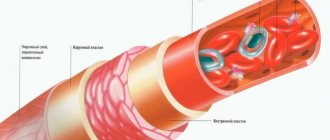
Veins are blood vessels that carry blood to the heart. In turn, blood is collected in the veins from capillaries. With healthy arteries, the circulatory system works stably. But what happens if problems arise with the veins? Swelling, pain in the legs, slight numbness, goosebumps, heaviness, impaired sensitivity in the form of paresthesia, convulsions, trophic disorders. These signs, repeated day after day, are most likely recognized by the doctor as venous insufficiency.
Excess body weight can lead to varicose veins
Chronic venous insufficiency
Chronic venous insufficiency is a common peripheral vascular disease that occurs as a result of impaired blood flow through the veins of the lower extremities and changes in the permeability of the vascular wall. Most often, venous insufficiency develops in women. The disease occurs when the valves that close the veins are unable to prevent blood from flowing back due to increased pressure on them. As a result, this leads to stretching of the walls of the venous vessels. The permeability of the vascular wall for blood and plasma proteins increases, swelling and compaction of adjacent tissues appear. Where small vessels are compressed, areas of ischemia (insufficient blood supply with oxygen) occur, which contributes to the formation of trophic ulcers.
The main risk factors for the development of chronic venous insufficiency include:
- weakness of the muscular wall of the veins (hereditary);
- overweight and obesity;
- pregnancy and childbirth;
- long-term constant work in a standing or sitting position, with limited movement (cooks, office workers, surgeons, etc.);
- chronic constipation;
- fluctuations in hormonal levels in women (contraception with hormonal drugs, hormonal treatment during menopause, etc.);
- wearing tight underwear and clothing, corsets.
The following stages of development of varicose veins are distinguished:
- Stage 0 – no major symptoms upon examination.
- Stage I - “morning fatigue” of the legs, complaints of intermittent swelling in the evenings (disappears in the morning).
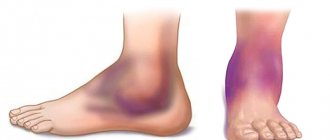
- Stage II – persistent swelling, skin pigmentation disorders; some areas of the skin become thicker, the skin above them cannot be folded (lipodermatosclerosis), redness appears on the skin, accompanied by itching and weeping (eczema).
- Stage III – the formation of trophic ulcers (active or healed), difficult to treat with medication.
The disease is accompanied by pain of varying intensity and the presence of evening cramps. In the treatment of varicose veins in the early stages, compression with elastic bandages and compression hosiery, physiotherapy and therapy in a sanatorium are used.
Introduction
A woman with chronic pain in the lower abdomen is a frequent, complex and, as a rule, conflict-prone patient encountered by doctors of many specialties. The causes of chronic pelvic pain in women are numerous, and one of the leading places among them is varicose veins of the small pelvis (PVV). The disease occurs in women of all ages and has a progressive course. It should be especially noted that ARVMT is an interdisciplinary problem, since patients often go in circles from a gynecologist to a surgeon, a gastroenterologist, a neurologist, and again to a gynecologist. Thus, doctors of many specialties may encounter the problem of treating ARVMT.
There are two main directions in the treatment of ARVMT. The first of them is represented by surgical methods, among which are ligation of the pelvic veins, their endovascular embolization and sclerosis. It should be noted that surgical methods are effective only for varicose veins of the ovary and have a number of disadvantages - primarily, invasiveness and frequent recurrence [1, 2, 4, 5].
The second direction is conservative methods, in which angioprotectors and microcirculation correctors are widely used. Among the phleboprotective agents in this group, the most effective are drugs based on diosmin, which include Detralex. The advantages of Detralex are good bioavailability, which is ensured by the micronized formula of the drug [6, 7], the absence of contraindications and the possibility of use in all biological periods of a woman’s life - adolescence, reproductive, pregnancy (from the second trimester), pre- and postmenopause [3].
The purpose of the presented study was to study the effectiveness of Detralex in the treatment of ARVMT in women during the main biological periods of life.
Material and methods
The study included 301 patients with URVT. The patients were divided into 4 main groups and 4 comparison groups. The main groups included 50 teenage girls, 30 women of reproductive age, 57 in the postpartum period and 35 in pre- and postmenopause. The comparison groups included, respectively, 50 teenage girls, 20 women of reproductive age, 34 in the postpartum period and 25 in pre- and postmenopause. All women included in the study in the postpartum period were delivered by cesarean section for obstetric indications.
Patients from the main groups received Detralex at a dose of 1000 mg/day (1 tablet 2 times a day) for 2 months. Patients from the comparison groups received placebo.
The effectiveness of Detralex was studied clinically and instrumental methods. The pelvic venous system was examined in all women. Using ultrasound (ultrasound), the diameter of the main venous collectors of the small pelvis was determined: uterine, internal iliac, ovarian and arcuate veins. Adolescents, women of reproductive age, and pre- and postmenopausal women underwent Doppler ultrasound to study peak systolic blood flow velocity (Vps) in the uterine veins. In patients of reproductive age, microcirculation in the pelvic organs was assessed using radioisotope clearance.
Statistical processing of data was carried out using the Statistica 6.0 program. The normality of the distribution of sample means was checked using the Kolmogorov–Smirnov test. In the case of a normal distribution of means, the hypothesis of their equality was tested using the t-test. In other cases, the Mann–Whitney test was used.
Research results
The leading clinical symptom of ARVMT in women is pain in the lower abdomen, which has varying irradiation and intensity. And if girls are characterized by an asymptomatic course of ARVMT, then with age the frequency of pain increases, and the peak of the pain syndrome occurs during the reproductive period. Detralex relieved pain in women in all biological periods of life, and most effectively during reproductive age. In patients receiving placebo, the frequency of pain did not change significantly (Fig. 1).
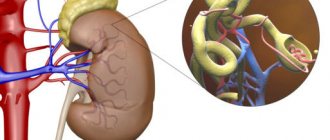
It is known that ARVMT in women is characterized by an increase in the diameter of the main venous collectors of the small pelvis, so studying the effect of Detralex on the tone of the pelvic veins is of particular interest (Fig. 2).
The results of ultrasound before and after treatment with Detralex show that a course of taking the drug leads to a significant decrease in the diameter of the uterine, internal iliac, ovarian and arcuate veins in all main groups of patients (Table 1).
Dilatation of the venous wall during URVMT leads to chronic venous congestion in the pelvic organs, which is manifested by a significant decrease in Vps in the uterine veins, detected by Doppler examination (Fig. 3).
Detralex improved the drainage function of the pelvic venous system, which was manifested by an increase in Vps in the uterine veins in patients of three main groups (Table 2), determined using Doppler sonography. Reducing the diameter of the pelvic veins and eliminating chronic venous stagnation is the result of the multifactorial action of Detralex. This has a venotonic effect, normalization of the drainage function of the pelvic venous system, and improvement of microcirculation. While taking Detralex, microcirculation indicators, determined in women of reproductive age using radioisotope clearance, significantly improve (Table 3): the time for establishing equilibrium of radioactivity over the common iliac veins is reduced, the angle of elevation of radioactivity over the iliac veins is increased, and the time for establishing general equilibrium is reduced.
Conclusion
ARVMT is a chronic relapsing disease that cannot be completely cured at the present stage of medical development. The main goals of treatment are to slow down the progression of ARVMT, prevent its relapses and improve the quality of life of patients. Detralex, the therapeutic effect of which is aimed at the main links in the pathogenesis of ARVMT - dilatation of veins, reduction in the speed of venous blood flow and microcirculation in the pelvic organs, allows you to successfully solve this problem. The undoubted advantage of Detralex is its effectiveness in all biological periods of a woman’s life, which makes it possible to prevent ARVMT at puberty, during pregnancy and childbirth, as well as during menopause. It is important to emphasize that treatment of ARVMT in women should not be limited to taking Detralex only, as it must be comprehensive.
Composition and therapeutic effect of the drug Detralex
A therapeutic course of venotonic drugs is also prescribed. Detralex is used most often.
It is based on flavonoids - substances of plant origin. The active ingredients are hesperidin and diosmin, which eliminate venostasis (blood stagnation).
Detralex restores and increases the tone of venous walls and blood microcirculation in small vessels. Capillaries become elastic and plastic, their permeability decreases. The medicine reduces the distensibility of the veins, which reduces the release of plasma and proteins from the bloodstream into the surrounding tissues.
Detralex has an angioprotective and venotonic effect.
In addition, the drug Detralex increases the outflow of lymph, thereby providing lymphatic drainage.
Medicine Detralex
Detralex is produced by the French company Servier, whose production complex is located, among other things, in Russia.
The main principle of the company producing Detralex is environmental friendliness, naturalness and safety. Therefore, all Servier products are a guarantee of high quality. Detralex is no exception. THIS IS INTERESTING: one of the components of Detralex - hesperidin - is extracted from the peel of unripe oranges. Moreover, the choice of unripe fruits is approached with special care - their size should not exceed 2.5 cm in diameter. Because the smaller the fruit, the more valuable substances it contains. The main countries for orange production are Mexico, Egypt, China and Morocco. First, the orange peels are dried and crushed. This is how the basis for Detralex is obtained - a complex of flavonoids or a flavonoid fraction, which is then sent for refinement and production of the drug we are familiar with.
Indications
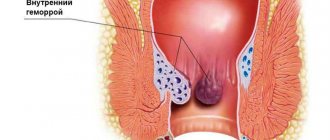
Indications for the use of the drug Detralex are organic and functional venous-lymphatic insufficiency of the lower extremities. Detralex is also used for the symptomatic treatment of acute hemorrhoidal attacks.
The medicine Detralex can be used for tired legs
Detralex is indicated for:
- pain;
- cramps of the lower extremities;
- feeling of heaviness and fullness in the legs;
- "fatigue" in the legs.
- swelling of the lower extremities;
- trophic changes in the skin and subcutaneous tissue;
- venous trophic ulcers.
Side effects
When taking the drug Detralex, in rare cases, the following adverse reactions may develop:
- from the gastrointestinal tract: dyspepsia, diarrhea, nausea, vomiting, colitis;
- from the central nervous system: headache, dizziness, general malaise;
- from the skin: urticaria, itching, rash, isolated swelling of the face, eyelids, lips, angioedema.
If any side effects occur, you should consult your doctor and adjust your treatment.
Note!
The description of the drug Detralex on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use.
Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug). Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.
How to take Detralex?
Detralex is used as a symptomatic remedy for varicose veins and hemorrhoids. Often, the attending physician prescribes therapy that includes venotonic ointments or gels. When treating hemorrhoids, rectal suppositories and ointments can be used to relieve pain and inflammation, improve vascular tone, reduce blood clots and stop bleeding.
Before taking the medicine, you must carefully read the instructions
Detralex tablets are intended for oral use. Depending on the indications and general condition of the patient, the daily dose of the drug and the duration of the course of therapy are determined by the doctor.
- Venous-lymphatic insufficiency: 2 tablets/day (1 tablet in the middle of the day and 1 tablet in the evening with meals).
- Chronic hemorrhoids: 2 tablets/day (1 tablet in the middle of the day and 1 tablet in the evening with meals). After 7 days, you can change the dosage regimen of Detralex and use the drug 2 tablets once, with meals.
- Acute hemorrhoids: 6 tablets/day (2-3 tablets at equal intervals) for 4 days, then 4 tablets/day (2 tablets in the morning and 2 tablets in the evening) for the next 3 days.
The duration of treatment with Detralex depends on the severity of the disease, the patient’s medical history and, on average, is about 2-3 months. As prescribed by a doctor, the therapeutic course can be repeated.
Please note that taking Detralex for acute hemorrhoids does not replace specific therapy. That is why it is necessary to contact a specialist who will prescribe a therapeutic course, including drug treatment.
Tips for taking the drug
For people with impaired venous circulation, to increase the effectiveness of the drug, it is recommended:
- avoid standing for long periods of time and prolonged exposure to the sun;
- adjust body weight and diet;
- wear compression stockings to improve blood circulation;
- hike.
As for drinking alcohol during treatment with Detralex, there is no direct prohibition. You just need to consider the effects of alcoholic beverages on the cardiovascular system. Thus, alcohol increases blood pressure and dilates blood vessels, in turn, a sharp blood flow provokes stagnation. That is, alcohol reduces the effectiveness of treatment.
Varicose veins of the pelvis
Basic concepts:
- Pelvic varicose veins (PVD) is a disease characterized by dilation of the ovarian veins and intrapelvic venous plexuses.
- Vulvar varicose veins (VV) are dilation of the veins of the external genitalia.
- Chronic pelvic pain (CPP) is non-cyclic pain lasting more than 6 months, localized in the pelvis, reducing the patient’s quality of life and requiring medical or surgical treatment.
Predisposing factors:
- Genetic predisposition;
- Pregnancy and childbirth;
- Aorto-mesenteric compression of the left renal vein;
- May-Turner syndrome;
- Postthrombotic disease, chronic occlusion of the iliac veins, inferior vena cava;
- Venous dysplasia;
Anatomical nomenclature
Anatomical terminology Terminology of the International Union of Phlebologists:
- Deep veins
- Inferior vena cava
- Common iliac vein
- Internal iliac vein
- External iliac vein
- Pelvic veins: gonadal, broad ligament, others
Classification and formulation of diagnosis
However, the most common classification is the following:
- according to clinical manifestations:
- pelvic venous congestion syndrome;
- varicose veins of the external genitalia (vulvar varicose veins).
- with the flow:
- painful form;
- painless form;
- latent form.
- according to the prevalence of pelvic vein lesions:
- isolated expansion of the pelvic venous plexuses;
- combined dilation of the gonadal veins and pelvic venous plexuses;
- unilateral or bilateral dilation of the gonadal veins;
- dilatation of the trunk or tributaries of the internal iliac veins.
Diagnosis of varicose veins of the pelvis
The objectives of diagnostic actions when examining patients with suspected VVVT are:
- Establishing the fact of the presence of VDVT;
- Establishment of the obvious etiological factor in the development of VDVT;
- Determining the treatment strategy: is it necessary to use surgical methods to correct the disease or should we limit ourselves to conservative methods;
- Determination of treatment tactics: what treatment technique (or combination thereof) should be used;
- Objective assessment of the effectiveness of therapeutic actions.
Methods for diagnosing varicose veins of the pelvis, which allow solving the assigned problems are:
- clinical examination (examination, palpation, collection of complaints, medical history);
- ultrasound scanning of the pelvic veins;
- pelvic vein scintigraphy (emission computed tomography);
- multislice computed tomography of the pelvic veins;
- selective ovariography and pelvic venography.
Clinical examination
In the classic version, VVVT is manifested by a triad of symptoms - pelvic pain, vulvar varicose veins, dysmenorrhea. Often the disease is accompanied by other signs, their various combinations, which are often found in other diseases, but have features characteristic of VTB. The following should be considered complaints (subjective signs) relatively specific to VVVT:
- Chronic pelvic pain (CPP) is the most striking symptom of the disease. Its features are the intensification/occurrence of pain during static (prolonged sitting, standing) and physical activity, in the second (luteal) phase of the menstrual cycle, against the background of the use of hormonal drugs containing gestagens. A decrease in pain occurs after the patient rests in a horizontal position with her legs elevated, after using venoactive drugs. The pain is a constant dull aching character, localized in the iliac regions, often on the left, and can radiate to the perineum and thighs. For an objective assessment of CPP, it is advisable to use a visual analogue school of pain.
- Heaviness and discomfort in the hypogastric region with the above orthostatic loads
- Dyspareunia is pain that occurs during or after sexual intercourse. A feature of this symptom is the persistence of pain from 30 minutes to a day after sexual intercourse.
- Dysuric disorders are manifested by a frequent urge to urinate. Mesaortic compression syndrome of the left renal vein is accompanied by micro- and macrohematuria.
- Dysmenorrhea is a disturbance in the rhythm and duration of menstruation. Characterized by the presence of prolonged, heavy and irregular uterine bleeding
- Infertility, probably caused by involution of the uterus and ovaries against the background of long-term venous congestion of the pelvic organs
- Psycho-emotional disorders (unstable mood, irritability, insomnia, masked depression).
Objective signs of varicose veins of the pelvis are:
- Vulvar varicose veins
- Pain on palpation of the hypogastric region, left or right iliac regions.
Instrumental examination
Ultrasound scanning of the pelvic veins is necessary for all patients with suspected VPVT. The study should be performed in 2 modifications: transabdominal (examine the inferior vena cava, renal and iliac veins, the renal segment of the left gonadal vein) and transvaginally (examine the veins of the uterus, parametrium, ovarian segment of the gonadal veins). The method is used as a screening diagnostic; its purpose is to confirm or exclude the existence of varicose transformation of the gonadal veins and pelvic venous plexuses.
Ultrasonographic signs of the disease are dilation of the gonadal veins (more than 5 mm) with the presence of pathological reflux of blood through them, varicose veins of the pampiniform, uterine plexuses, veins of the parametrium (diameter more than 4 mm), detection of retrograde blood flow through these vessels. Mesaortic compression of the left renal vein during ultrasound examination is manifested by a decrease in the diameter of the vessel in the renocaval anastomosis and prestenotic dilatation of the left renal vein.
The protocol for ultrasound examination of the pelvic veins for VPVT or its relapse should indicate:
- Patency and diameter of gonadal veins
- Patency and diameter of the veins of the pelvic plexuses (cliniform, parametrium, arcuate)
- Patency and diameters of the inferior vena cava, renal and iliac veins
Possibilities of ultrasound angioscanning. The study is a reliable way to detect varicose transformation of the gonadal veins and intrapelvic venous plexuses, register pathological blood reflux through these vessels, and assess the condition of the left renal vein.
Multislice computed tomography of the pelvic veins is indicated for patients with a diagnosis of VPVT verified by ultrasound and radionuclide methods, and for patients with recurrent pelvic pain after surgery on the gonadal veins. X-ray signs of VVVT are contrasting dilated gonadal veins and pelvic venous plexuses in sagittal, frontal and axial projections.
Possibilities of multislice computed tomography. The method makes it possible to accurately determine the anatomical and topographical features of the pelvic veins, the diameter of the gonadal veins and pelvic venous plexuses, the number of tributaries of the ovarian veins and their exact location, and to identify concomitant pathology of the pelvic organs and kidneys. The advantages of the method in comparison with ovariography are the immediate assessment of the condition of the arteries and veins of the pelvis, renal and mesenteric vessels, the short duration of the study (no more than 5 minutes), less invasiveness and radiation exposure to the patient and the doctor, and the ability to perform the study on an outpatient basis.
Selective ovariography and pelvic venography. The method should be used in patients who are planning surgery on the gonadal veins, as well as in patients with recurrent CPP in the postoperative period. This study cannot be replaced by any other in case of suspected/detected mesaortic compression of the left renal vein, because Only during ovariography is it possible to determine the pressure gradient between the inferior vena cava and the left renal vein, the excess of which is more than 5 mmHg. serves as an indication for reconstructive surgery on the renal vein or shunt surgery.
Phlebographic signs of VVVT are:
- dilatation of gonadal veins more than 5 mm
- reflux of contrast agent into the left and/or right ovarian vein with contrasting of the pampiniform and uterine venous plexuses
- deposition of contrast in the veins of the parametrium and uterus and its flow to the opposite side.
Pelvic vein scintigraphy (emission computed tomography) should be used in patients with an ultrasound-confirmed diagnosis of VPVT. The main purpose of using pelvic vein scintigraphy is to determine the degree of pelvic venous congestion (PVP), calculated using a computer program. The dynamics of the TVP coefficient can be used to objectively assess the effectiveness of surgical or conservative treatment of VVVT.
Detralex during pregnancy and lactation
Detralex is not recommended for pregnant women
The use of Detralex by pregnant women and children during breastfeeding is not recommended due to insufficient research and clinical data. There is no information on the occurrence of side effects in pregnant women, nor has there been any information recorded on the ability of the active ingredients - diosmin and hesperidin - to pass into breast milk during breastfeeding, as well as in children during breastfeeding.
Analogues of the drug Detralex
For problems with veins and varicose veins, it is possible to use Detralex analogues. They can have a similar therapeutic effect, but have their own contraindications, dosages and possible side effects. Be sure to consult a specialist!
So the pharmaceutical market offers us the following analogues of Detralex:
Venozol
The main active ingredients, like Detralex, are diosmin and hesperidin. Pharmacological action is similar to Detralex. Release form: tablets, gel and cream.
Vasocket
The active substance (diosmin) reduces the distensibility and increases the tone of the veins, thereby preventing the appearance of edema. Available in tablet form.
Antistax
Bioflavonoid drug belongs to the group of venotonic drugs. Available in tablet form.
Troxevasin
Produced under the trade names Venoruton, Troxerutin. Improves the condition of the walls of blood vessels and has an anti-edematous effect. Main forms of release: capsules, gel for topical use, solution for injection in ampoules.
Analogues of the drug Detralex
Anavenol
Combined venoprotective drug. Available in tablet form. Side effects: bleeding, dizziness, nausea. Contraindicated for children under 15 years of age.
Venoruton
Angioprotective drug. The active ingredient is hydroxyethylrutoside. Release form: tablets and gel for external use. Possible use in the second and third trimesters of pregnancy.
Ginkor fort
Venotonic and venoprotective drug It contains a standardized extract of ginkgo biloba, heptaminol hydrochloride and troxerutin. Available in the form of capsules and gel for external use. In case of overdose, blood pressure may increase. According to indications, the drug can be prescribed in the second and third trimesters of pregnancy. Contraindicated in hyperthyroidism and concomitant use of MAO inhibitors.
Detralex or Venarus?
Venarus is a generic drug. That is, it is based on the same active ingredients (diosmin and hesperidin), but the original drug (Detralex) always contains components of a higher degree of purification. Therefore, its effectiveness is higher and its tolerability is better. In addition, Venarus is characterized by lower bioavailability and more often provokes adverse reactions in the body. The drug is also contraindicated during lactation. The pharmacological action is similar to the drug Detralex. There is no fundamental difference between them. Recommendations for taking medications for varicose veins and hemorrhoids are identical.
Detralex or Phlebodia?
The active ingredient of the drug Phlebodia 600 is diosmin. But its concentration in Detralex is 450 mg/tablet (plus its enhancing hesperidin 50 mg/tablet), and Phlebodia 600 is available in the form of tablets with a diosmin concentration of 600 mg/tablet.
The medicine has a therapeutic effect similar to Detralex. It also increases the tone of the venous wall, improves blood flow, and normalizes the permeability of vascular walls.
Nevertheless, Detralex is absorbed into the body faster than its analogue, and its concentration in the blood plasma reaches its maximum after three to four hours.