Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more deep veins in your body, usually in the legs. Deep vein thrombosis can cause leg pain or swelling, but may be asymptomatic.
- Symptoms of deep vein thrombosis
- Causes of deep vein thrombosis
- Risk factors
- Complications of DVT
- Prevention of thrombosis
DVT may be associated with diseases that affect the blood clotting process. A blood clot in your legs can also form if you have not moved for a long time, such as after surgery or an accident. But walking over extremely long distances can lead to the formation of blood clots.
Deep vein thrombosis is a serious condition because blood clots in your veins can travel through your bloodstream and become lodged in your lungs, blocking blood flow (pulmonary embolism). However, pulmonary embolism can occur without evidence of DVT.
When DVT and pulmonary embolism occur at the same time, it is called venous thromboembolism (VTE).
Symptoms
Signs and symptoms of DVT:
- Swelling of the affected leg. In rare cases, swelling appears in both legs.
- Leg pain. The pain often begins in the calf and may feel like cramping or soreness.
- Red or discolored skin on the leg.
- Feeling of warmth in the affected leg.
Deep vein thrombosis may occur without noticeable symptoms.
When to see a doctor
If you have signs or symptoms of DVT, contact your doctor.
If you develop signs or symptoms of pulmonary embolism (PE), a life-threatening complication of deep vein thrombosis, get emergency medical help.
Call 103
Warning signs and symptoms of pulmonary embolism include:
- Sudden shortness of breath
- Chest pain or discomfort that gets worse with deep breathing or coughing.
- Feeling dizzy or dizzy or faint
- Rapid pulse
- Rapid breathing
- Coughing up blood
Do you suspect deep vein thrombosis? Contact the professionals.
How is thrombophlebitis diagnosed?
A phlebologist is able to determine and prescribe adequate treatment for venous thrombosis of the lower extremities. In especially severe cases, consultation with a vascular surgeon is required. To diagnose this disease, in addition to visual examination and entering data into the patient’s medical record, they can use:
- Duplex ultrasound angioscanning using color Doppler mapping allows you to determine thrombosis localized below the level of the inguinal ligament. Shows the condition of the vessels, features of the movement of blood flow, thanks to which it is possible to determine the places of blockage and parietal thickenings.
- X-ray contrast venography - a contrast agent is injected into the venous system. This method is often used when the previous research is unreliable. Phlebography is especially good at identifying clots in the groin area.
- Magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) - allow you to examine peripheral and central veins. MRI is used to visualize blood clots, and MRA is used to visualize blood vessels.
- Radionuclide scintigraphy is the filling of a vein with a radioactive drug, the movement of which through the deep veins is monitored using a gamma camera. The method allows you to determine the speed and nature of blood flow. This technology is used in extremely difficult cases.
- Plethysmography is a study that is most widespread in Western countries. It is used to measure the degree of blood filling of the venous trunk during physical activity and rest. As a result, it is possible to determine the difference in the electrical resistance of the limb.
The use of laboratory tests is additional. They are not able to give a complete picture of the boundaries of the spread of phlebitis and thrombosis.
Great importance is given to differential diagnosis, which makes it possible to exclude other diseases and pathological conditions that have a similar clinical picture to thrombophlebitis:
- cellulite - subcutaneous fat tissue is affected, mainly in the lower extremities, accompanied by frequent cramps, changes in skin color, and dryness;
- lymphedema - depending on whether the disease is primary or secondary, it affects one or two limbs, is characterized by swelling of the lower leg, pain, fatigue;
- compression of the vessel by neoplasms or inflamed lymph nodes;
- stretching, rupture of muscle tissue - intermuscular hematoma puts pressure on the venous trunks, causing them to narrow;
- rupture of Baker's cyst - diagnosis is carried out using ultrasound.
Risk factors
Many factors can increase your risk of developing DVT, which include:
- Age. At age 60, the risk of DVT increases, although it can happen at any age.
- Sitting for long periods of time, such as while driving or flying. When your legs remain motionless for several hours, your calf muscles do not contract. Muscle contractions promote blood circulation.
- Prolonged bed rest, such as during a long hospital stay or paralysis. Blood clots can form in the calves if the calf muscles are not used for a long time.
- Trauma or surgery. Injury to the veins or surgery may increase the risk of blood clots.
- Pregnancy. Pregnancy increases pressure in the veins of the pelvis and legs. Women with an inherited bleeding disorder are at particular risk. The risk of blood clots from pregnancy can last up to six weeks after the baby is born.
- Birth control pills (oral contraceptives) or hormone replacement therapy. Both factors can increase the blood's ability to clot.
- Exposure to drugs or chemicals. Certain drugs can cause blood clots. Consult your physician before use.
- Overweight or obese. Excess weight increases pressure in the veins of the pelvis and legs.
- Smoking. Smoking affects clotting and circulation, which may increase the risk of DVT.
- Cancer. Some forms of cancer increase levels of substances in the blood that cause blood clotting. Some forms of cancer treatment also increase the risk of blood clots.
- Heart failure. Increases the risk of developing deep vein thrombosis and pulmonary embolism. Because people with heart failure have limited heart and lung function, symptoms caused by even a small pulmonary embolism are more noticeable.
- Inflammatory bowel diseases. Bowel diseases such as Crohn's disease or ulcerative colitis increase the risk of DVT.
- Personal or family history of DVT or PE. If you or someone in your family has had one or both of these, you may be at greater risk of developing DVT.
- Genetics. Some people inherit genetic risk factors or disorders, such as factor V Leiden, that make their blood clot more easily. The hereditary disease itself may not cause blood clots unless it is combined with one or more other risk factors.
- Risk factor unknown. Sometimes a blood clot in a vein can occur without an obvious underlying risk factor. This is called unprovoked VTE.
What is thrombophlebitis
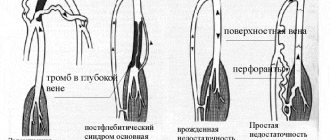
Thrombophlebitis is an inflammatory process of the inner surface of a vein due to the deposits of thrombotic masses on it. They can partially or completely block blood flow. It is worth noting that such a diagnosis will be made if the superficial veins of the lower extremities are affected. If pathology is found in the deep veins, then the diagnosis will be phlebothrombosis.
Thrombophlebitis is a severe pathological condition affecting about 15% of the population, causing damage to the superficial and deep veins. The detachment of part of a blood clot threatens immediate death, submassive pulmonary embolism. In 70% of cases, this disease causes disability. This disease was included in the International Medical Register under code 10, with the designation I80.2, calling it “Phlebitis and thrombophlebitis of the lower extremities.”
Complications
Complications of DVT may include:
- Pulmonary embolism (PE). PE is a potentially life-threatening complication associated with DVT. This occurs when a blood vessel in your lung is blocked by a blood clot that travels to the lung from another part of your body, usually your leg. If you have signs and symptoms of PE, it is important to seek medical help immediately. Sudden shortness of breath, chest pain when inhaling or coughing, rapid breathing, rapid pulse, feeling weak or faint, and coughing up blood may occur with PE.
- Postphlebitic syndrome. Damage to the veins by a blood clot reduces blood flow to the affected areas, causing leg pain and swelling, skin discoloration, and skin ulcers.
- Complications of treatment. Complications may arise from blood thinners used to treat DVT. Bleeding is a side effect of anticoagulants. It is important to have regular blood tests when taking these medications.
Drug treatment
It consists of prescribing anticoagulants, angioprotectors, non-steroidal anti-inflammatory drugs, and certain enzyme preparations. And antibiotics in case of acute purulent thrombophlebitis.
Special ointments are also used: Heparin, Essaven-gel, Ketonal 5% cream, Lyoton-gel and some others. Ointments such as Levomekol, Levosin and others, intended for the treatment of superficial skin lesions and ulcers, only worsen the problem.
Surgery is prescribed when the possible development of pulmonary embolism is suspected after differential diagnosis. Also, the surgical method gets rid of blood clots that have accumulated during acute thrombophlebitis in the bed of the great saphenous vein. The main indication for surgical treatment is signs of movement of part of the clot noticed during ultrasound.
Prevention
Measures to prevent deep vein thrombosis include the following:
- Don't sit still. If you have had surgery or were on bed rest for other reasons, try to get back to work as soon as possible. If you sit for any period of time, do not cross your legs as this can block blood flow. If you are traveling long distances by car, stop every hour or so and take a walk. If you're on an airplane, stand or walk occasionally. If you can't do this, stretch your shins. Do some exercises. Try raising and lowering your heels while keeping your toes on the floor, then lifting your toes while pressing your heels into the floor.
- Do not smoke. Smoking increases the risk of developing DVT.
- Do exercises and control your weight. Obesity is a risk factor for DVT. Regular exercise reduces the risk of blood clots, which is especially important for people who sit a lot or travel frequently.
Treatment with leeches
In acute thrombophlebitis of the lower extremities, leech therapy is practiced. They are dispersed in the direction of the affected vein, up to a maximum of 10 pieces. for 1 time. And not on the vein itself, but at a distance of at least 1 cm from it, staggered. in a checkerboard pattern, if leeches are placed in quantities of up to 10 pieces along the painful vein in a checkerboard pattern at a distance of at least 1 cm from the vein. Up to 60 leeches can be delivered per course.
The use of leeches is not suitable for everyone and not always. Minor reactions are also possible - redness, swelling of the skin, itching. This is an allergy to bites, but it is not serious and will go away on its own fairly quickly. Hyperpigmentation rarely occurs. But in case of individual intolerance, Quincke's edema is possible.
Tests for thrombosis
Laboratory indicators play a significant role in the timely diagnosis of thrombosis.
Thus, guidelines for the management of patients with a new coronavirus infection provide for stratification of the risk of coagulopathy in patients with COVID-19 based on simple laboratory tests: D-dimer, prothrombin time, platelet count, fibrinogen level [1,9]. A clinical blood test can detect inflammation. It also determines the level of platelets, that is, the very substrate of thrombosis.
Additionally, the level of inflammation in the blood and the risk of thrombosis is indicated by an increased level of C-reactive protein.
Biochemical analysis primarily demonstrates blood glucose levels. It can be used to judge the presence of diabetes, one of the most serious risk factors for thrombosis.
Also, a biochemical analysis can determine the level of protein C, which also characterizes the severity of the risk of thrombosis.
Elevated levels of homocysteine in the blood are also a currently proven risk of thrombosis, leading to miscarriage and cardiovascular events (heart attacks and strokes).
D-dimer is a laboratory marker of fibrin formation [8]. It also indicates the presence of inflammation, just like C-reactive protein. The level of D-dimer is a control indicator of COVID-19 and its complications, including those associated with thrombosis.
You can take tests under the comprehensive Thrombosis program, which includes determining the levels of Antithrombin-III, D-dimer and genetic factors of cardiac diseases and platelet levels. This program allows you to determine the fact of thrombosis occurring somewhere in the body, as well as determine the genetic predisposition to it. This program, like other tests, is offered by the CITILAB network of clinics.
Additional determination of homocysteine and C-reactive protein levels will help determine the biochemical risk of thrombosis.
Reasons for development
- Changes in blood composition due to increased viscosity. This happens, for example, with hereditary diseases, oncology, after surgery or serious injuries. Blood viscosity also increases during pregnancy or due to taking medications: hormonal contraceptives, drugs for treating oncology or stopping bleeding.
- Damage to the vessel wall. This happens with injury, burns, serious infection, or after long-term damage to the vascular wall by cholesterol plaques. Radiation or chemotherapy and even the installation of a catheter for administering intravenous drugs also affects.
- Change in blood flow. This can happen with heart rhythm disturbances. Arrhythmias cause turbulence in the blood flow and clots form. Another option is to slow down the blood flow. This happens when there is a lack of movement, for example, after a long flight.
What is the difference between thrombophlebitis and varicose veins?
Thrombophlebitis and varicose veins have similar symptoms, but different nature. With varicose veins, the vessels are constantly dilated, and their walls become thinner. The disease leads to disruption of blood flow and the formation of nodes in the vessels. With thrombophlebitis, the walls of the vein become inflamed and a blood clot forms. Blockage of the lumen of the vessel causes circulatory disorders and swelling of the affected vessel.
Diagnosis of thrombosis
Primary diagnosis is based on a detailed history and anthropometry (calf or thigh circumference).
The Wells scale is used to diagnose acute thrombosis and diagnose pulmonary embolism [8,9]. Instrumental diagnostics include compression or duplex scanning of veins, Doppler ultrasound with compression of veins, impedance plethysmography, pulmonary angiography, radiocontrast or MRI venography [6,9], CT and MRI angiography [7,9].
To diagnose arterial thrombosis, physical tests are used (6-minute walk test, treadmill test), determination of pulsation of superficial arteries (arteries of the dorsum of the foot), duplex scanning of the arteries of the extremities, angiography (X-ray of a vessel filled with a radiopaque substance) and measurement of transcutaneous oxygen tension [ 7].
Thrombosis - treatment with folk remedies
The possibility of treating thrombosis with folk remedies should be discussed with your doctor. Patients with a tendency to form blood clots need to eliminate the causes of leg swelling. Regular physical activity prevents congestion in blood vessels. The most beneficial for varicose veins and venous insufficiency are walking, cycling, and swimming.
Overheating and prolonged exposure to the sun should be avoided. To relieve tension from diseased vessels, you need to raise your legs up so that they are above the level of the heart with support along the entire length of the lower leg.
What is the difference
The pathology differs in the size of the blood clot:
- Occlusive . The thrombus completely covers the venous lumen. The outflow of blood from the lower extremities is completely stopped. This condition leads to necrosis and gangrene.
- Non-occlusive . The venous lumen is partially blocked. The outflow of blood is difficult, but it happens.
There is another type of pathology – floating thrombosis. The thrombus is partially attached to the venous wall and dangles in the lumen of the vessels. This form is no less dangerous than the occlusive one, since a blood clot can break off at any time, block the functioning of the heart or lungs, which will lead to death.
Thrombosis Clinic
Symptoms of thrombosis can be general, regardless of location, or specific.
Common symptoms include pain with movement and at rest, limited mobility, and decreased function of the affected organ or tissue. Symptoms of arterial obstruction (acute thrombosis, or gradual obstruction of vessel patency):
- asymmetry of blood pressure when measured on both arms [7];
- pallor of the skin, turning into cyanosis [7];
- pain at rest at night [7];
- pain when moving in the thigh, buttock, lower leg, foot, shooting or aching [7];
- sleep disorders [7];
- numbness, coldness of the limb [7];
- absence of peripheral pulsation [7];
- necrosis (necrosis) of affected tissues, trophic ulcers, gangrene [7];
- intermittent claudication [7].
Symptoms of venous thrombosis:
- pain [6];
- swelling, soft and asymmetrical [6];
- blue discoloration of the skin (skin cyanosis) [6];
- increased skin temperature of the extremities [6];
- increased sensitivity and compaction in the projection of the superficial veins [2];
- post-inflammatory hyperpigmentation [2];
- dilated saphenous veins [6];
- erythema [2].
Sometimes the only symptom of venous thrombosis is PE [6].