mild severity.
2. Transfusion of red blood cells and erythropoiesis-stimulating drugs , with or without combination with intravenous iron supplements - for severe anemia.
In any case, the treatment of ACD should be carried out by competent specialists; self-diagnosis and self-medication should not exist here.