Take the first step
make an appointment with a doctor!
Pregnancy is a happy time in the life of every woman, but, unfortunately, it is often overshadowed by various diseases. These include hepatosis in pregnant women, the symptoms of which most often begin to appear in the third trimester. Just a few years ago, this disease was very rare in medical practice; only one out of 16,000 expectant mothers suffered from it. But recently, an increasing number of pregnant women are faced with this unpleasant disease. Hepatosis in pregnant women is a degenerative liver lesion, manifested in impaired bile formation and bile flow.
Causes of hepatosis in pregnant women
Doctors turned their attention to this disease relatively recently, so experts are still arguing about what causes its appearance. Most medical minds agree that hepatosis in pregnant women is caused by certain genetic characteristics or disorders and can be transmitted through the female line. These genetic abnormalities may not manifest themselves in any way throughout life. But sometimes pregnancy, which brings with it an increase in body weight, hormonal imbalances and an increased load on the body in general and on the liver in particular, gives impetus to the development of hepatosis. The liver is also very susceptible to the influence of pregnancy hormones. For example, estrogen.
The main factors that increase the risk of this disease include:
- Incorrect intake of vitamins. Vitamins are always an additional burden on the liver. Many vitamin complexes contain increased amounts of various components, which cause liver dysfunction, so they need to be taken correctly, taking into account age, body weight, dosage and stage of pregnancy.
- Dietary disorder. Overeating and eating salty, fried, smoked, fatty foods, as well as foods rich in chemical additives, overload the liver and impair its functioning.
- Insufficient physical activity. If the expectant mother moves little, then little energy obtained from food is consumed, and the metabolism, which is already slowed down by pregnancy, slows down.
Take the first step
make an appointment with a doctor!
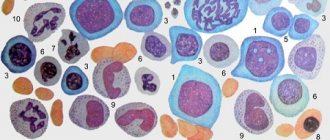
Biochemical blood test / “9 months”
Return to list
No. 3, March 2008.
During 9 months of pregnancy, the expectant mother has to undergo a considerable number of tests. Why is this necessary and what do their results mean?
A biochemical blood test allows you to evaluate the functioning of many internal organs - kidneys, liver, pancreas, etc. In addition, a biochemical blood test shows which microelements are missing in a woman’s body. Since various changes associated with metabolic processes occur during pregnancy, assessment of biochemical blood parameters is important for the timely diagnosis of pathological conditions that may arise in the body of the expectant mother.
Let us list the main indicators of a biochemical blood test.
Total protein is an indicator of protein metabolism, reflecting the total content of all proteins in the blood serum. The normal concentration of total protein in the blood is 63-83 g/l. Plasma proteins are divided into groups with different structures and functions, which are called protein fractions. Among the protein fractions, albumins and alpha, beta, and gamma globulins are distinguished. Their definition and correlation allows a more accurate assessment of dysfunctions of internal organs. Physiological hypoproteinemia (decreased protein levels) can be observed in pregnant women (especially in the third trimester) and during lactation due to a decrease in the number of red blood cells in plasma associated with an increase in total plasma volume. A slight decrease in total protein (55-65 g/l) during pregnancy is not a pathology. An increase in protein concentration in the blood serum is observed due to pathology - dehydration and thickening of the blood due to fluid loss.
Lipids (fats) - there are 4 main groups of lipids in the blood: cholesterol (cholesterol), triglycerides, phospholipids, fatty acids. Cholesterol is the most important indicator of lipid metabolism, serves as a structural component of cell membranes, participates in the synthesis of sex hormones, bile acids, vitamin D. There are fractions of low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL) and some others, differing in composition and functions. The level of cholesterol in the blood largely depends on age. The normal level of cholesterol in the blood of a young woman is 3.15-5.8 mmol/l. During pregnancy, there is a physiological increase in the level of total cholesterol (up to 6.0-6.2), which is due to the increased formation of endogenous (produced in the liver) cholesterol, necessary for the construction of the vascular bed of the placenta and fetus. An increase in cholesterol levels in the blood is considered a factor predisposing to the development of atherosclerosis - the formation of specific plaques in blood vessels.
Carbohydrates are the main source of energy for the body.
Glucose is a source of energy and a component of the vital activity of any cell in the body. The normal blood glucose concentration in adults is 3.9-5.8 mmol/l. In healthy pregnant women, glucose levels may be slightly reduced (to 3.5-4.0 mmol/L) as the growing fetus consumes increasing amounts of glucose.
During pregnancy, the body's increased need for insulin (a pancreatic hormone that regulates carbohydrate metabolism) exceeds the functional capacity of pancreatic cells that produce insulin. This may result in insufficient secretion to maintain normal blood glucose levels. During this period, in some pregnant women, a relative lack of insulin can cause the development of gestational diabetes (pregnant diabetes), as evidenced by an increase in blood glucose. blood glucose testing is recommended for all expectant mothers between the 24th and 28th week . This analysis is carried out additionally, without examining other indicators of biochemical analysis.
specific proteins called enzymes participate as catalysts in all biochemical reactions . Each reaction involves its own specific enzyme, so their number is in the hundreds. In this case, only a few dozen enzymes have diagnostic value.
Alanine aminotransferase (ALT) - normally in women it is up to 32 U/l. The highest ALT activity is detected in the liver and kidneys. ALT levels increase when liver and kidney cells are damaged by viruses or chemicals.
Aspartate aminotransferase (AST) - normally in women it contains up to 30 U/l. AST is found in heart, liver, nerve, and kidney tissues; accordingly, it is determined in order to identify the pathology of these organs. During normal pregnancy, ALT and AST levels do not change. A slight increase in transaminases is observed with mild to moderate gestosis. A multiple increase in the activity of ALT (up to 100 IU/l) and AST (up to 160 IU/l) is observed with severe gestosis. This result indicates that the liver cannot cope with the load.
Alkaline phosphatase is present in almost all tissues of the body. The highest activity of alkaline phosphatase is found in the cells of bone tissue, liver, kidneys, intestinal mucosa and placenta. An increase in blood alkaline phosphatase activity is associated mainly with bone diseases and liver pathology. In pregnant women, especially in the third trimester, there is also a physiological increase in the activity of this enzyme; in this case, the placenta is an additional source of alkaline phosphatase. Normal values of alkaline phosphatase in adults are up to 150 U/l. In pregnant women, this figure can increase to 240 U/l.
Pancreatic amylase is synthesized by pancreatic cells. Normally, adults contain up to 50 U/l. The level of pancreatic amylase in the blood increases with pathology of the pancreas.
Pigments are colored organic substances. Bile pigments (bilirubin and urobilinogen) and porphyrins (red pigments) are of diagnostic importance.
Bilirubin is a bile pigment that is formed as a result of the breakdown of hemoglobin, the pigment in red blood cells to which oxygen attaches. When hemoglobin breaks down, free bilirubin is initially formed, which is transported from the spleen to the liver in combination with albumin. Then, in the liver, free bilirubin binds to a special acid (glucuronic acid), resulting in the formation of direct, less toxic bilirubin, which is actively released into the bile ducts and excreted with bile. It is one of the main components of bile. Bilirubin is contained in blood serum in the form of two fractions : direct (bound) and indirect (free) bilirubin , together making up the total blood bilirubin . The normal level of total bilirubin, including during pregnancy, is 3.4-17.2 µmol/l. When the concentration of bilirubin in the blood increases (with accelerated breakdown of red blood cells, pathology of the liver or biliary tract), jaundice appears . This is due to the fact that in hyperbilirubinemia, bilirubin accumulates in the eyeball and skin.
Nitrogenous substances are the end products of the breakdown of proteins and nucleic acids - urea, creatinine, creatine, ammonia, uric acid. But in blood biochemistry, urea and creatinine are determined mainly.
Urea - serum urea levels, along with creatinine, are used to assess renal excretory function. The normal concentration of urea in the blood is 2.5-6.3 mmol/l. An increase in the concentration of urea in the blood is observed in various kidney diseases.
Creatinine - normal creatinine values in women are 53-97 µmol/l. An increase in serum creatinine indicates a decrease in the level of renal filtration (decreased kidney function). Blood creatinine concentrations in pregnant women are physiologically reduced (by 40%) due to increased blood volume, increased renal plasma flow and filtration, especially in the second and third trimesters of pregnancy. For pregnant women, the normal creatinine level is 35-70 µmol/l.
Microelements are chemical substances whose content in the body ranges from a few micrograms to several nanograms. But, despite such a small amount, they play a significant role in all biochemical processes of the body.
Iron is a vital trace element involved in oxygen transport. The normal iron level in women is 8.95-30.4 µmol/l. Iron is part of erythrocyte hemoglobin, muscle myoglobin and some enzymes. With iron deficiency, iron deficiency anemia develops - the most common pathology of pregnancy, observed mainly in the second or third trimester due to insufficient satisfaction of the increased need of the mother and fetus for substances necessary for hematopoiesis. However, with normal hemoglobin levels, low iron levels may occur, which is an indicator of hidden iron deficiency anemia - which is why it is important to monitor iron levels in a biochemical blood test during pregnancy. The greatest loss of iron occurs during bleeding.
Sodium is the most important component of the extracellular space, which is associated with the regulation of water distribution in the body. The normal sodium concentration is 136-145 mmol/l. Sodium is involved in the mechanisms of excitation of nerve and muscle cells. A decrease in its level in plasma causes general weakness and can lead to the development of various neurological disorders. An increase in sodium concentration in the blood is observed when water intake is limited, vomiting, for example, during toxicosis of the first half of pregnancy or diarrhea (loose stools) without replacing fluid loss.
Potassium is the main intracellular microelement. The normal potassium level in adults is 3.5-5.5 mmol/l. Hyperkalemia is observed in renal failure and drug overdose. When potassium levels decrease, which can occur with diarrhea and vomiting, heart rhythm disturbances, muscle weakness, and decreased muscle tone develop.
Calcium is the main component of bone tissue. The normal calcium concentration in young women is 2.20-2.55 mmol/l. Calcium performs many functions in the body: it participates in the processes of muscle contraction, hormone secretion, regulation of the activity of many enzymes, and blood clotting. Calcium deficiency is observed during pregnancy, which is explained by the child’s need for building material for bones. If calcium in the analysis decreases, it is necessary to replenish its content with the help of medications.
Phosphorus - the main part of it is found in bone tissue in the form of calcium salts, the rest is mainly in soft tissues. The normal phosphorus concentration for an expectant mother is 1.0-1.40 mmol/l. An increase in its content in the blood is observed with an overdose of vitamin D. Decreased function of the parathyroid glands, renal failure.
The biochemical composition of the blood is examined twice during pregnancy: at the very beginning of pregnancy, when registering the pregnant woman, and at 30 weeks of pregnancy, if not required more often. Blood for biochemical analysis is taken from a vein in the morning on an empty stomach. At least 12 hours must pass since the last meal.
We have provided a list of the necessary, most frequently performed studies, but in each case the set of positions being studied is determined by the doctor. Based on necessity, in each specific case the number of indicators can be reduced or increased.
Nona Hovsepyan, doctor, INVITRO Independent Laboratory
Diagnosis of hepatosis and its signs
Hepatosis in pregnant women is a disease that is sometimes very difficult to diagnose. By this time, the uterus already occupies the entire abdominal cavity, which makes palpation of the liver impossible. This disease is often confused with gallstone disease, because their symptoms are very similar. The most common signs of hepatosis include:
- skin itching;
- yellowing of the skin and whites of the eyes, the appearance of vascular networks on the face and hands, redness of the palms (they seem to be covered with red spots from the inside);
- nausea, vomiting, abdominal discomfort, bitterness in the mouth, stool disorders, loss of appetite;
- pain in the right hypochondrium;
- lightening of stool and darkening of urine (from orange to dark brown);
When the bile duct is disrupted, a large amount of bile accumulates in the liver. Unable to escape, bile begins to break through into the lymphatic system, and from there into the general bloodstream. If you conduct a blood test, it will show an increase in the level of transaminases, alkaline phosphatase, bilirubin and cholesterol, a decrease in hemoglobin, as well as red blood cells and platelets. A urine test will reveal the presence of bile acids and increased secretion of urobilin.
When bile enters the bloodstream, it causes itching, which intensifies in the evening and at night. Most often, pregnant women with this disease consult a doctor with complaints of an acute and irresistible desire to scratch. It drives you crazy, disrupts sleep, leads to fatigue and irritation. As a rule, the arms, legs and stomach itch the most. Filling the liver with bile causes overstretching of its capsule, the surface of which has a large number of pain receptors. This causes constant dull pain in the right side.
If hepatosis is suspected, the doctor at the antenatal clinic should carefully examine the patient, try to palpate the liver area, prescribe extensive blood and urine tests, as well as an ultrasound examination of the liver, gall bladder and neighboring organs.
Painful attacks during hepatosis
In the most difficult cases of hepatosis, the patient sometimes experiences attacks characterized by severe pain in the right hypochondrium. Often the pain is felt in the abdomen, at the level of the navel and is mistaken for an exacerbation of gastritis. Such attacks may be accompanied by continuous and painful vomiting without relief, headache, tinnitus, rapid heartbeat, darkening of the eyes and shortness of breath. They are very similar to severe poisoning syndrome, only in this case the stool practically does not change, and the food eaten is vomited.
Most often, such attacks are caused by eating harmful foods (fried, spicy, fatty, alcohol) and begin 40-60 minutes after eating or by a sudden movement, for example, a quick turn, bend or fall. Painful attacks can last up to 20-40 minutes, they begin suddenly and recede just as sharply. Often after an attack, quite severe residual pain remains in the right hypochondrium for several days. A big mistake during such attacks is taking paracetamol, because it only aggravates the situation, negatively affecting liver activity. It is allowed to take antispasmodic drugs such as No-Shpa.
Take the first step
make an appointment with a doctor!
Delivery with ICP
For ICP, prenatal hospitalization is indicated at 36 weeks. in order to resolve the issue of time and method of delivery, including induction of labor. There is no evidence of the need for early delivery in ICP, but there is a practice of induction of labor in severe forms of cholestasis with severe hyperfermentemia and bile acid concentrations >40 µmol/l [5, 7]. When discussing the issue of delivery, it is necessary to warn about the impossibility of accurately predicting perinatal complications in ICP and the advisability of early delivery in order to reduce the risk of stillbirth. It is also necessary to warn about the risks of intensive care for newborns. Thus, the frequency of hospitalization in the neonatal intensive care unit for early induction of labor at 37 weeks. is 7–11%, at 38 weeks - 6% and at 39 weeks - 1.5%. The decision to deliver should be based not only on laboratory results, but also on other risk factors, since a strong correlation between liver enzyme levels and fetal outcome has not been identified. Making a final decision on the time and method of delivery is possible only after the pregnant woman has been fully informed about the risks to the fetus during induction of labor and the possible deterioration of the fetal condition when pregnancy is prolonged [5].
The danger of hepatosis during pregnancy
The affected liver is not able to cleanse the body of harmful substances, which leads to intoxication of the mother and a deterioration in her well-being. Surprisingly, from the very first day after birth, the disease begins to quickly recede and soon leaves no trace behind. After 1-2 weeks, blood counts return to normal. Even if hepatosis recurs in several pregnancies in a row, it does not make any visible changes in the woman’s liver. However, this does not mean that this disease is harmless. It disrupts the metabolism between mother and fetus, thereby adversely affecting the child. It has been proven that hepatosis increases the likelihood of perinatal mortality by 5%, and in 35% of pregnancies occurring against the background of this disease, hypoxia, prematurity and delay in fetal development were observed.
What causes cholesterol levels to increase?
A healthy woman's body contains approximately 4.138 mmol/L cholesterol. This indicator indicates the normal functioning of organs and systems and the absence of serious health problems. Why does the level of the substance increase? During pregnancy, cholesterol may rise slightly above the permissible norm.
This occurs against the background of the fact that the kidneys and liver begin to work harder due to hormonal changes. The adrenal glands are not able to cope with the elimination of excess and when taking tests, you can see an increase in a fat-like organic compound. During the period of bearing a baby, the normal cholesterol level is considered to be 3.20 - 14 mmol/l.
The organic compound indicator may increase depending on the age category of the pregnant woman. An organic fat-like compound plays an important role for the body of a woman carrying a child. Cholesterol is involved in the formation of the placenta, where the baby grows and develops. Cholesterol takes an active part in the synthesis of hormones.
Very often, the cholesterol level of the expectant mother increases by 1.5-2 times.
If a woman feels well and does not experience any symptoms, then a decreased or increased indicator in this case will not indicate a pathological condition. The amount of cholesterol affects the health of the expectant mother and is responsible for the intrauterine development of the baby.
To lower cholesterol you will need to follow a special diet
Treatment of hepatosis in pregnant women
Treatment of hepatosis is complicated by the fact that almost all medications are contraindicated for pregnant women. Many medications can cause hypoxia and intrauterine growth retardation in the fetus, so the doctor must conduct a full examination of the patient and make sure the diagnosis is correct before deciding on a treatment method. It is very important to understand at what stage the disease is. In the mild stage, you can do without drug intervention by using a special diet. The expectant mother should exclude all heavy, fatty and high-calorie foods from her diet, and also stop taking vitamin complexes and other medications (if their withdrawal does not harm the pregnancy). Drugs designed to optimize liver function are also often prescribed (Hofitol, Essentiale Forte N and others). In many cases, diet is enough to remove toxins from the body and improve the patient's condition.
In more severe stages, the woman is sent to a hospital, where the issue of early delivery is decided. If there is no danger to the fetus, then labor can be delayed by purifying the blood using IVs. They are combined with taking large doses of the above-mentioned drugs and a strict diet. If this technique makes it possible to suppress the disease or at least keep it at the same level of development, and the condition of the fetus does not cause concern, then treatment is continued until 37-38 weeks, and childbirth is planned for this period. If the method does not give the desired result (or if the condition of the fetus worsens, hypoxia is clearly visible), consent to induced labor or Caesarean section is urgently signed. Often the child has a defensive reaction to the unfavorable situation created, and premature birth spontaneously begins. However, you should not rely only on nature. If serious indications arise, it is recommended to start the labor process in advance to minimize the risk of complications.
It is very important that a pregnant woman with severe hepatosis is under constant medical supervision. It is also necessary to carry out extensive blood tests every two days. It often happens that under the influence of IVs, blood counts suddenly drop significantly. Having decided that the disease has subsided, the doctor discharges the patient, and after a couple of days she is again admitted to the hospital with a sharp increase in transaminases.
Take the first step
make an appointment with a doctor!
Why is control needed?
It is important to keep serum cholesterol levels under control. The increase in the level of the compound should be within reasonable limits so as not to provoke the development of complications.
An excessive increase in the fat-like organic compound can cause a decrease in the strength of the expectant mother’s blood vessels and an increase in blood viscosity. As a result, the baby develops heart defects and liver and kidney diseases. Therefore, it is so important to keep cholesterol levels under control and record their dynamics.
You should immediately seek help from your doctor if:
Deciphering a blood test for cholesterol
- a sharp increase in the percentage of fat-like organic compounds by more than 2 times;
- deterioration of health;
- frequent migraines;
- systematic prolonged attacks of nausea in the last months of pregnancy;
- high blood pressure;
- pain in the neck, heart and collarbone.
A specialist will help you find out the reason for the increase in the substance in the blood and take measures to reduce cholesterol. If you ignore unpleasant symptoms, a pregnant woman may experience complications such as the formation of atherosclerotic plaques, the development of varicose veins, difficulties in bearing a child, the risk of premature birth or termination of pregnancy.
The right snack – nuts and sunflower seeds
Prevention of hepatosis in pregnant women
Although hepatosis is considered the result of certain genetic characteristics, there are a number of recommendations to avoid it or delay its appearance for a longer period:
- Dieting. If you have a tendency to overload the liver, then you must completely avoid everything fried, fatty, smoked, salty, spicy and sour. The diet should consist of fruits, vegetables (except potatoes, legumes, onions and garlic), low-fat dairy products, chicken breast meat, and low-fat fish. You should not eat chocolate and other cocoa-containing products, egg yolks, cheese, pastries (1-2 pieces of black bread per day are allowed).
- Physical activity. Movement is life, so you need to move more. This speeds up metabolic processes in the body, eliminates congestion, and facilitates the functioning of the liver.
- Refusal of oral hormonal contraceptives and antibacterial agents. They can cause great harm to the liver.
- Take vitamins carefully or avoid them. If possible, you should try to get all the substances the body needs from food, and not from vitamin complexes.
- Treatment of chronic gastrointestinal diseases.
- The use of hepatoprotectors and choleretic drugs. If pregnancy is not planned yet, then it is enough to carry out preventive courses with these drugs, and if pregnancy has already occurred, then they must be taken according to a special schedule agreed with the attending physician.
Hepatosis in pregnant women is a very insidious disease. If you suspect you have signs of it, be sure to tell your doctor so that he can order a blood test and make or rule out a diagnosis.