Right atrium hypertrophy is an expansion, thickening of the myocardial wall at the level of this chamber. At the initial stages it does not manifest itself in any way, except for rare exceptions. Further, the symptoms are represented not only by cardiac, but also by respiratory signs. The clinical picture is bright, the patient’s quality of life drops significantly.
Without competent, timely assistance, there is a high probability of death from cardiac arrest or pulmonary edema. Therapy is conservative or surgical, if the root cause is eliminated. Depends on the diagnosis.
In most cases, the process has a closed, paradoxical character: hypertrophy is provoked by problems with the bronchopulmonary system and aggravates them in the future.
In extremely rare cases, it can be a variant of the physiological conditional norm (in athletes).
Development mechanism
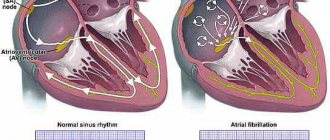
Enlargement of the right atrium is the result of an increase in pressure in the pulmonary artery, other vessels of the small circle, as well as overload of the chamber with blood as a result of the influence of one or another factor.
Detection plays a diagnostic role, because hypertrophy has several types.
An increase in pressure in the pulmonary and other arteries develops as a result of hemodynamic disturbances, vascular defects, and hypertension.
The normal outflow of blood from the right atrium weakens, the remains of liquid connective tissue press on the walls, provoking adaptive mechanisms.
The load on the atrium increases, the organ grows. Builds muscle mass to improve contractility and prevent tissue tearing.
Another mechanism is associated with dysfunction of the tricuspid valve. It covers the passage between the right atrium and the ventricle.
Malfunction leads to incomplete ejection of blood, increased pressure in the chambers and their hypertrophy for the same reasons.
Based on the origin of the process, the mechanism of formation, three forms are distinguished:
- Cardiosclerotic variety. It occurs as a result of inflammation, heart attack and other phenomena of the same kind (coronary insufficiency, coronary artery disease). The affected area becomes scarred, cells are roughly arranged around the area, and tissue grows artificially. Hence the increase in volume, disruption of normal activity.
- Compensatory type. It develops as a result of the influence of a negative factor: an increase in pressure in the pulmonary artery, pulmonary vessels, and other processes.
- Working variety. It develops in patients who are professionally involved in sports. Less likely to engage in similar physical activity as part of work (loaders, others).
Determining the mechanism plays an important role in diagnosis. This is the basis for prescribing competent therapy.
Causes
Factors may be cardiac or non-cardiac. Some lead to the development of the defect faster. Others for a long period (from 3 years and more).
Sample list:
Arterial hypertension
Represents a stable increase in pressure. The result of a combination of a group of moments that lead to a change in the tonometer readings.
As it progresses, blood pressure levels stabilize at high levels, and increased atrial output is noted. The tension on the walls of the chambers increases, the first blow falls on the right structure. Hence the thickening and the beginning of a compensatory mechanism.
At the 3rd stage of hypertension, it is no longer possible to radically help. There is a high risk of developing resistance to therapy, in which case the rate will decrease slightly or not completely.
The load is still there. Therefore, regular hospitalizations are indicated to correct the treatment regimen. Otherwise, there is a high risk of death within 5-10 years from diagnosis. Perhaps less.
Change in body weight towards increase
Obesity is not recognized by everyone as a disease. This is a pathological process, but it is not to blame for hypertrophy.
An enlarged right atrium is the result of ongoing atherosclerosis, blockage of the lumen primarily of the pulmonary and coronary arteries with cholesterol deposits - plaques.
Hence the increase in pressure, overstrain of the chambers, ischemia of myocardial tissue and the dual mechanism of development of the disorder.
Metabolic conditions are treated with statins. Treatment is prescribed in the early stages, before generalized cellular disorders begin.
Long-term stress
Accompanied by the release of corticosteroids and catecholamines. Cortisol and adrenaline as the main ones. They cause constriction of blood vessels, including coronary ones. An increase in blood pressure, then cardiac dysfunction occurs.
Recovery is very difficult. Psychotherapeutic assistance, mastering relaxation methods, changing professional activities, and other activities are indicated. Depends on the case.
The body cannot exist in this state for a long time.
Congenital and acquired vascular malformations
An example is stenosis of the pulmonary artery or aortic valve.
It ends with a disturbance in the movement of blood in the small (pulmonary) circle and an increase in pressure in the vessels. The stress on the chamber walls also increases.
Such processes are difficult to correct. Medicines only treat the symptoms, while the root cause remains untouched.
Tricuspid valve defects
The tricuspid structure bridges the gap between the right atrium and the ventricle. If there is a malfunction, an incomplete release of blood into the next chamber occurs, or its reverse flow occurs - regurgitation.
Some of the liquid connective tissue remains in the atrium and presses on the walls. Thickening occurs as a compensatory mechanism.
On the one hand, this prevents rupture, on the other hand, it allows blood to be pumped more actively. Read more about tricuspid regurgitation in this article.
Treatment is prescribed immediately after detection. Advanced or dangerous cases are corrected surgically. The operation significantly increases the chances of survival and health.
Previous heart attack
Necrosis of cardiac tissues, myocardium. It is accompanied by severe symptoms, so it is difficult to confuse the pathological process with others. Requires urgent hospitalization and first aid.
Even in case of success, which is recognized as saving the patient’s life, coronary disease is observed. It imposes a lot of restrictions on everyday and professional conditions.
Constant treatment under the supervision of a cardiologist is also required. Protectors, antiarrhythmics, antihypertensives and others are used.
The cause of right atrium hypertrophy is tissue scarring and rough epithelization of damaged areas.
Angina pectoris
A variant of coronary insufficiency on a par with a heart attack. A process that is so dangerous gives a chance for a cure and time for diagnosis.
It occurs in fits and starts. Each such episode leads to the death of a small part of the muscle layer, necrosis. Further, just as during a heart attack, the dead tissue is replaced by thick, scar tissue.
Read more about the symptoms of an angina attack and methods of treating it here.
Pneumonia or pneumonia
Septic lesion of the parenchyma. Accompanied by long-term disturbances in gas exchange and an increase in pressure in the small circle.
Damage to cardiac structures is possible, especially with a long-term or chronic process.
Treatment in a hospital, with elimination of signs of respiratory failure, antimicrobial therapy and restoration of heart activity.
Bronchial asthma
Most cases are of the allergic variety. It cannot be completely cured because it is immune in nature. There are chances to achieve a stable long-term remission.
A long course is accompanied by the process getting out of control, an increase in the phenomena of respiratory failure and disruption of normal gas exchange, and an increase in pressure in the small circle.
The result is hypertrophy not only of the atrium, but also of the right ventricle (pulmonary heart).
Systematic use of glucocorticoids and bronchodilators is required (with caution, the latter wash out potassium and impair myocardial contractility).
Chronic obstructive pulmonary disease
The scourge of smokers and workers of hazardous industrial enterprises.
The violations are irreversible. You shouldn't expect a total cure. It is also not easy to transfer the pathological process into remission. Long periods of therapy with powerful hormone-based drugs are required. Quitting smoking will no longer help.
Extended sports activities
Lead to artificial growth of the chambers of the heart. This is the result of excessive physical activity, a response to the need to normalize blood flow.
The organic defect is associated with bradycardia (decreased heart rate) and a drop in blood pressure. This is part of the overall clinical picture.
“The heart of an athlete” is considered a variant of the physiological norm, but individuals with this type of professional activity must be carefully monitored.
Thickening of the right atrium is not the only change. The remaining chambers are also expanding.
Inflammation of the myocardium, pericardial sac
Infectious or autoimmune. They lead to consequences similar to those of a heart attack.
The causes of RA hypertrophy are the result of cardiac and bronchopulmonary pathologies.
Arrhythmogenic right ventricular dysplasia
Terminology
Arrhythmogenic right ventricular dysplasia (ARVD) is a relatively rare cardiac disease, regarding which many questions and conflicting ideas remain to this day.
The first clinical description belongs to the outstanding Italian thinker, doctor, anatomist Giovanni Maria Lancisi (all other transcriptions of the Italian surname Lancisi, namely “Lancisi”, “Lancisi”, etc., are incorrect). He also wrote avant-garde works for that time (XVII-XVIII centuries) on the neuro-brain organization, on malaria, on the connection between syphilis and vascular aneurysms, and on epizootics in cattle. The date of writing the cardiological study “De Motu Cordis et Aneurysmatibus”, where J.-M. Lancisi described in detail ARVD as a hereditary disease in four generations of one family, domestic sources call it either 1736 or 1745, without any reservations regarding the fact that Lancisi himself died in 1720. In fact, the publication was posthumous and was published in 1728.
All this may seem unimportant, but there are other ambiguities regarding arrhythmogenic pancreatic dysplasia. The modern formulation of the diagnosis of ARVD was proposed only in 1977, but already five years later (1982) the synonymous diagnosis “arrhythmogenic right ventricular cardiomyopathy” came into use, which is used, in particular, in ICD-10 (heading “Other heart diseases / Cardiomyopathies” ). The disease is usually called hereditary, but often in the same text it is reported that the genetic factor is traced in less than half of the cases. Epidemiological data are incomplete and inaccurate; arrhythmogenic pancreatic cardiomyopathy is classified as a rare disease, but it is the second most common cause of sudden cardiac death at a young age.
The essence of this pathology is that the parenchymal (functional, specialized) tissue of the right cardiac ventricle is gradually replaced by fatty and connective tissue; this steato-fibrous process is usually localized in the “triangle of dysplasia”, the vertices of which are the apex of the heart, the inlet and outlet valves of the ventricle. Statistical estimates of occurrence in the general population vary very widely, with a range of two orders of magnitude: from 0.01% to almost 1% (the latter applies to the Mediterranean region, where ARVD is recorded much more often). Men predominate among those affected - again, some authors limit themselves to this statement, others talk about a threefold predominance. Only one case out of five is diagnosed over the age of 40, the remaining 4/5 occur in children and young people. Sudden cardiac death in 25-26% of people under 20 years of age is caused by arrhythmogenic cardiomyopathy of the pancreas. Similar statistics (25%) are observed in athletes who suddenly died. In total, in the age group under 40 years, ARVD as a direct cause of cardiovascular mortality is detected in 20% of cases. However, it should be emphasized that all these data were obtained from small samples; Of course, they need clarification, and the disease itself needs intensive further research (which is currently being carried out), since until recent decades the clinical and medical-social relevance of this problem, apparently, was seriously underestimated.
Symptoms
Signs of the process depend on the degree and severity of the disorder. In the early stages, the following points arise:
- A slight burning sensation in the chest, possibly tingling. The pain is weak, not pronounced. Duration is minimal. Treated with Nitroglycerin.
- Cough. Intense, non-productive, no sputum. It intensifies at night and may be accompanied by hemoptysis.
- Paleness of the skin. Mucous membranes.
- Cyanosis of the nasolabial triangle. Blue discoloration of the area around the mouth.
- Dyspnea. First associated with intense physical activity. Deviations can only be detected by athletes; a person without daily training does not reach the threshold when the symptom manifests itself. Then at rest. The manifestation accompanies the patient on an ongoing basis and is not controlled by bronchodilators.
- Excessive fatigue without physical activity. Weakness, drowsiness, apathy. Decreased ability to work.
Similar symptoms are observed at a later time, but are aggravated and supplemented by a number of signs.
Among the alarming points:
- Hemoptysis. It has nothing to do with tuberculosis, but differential diagnosis is necessary. At the very least, an X-ray, or better yet a computed tomography scan to differentiate.
- Swelling of the lower extremities. At first only the feet are affected, then the ankles. Next, the process covers the entire leg or both at once.
- Enlarged liver. Painful sensations in the right hypochondrium; palpation reveals an organ protruding beyond the edge. In the absence of treatment, the phenomena of the inflammatory, destructive process increase. Possible accumulation of fluid in the abdominal cavity or ascites, jaundice, and other phenomena.
- Swelling of the cervical vessels. Indicates an increase in venous pressure. This is a consequence of blood stagnation.
- Heart rhythm disturbances. According to the type of bradycardia, ventricular fibrillation. Subjectively it is felt as freezing in the chest, interruptions, heaviness and other moments
- Headache. In the occipital region. Top of the head.
- Vertigo. To the point of being unable to stand on your feet.
- Nausea. Extremely rarely - vomiting. Signs of neurological deficit.
Fainting is possible. Indicate circulatory disorders in cerebral structures. Evaluation in the system.
Heart defects
Rubella
Cold
Stroke
Atherosclerosis
Diabetes
5074 19 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Heart defects: causes, symptoms, diagnosis and treatment methods.
Definition
Heart disease is defined as an atypical or abnormal structure of its structures (chambers, valves, large vessels), which is a consequence of disturbances in the formation and development (congenital heart disease) or various pathological changes (acquired heart disease). As a result of the formation of this pathology, the functioning of the heart is disrupted and oxygen deficiency of organs and tissues of the body is formed, which can ultimately lead to heart failure.
Causes of heart defects
In humans, the blood returning to the heart from all organs and tissues (oxygen-poor blood) passes through the right atrium and then through the right ventricle into the pulmonary artery, and from there it enters the lungs. In the lungs, the blood is enriched with oxygen, releases carbon dioxide and enters the left atrium and left ventricle, and from there it is pumped to all organs and tissues through the aorta, and then through smaller arteries. The performance of the heart muscle depends on the functioning of the valves, which, when contracting, freely allow blood to flow into the next section, and when relaxing, do not allow blood to flow back.
If the function of the valves is impaired, the function of the heart is also impaired.
Congenital heart defects are very diverse. More than one and a half hundred different variants of atypical heart structure have been described. About one in 100 babies is born with a heart defect. Common heart pathologies diagnosed in infancy and childhood are atrial and ventricular septal defects (the openings between the chambers of the heart). Often the defects are combined with anomalies of the valvular apparatus of the heart or large vessels. The most common congenital heart defect is the bicuspid aortic valve, which opens with every heartbeat, allowing blood to flow from the heart to all organs. A normal aortic valve has three leaflets.
Bicuspid aortic valve does not usually cause problems during infancy or childhood, so it is often not diagnosed until adulthood.
The causes of congenital heart defects include genetic, environmental and infectious. In addition, their formation can be caused by certain diseases (gestational diabetes mellitus, rubella and systemic lupus erythematosus) in the mother, taking certain medications, drugs and alcohol during pregnancy, and other factors.
Acquired defects are anomalies and defects of the heart valves, its openings or partitions between the chambers, and the vessels extending from it, which appeared during life under the influence of morphological and functional changes in the functioning of the heart. The mitral valve is affected more often than the aortic valve. Pathologies of the tricuspid (tricuspid) valve and pulmonary valve are less common. Diseases can manifest at any age under the influence of atherosclerosis, cardiosclerosis, ischemic or hypertension, rheumatism, systemic pathology, trauma, syphilis and some other reasons. Also, degenerative changes in the valves lead to valvular heart defects - as the disease develops, their structure and function are disrupted, which causes a restructuring of hemodynamics, overload of the corresponding parts of the heart occurs, hypertrophy of the heart muscle, and impaired circulation in the heart and in the body as a whole.
Classification of the disease
It is customary to highlight:
- defects of the “white” type, when there is no tendency to mix arterial and venous blood;
- “blue” type defects - venous blood enters the arterial bed, resulting in oxygen deficiency.
Type of functional pathology:
- stenosis - as a result of the pathological process, deformation of the valve tissue occurs and the hole through which blood flows to the next part of the heart narrows;
- valve insufficiency - failure of the heart valves to close due to changes in shape, their shortening as a result of scarring of the affected tissues;
- combined and concomitant heart defects:
- combined – in the presence of both stenosis and insufficiency of one valve;
- combined – when several valves are affected at once.
Based on the reasons for their formation, acquired defects are classified as follows:
- degenerative, or atherosclerotic (occur in 5-6% of cases) - more often these processes develop after 40-50 years, when calcium is deposited on the leaflets of the affected valves, which leads to the progression of the defect;
- rheumatic, developing against the background of rheumatic diseases (80% of cases);
- defects that arise as a result of inflammation of the inner lining of the heart (endocarditis);
- syphilitic (in 5% of cases).
Based on the general hemodynamic condition, compensated, subcompensated and decompensated heart defects are distinguished.
Symptoms of heart defects
Clinical symptoms of heart defects include shortness of breath, weakness, fatigue, swelling of the lower extremities, sleep disturbances, interruptions in heart function, arrhythmia (usually tachycardia), change in skin color (blueness or pallor), swelling of the veins of the neck and head, causeless anxiety, pressing pain in the heart area (especially during physical activity) or between the shoulder blades, in rare cases - loss of consciousness.
Specific symptoms of congenital heart defects depend on the patient's age. Because normal circulation of oxygen-rich blood is essential for normal growth and development, infants may experience difficulty or rapid breathing, poor appetite, sweating or increased breathing during feeding, cyanosis of the lips and/or skin, unusual irritability, or failure to gain weight. .
Children and adolescents may experience decreased exercise tolerance, dizziness, and fainting.
Most serious heart defects in children are identified based on symptoms noticed by parents and abnormalities found when examined by a doctor. Impaired blood flow through the heart usually manifests as a heart murmur that can be heard with a stethoscope. Abnormal heart murmurs are often loud or harsh. However, in the vast majority of cases, heart murmurs noted in childhood are functional and not caused by heart defects.
The severity and nature of symptoms depend on the location of the affected valve. With valve defects of the left half of the heart (mitral and aortic), the lungs are primarily affected, since blood stagnates in their vessels, which is manifested by shortness of breath and cough. In addition, there are signs of insufficient blood supply to the brain and the heart itself, dizziness, fainting, and angina. In the presence of cyanosis, one of the most common pathologies is tetralogy of Fallot (restriction of blood flow to the lungs).
When the valves of the right half of the heart (the tricuspid and pulmonary valves) malfunction, blood stagnates in the vessels of the systemic circulation, so all organs except the lungs suffer. Swelling of the legs and feet, ascites (accumulation of fluid in the abdominal cavity), enlarged liver, and other lags in weight gain develop.
Signs of acquired defects are often combined with other heart diseases, in particular coronary artery disease, which makes their clinical differentiation difficult.
Diagnosis of heart defects
Diagnostic measures carried out to detect heart defects require an integrated approach, but always begin with collecting an anamnesis: the doctor finds out the patient’s complaints, the time and circumstances of their manifestation, intensity, and hereditary factors. Next, a physical examination is carried out, which includes visual inspection, palpation, percussion (tapping), auscultation (listening).
Laboratory tests that are prescribed for suspected heart disease:
- clinical blood test;
Diagnostics
It takes place on an outpatient basis. In most cases, there is time for a quality examination; the main thing is to contact before the development of threatening phenomena.
Approximate list of events:
- Oral questioning of the patient, collection of anamnestic data.
- Auscultation. Listening to heart sounds. Noises of various types are noted. But not always.
- Measurement of blood pressure, contraction frequency. Both indicators may be normal or abnormal. Based on the nature of the disorder, one or another probable diagnosis is indicated.
- Daily monitoring. Record vital signs within 24 hours. Used to assess the state over time.
- Electrocardiography. Detection of functional disorders of the muscular organ.
- Echocardiography. Visualization technique. Used to determine defects, their location and severity.
- MRI or CT scan of the chest as needed.
- Assessment of neurological status.
- Ultrasound of the liver and abdominal organs.
General blood test, biochemical, also not hormones (if endocrine disorders are suspected).
Main features of a normal ECG in children
This article presents modern views on ECG diagnostics in pediatrics. The team of authors examined some of the most characteristic changes that distinguish the ECG in childhood.
A normal ECG in children differs from the ECG in adults and has a number of specific features in each age period. The most pronounced differences are observed in young children, and after 12 years, the child’s ECG approaches the cardiogram of an adult.
Features of heart rhythm in children
Childhood is characterized by a high heart rate (HR); newborns have the highest heart rate; as the child grows, it decreases. Children exhibit pronounced lability of heart rate; permissible fluctuations are 15–20% of the average age value. Sinus respiratory arrhythmia is often noted; the degree of sinus arrhythmia can be determined using Table 1.
The main pacemaker is the sinus node, however, acceptable variants of the age norm include the mid-atrial rhythm, as well as migration of the pacemaker through the atria.
Features of the duration of ECG intervals in childhood
Considering that children have a higher heart rate than adults, the duration of ECG intervals, waves and complexes decreases.
Changing the voltage of the QRS complex waves
The amplitude of the ECG waves depends on the individual characteristics of the child: tissue electrical conductivity, chest thickness, heart size, etc. In the first 5–10 days of life, a low voltage of the QRS complex waves is noted, which indicates reduced electrical activity of the myocardium. Subsequently, the amplitude of these waves increases. From infancy to 8 years, a higher amplitude of the waves is detected, especially in the chest leads, this is due to the smaller thickness of the chest, the larger size of the heart relative to the chest and the rotation of the heart around its axes, as well as a greater degree of fit of the heart to the chest. Features of the position of the electrical axis of the heart
In newborns and children in the first months of life, there is a significant deviation of the electrical axis of the heart (EOS) to the right (from 90 to 180°, on average 150°). From the age of 3 months. By the age of 1 year, in most children, the EOS moves to a vertical position (75–90°), but significant fluctuations in the angle are still allowed (from 30 to 120°). By 2 years, 2/3 of children still maintain the vertical position of the EOS, and 1/3 have a normal position (30–70°). In preschoolers and schoolchildren, as well as in adults, the normal position of the EOS predominates, but variants in the form of a vertical (more often) and horizontal (less often) position may be noted.
Such features of the position of the EOS in children are associated with changes in the ratio of masses and electrical activity of the right and left ventricles of the heart, as well as with changes in the position of the heart in the chest (rotations around its axes). In children in the first months of life, anatomical and electrophysiological predominance of the right ventricle is noted. With age, as the mass of the left ventricle increases rapidly and the heart rotates with a decrease in the degree of adhesion of the right ventricle to the surface of the chest, the position of the EOS moves from the right to the normogram. The changes that are occurring can be judged by the changing ratio of the amplitude of the R and S waves in the standard and chest leads on the ECG, as well as by the displacement of the transition zone. Thus, as children grow in standard leads, the amplitude of the R wave in lead I increases, and in lead III it decreases; the amplitude of the S wave, on the contrary, decreases in lead I and increases in lead III. In the chest leads, with age, the amplitude of the R waves in the left chest leads (V4-V6) increases and decreases in leads V1, V2; the depth of the S waves increases in the right chest leads and decreases in the left ones; The transition zone gradually shifts from V5 in newborns to V3, V2 after the 1st year. All this, as well as an increase in the interval of internal deviation in lead V6, reflects the increasing electrical activity of the left ventricle and rotation of the heart around its axes with age.
In newborn children, large differences are revealed: the electrical axes of the P and T vectors are located practically in the same sector as in adults, but with a slight shift to the right: the direction of the P vector is on average 55°, the T vector is on average 70°, while the QRS vector is sharply deviated to the right (on average 150°). The value of the adjacent angle between the electrical axes P and QRS, T and QRS reaches a maximum of 80–100°. This partly explains the differences in the size and direction of the P waves, and especially the T waves, as well as the QRS complex in newborns.
With age, the value of the adjacent angle between the electrical axes of the P and QRS, T and QRS vectors decreases significantly: in the first 3 months. life on average up to 40–50°, in young children – up to 30°, and in preschool age it reaches 10–30°, as in schoolchildren and adults (Fig. 1).
In adults and school-age children, the position of the electrical axes of the total vectors of the atria (vector P) and ventricular repolarization (vector T) relative to the ventricular vector (vector QRS) is in the same sector from 0 to 90°, and the direction of the electrical axis of the vectors P (on average 45 –50°) and T (on average 30–40°) does not differ sharply from the orientation of the EOS (QRS vector on average 60–70°). An adjacent angle of only 10–30° is formed between the electrical axes of the P and QRS, T and QRS vectors. This position of the listed vectors explains the same (positive) direction of the P and T waves with the R wave in most leads on the ECG. Features of teeth intervals and complexes of children's ECG
Atrial complex (P wave). In children, as in adults, the P wave is small (0.5–2.5 mm), with maximum amplitude in standard leads I and II. In most leads it is positive (I, II, aVF, V2-V6), in lead aVR it is always negative, in leads III, aVL, V1 it can be smoothed, biphasic or negative. In children, a slightly negative P wave in lead V2 is also allowed.
The greatest features of the P wave are observed in newborns, which is explained by increased electrical activity of the atria due to the conditions of intrauterine circulation and its postnatal restructuring. In newborns, the P wave in standard leads, compared to the size of the R wave, is relatively high (but in amplitude no more than 2.5 mm), pointed, and sometimes may have a small notch at the apex as a result of non-simultaneous coverage of the right and left atria by excitation (but not more than 0 .02–0.03 s). As the child grows, the amplitude of the P wave decreases slightly. With age, the ratio of the size of the P and R waves in standard leads also changes. In newborns it is 1: 3, 1: 4; as the amplitude of the R wave increases and the amplitude of the P wave decreases, this ratio by 1–2 years decreases to 1: 6, and after 2 years it becomes the same as in adults: 1: 8; 1: 10. The smaller the child, the shorter the duration of the P wave. It increases on average from 0.05 s in newborns to 0.09 s in older children and adults.
Features of the PQ interval in children. The duration of the PQ interval depends on heart rate and age. As children grow, there is a noticeable increase in the duration of the PQ interval: on average from 0.10 s (no more than 0.13 s) in newborns to 0.14 s (no more than 0.18 s) in adolescents and 0.16 s in adults (no more than 0.20 s).
Features of the QRS complex in children. In children, the time of ventricular excitation coverage (QRS interval) increases with age: on average from 0.045 s in newborns to 0.07–0.08 s in older children and adults.
In children, as in adults, the Q wave is recorded inconsistently, more often in II, III, aVF, left chest leads (V4-V6), less often in I and aVL leads. In lead aVR, a deep and wide Q wave of the Qr type or QS complex is detected. In the right chest leads, Q waves, as a rule, are not recorded. In young children, the Q wave in standard leads I and II is often absent or weakly expressed, and in children of the first 3 months. – also in V5, V6. Thus, the frequency of registration of the Q wave in various leads increases with the age of the child.
In standard lead III in all age groups, the Q wave is also small on average (2 mm), but can be deep and reach up to 5 mm in newborns and infants; in early and preschool age - up to 7–9 mm and only in schoolchildren it begins to decrease, reaching a maximum of 5 mm. Sometimes, in healthy adults, a deep Q wave is recorded in standard lead III (up to 4–7 mm). In all age groups of children, the size of the Q wave in this lead can exceed 1/4 of the size of the R wave.
In lead aVR, the Q wave has a maximum depth, which increases with the age of the child: from 1.5–2 mm in newborns to 5 mm on average (with a maximum of 7–8 mm) in infants and at an early age, up to 7 mm on average (with a maximum of 11 mm) in preschool children and up to 8 mm on average (with a maximum of 14 mm) in schoolchildren. The duration of the Q wave should not exceed 0.02–0.03 s.
In children, as well as in adults, R waves are usually recorded in all leads, only in aVR they can be small or absent (sometimes in lead V1). There are significant fluctuations in the amplitude of the R waves in different leads from 1–2 to 15 mm, but the maximum value of the R waves in standard leads is up to 20 mm, and in the chest leads up to 25 mm. The smallest magnitude of R waves is observed in newborns, especially in the strengthened unipolar and chest leads. However, even in newborns, the amplitude of the R wave in standard lead III is quite large, since the electrical axis of the heart is deviated to the right. After 1 month the amplitude of the RIII wave decreases, the size of the R waves in the remaining leads gradually increases, especially noticeably in the II and I standard and in the left (V4-V6) chest leads, reaching a maximum at school age.
In the normal position of the EOS, high R waves with a maximum of RII are recorded in all limb leads (except aVR). In the chest leads, the amplitude of the R waves increases from left to right from V1 (r wave) to V4 with a maximum of RV4, then decreases slightly, but the R waves in the left chest leads are higher than in the right ones. Normally, in lead V1, the R wave may be absent, and then a QS-type complex is recorded. In children, the QS type complex is also rarely allowed in leads V2, V3.
In newborns, electrical alternans is allowed - fluctuations in the height of the R waves in the same lead. Variants of the age norm also include respiratory alternation of ECG waves.
In children, deformation of the QRS complex in the form of the letters “M” or “W” in the III standard and V1 leads is often found in all age groups, starting from the neonatal period. In this case, the duration of the QRS complex does not exceed the age norm. Splitting of the QRS complex in healthy children in V1 is referred to as “slow excitation syndrome of the right supraventricular crest” or “incomplete block of the right bundle branch.” The origin of this phenomenon is associated with the excitation of the hypertrophied right “supraventricular scallop” located in the region of the conus pulmonary of the right ventricle, which is the last to be excited. The position of the heart in the chest and the electrical activity of the right and left ventricles changing with age are also important.
The internal deviation interval (time of activation of the right and left ventricles) in children changes as follows. The activation time of the left ventricle (V6) increases from 0.025 s in newborns to 0.045 s in schoolchildren, reflecting an accelerated increase in the mass of the left ventricle. The activation time of the right ventricle (V1) remains virtually unchanged with the child’s age, amounting to 0.02–0.03 s.
In young children, a change in the localization of the transition zone occurs due to a change in the position of the heart in the chest and a change in the electrical activity of the right and left ventricles. In newborns, the transition zone is located in lead V5, which characterizes the dominance of the electrical activity of the right ventricle. At the age of 1 month. the transition zone shifts to leads V3, V4, and after 1 year it is localized in the same place as in older children and adults - in V3 with fluctuations V2-V4. Together with an increase in the amplitude of the R waves and deepening of the S waves in the corresponding leads and an increase in the activation time of the left ventricle, this reflects an increase in the electrical activity of the left ventricle.
Both in adults and in children, the amplitude of the S waves in different leads varies widely: from absence in a few leads to a maximum of 15–16 mm, depending on the position of the EOS. The amplitude of the S waves changes with the age of the child. Newborn children have the smallest depth of S waves in all leads (from 0 to 3 mm), except standard I, where the S wave is quite deep (on average 7 mm, maximum up to 13 mm).
In children older than 1 month. the depth of the S wave in the first standard lead decreases and subsequently in all leads from the limbs (except aVR) S waves of small amplitude (from 0 to 4 mm) are recorded, just like in adults. In healthy children, in leads I, II, III, aVL and aVF, the R waves are usually larger than the S waves. As the child grows, there is a deepening of the S waves in the chest leads V1-V4 and in lead aVR, reaching a maximum value at high school age. In the left chest leads V5-V6, on the contrary, the amplitude of the S waves decreases, often they are not recorded at all. In the chest leads, the depth of the S waves decreases from left to right from V1 to V4, having the greatest depth in leads V1 and V2.
Sometimes in healthy children with an asthenic physique, with the so-called. “hanging heart”, S-type ECG is recorded. In this case, the S waves in all standard (SI, SII, SIII) and chest leads are equal to or exceed the R waves with reduced amplitude. It is believed that this is due to the rotation of the heart around the transverse axis with the apex posteriorly and around the longitudinal axis with the right ventricle forward. In this case, it is almost impossible to determine the angle α, so it is not determined. If the S waves are shallow and there is no shift of the transition zone to the left, then we can assume that this is a normal variant; more often, the S-type ECG is determined by pathology.
The ST segment in children, as well as in adults, should be on the isoline. The ST segment may shift up and down up to 1 mm in the limb leads and up to 1.5–2 mm in the chest leads, especially in the right ones. These shifts do not mean pathology if there are no other changes on the ECG. In newborns, the ST segment is often not expressed and the S wave, when reaching the isoline, immediately turns into a gently rising T wave.
In older children, as in adults, the T waves are positive in most leads (standard I, II, aVF, V4-V6). In standard III and aVL leads, T waves can be smoothed, biphasic or negative; in the right chest leads (V1-V3) are often negative or smoothed; in lead aVR – always negative.
The greatest differences in T waves are observed in newborns. In their standard leads, the T waves are low-amplitude (from 0.5 to 1.5–2 mm) or smoothed. In a number of leads, where T waves in children of other age groups and adults are normally positive, in newborns they are negative, and vice versa. Thus, in newborns there may be negative T waves in standard I, II, in strengthened unipolar and in the left chest leads; may be positive in standard III and right chest leads. By 2–4 weeks. life, an inversion of T waves occurs, i.e. in the I, II standard, aVF and left chest leads (except V4) they become positive, in the right chest and V4 - negative, in the III standard and aVL they can be smoothed, biphasic or negative.
In subsequent years, negative T waves persist in lead V4 until 5–11 years, in lead V3 – up to 10–15 years, in lead V2 – up to 12–16 years, although in leads V1 and V2 negative T waves are allowed in some cases and in healthy adults.
After 1 month During life, the amplitude of T waves gradually increases, amounting in young children from 1 to 5 mm in standard leads and from 1 to 8 mm in chest leads. In schoolchildren, the size of T waves reaches the level of adults and ranges from 1 to 7 mm in standard leads and from 1 to 12–15 mm in chest leads. The T wave is largest in lead V4, sometimes in V3, and in leads V5, V6 its amplitude decreases.
The QT interval (ventricular electrical systole) makes it possible to assess the functional state of the myocardium. The following features of electrical systole in children can be identified, reflecting the electrophysiological properties of the myocardium changing with age.
The duration of the QT interval increases as the child grows from 0.24–0.27 s in newborns to 0.33–0.4 s in older children and adults. With age, the relationship between the duration of electrical systole and the duration of the cardiac cycle changes, which is reflected by the systolic index (SP). In newborn children, the duration of electrical systole occupies more than half (SP = 55–60%) of the duration of the cardiac cycle, and in older children and adults – 1/3 or slightly more (37–44%), i.e., with age, SP decreases.
With age, the ratio of the duration of the electrical systole phases changes: the excitation phase (from the beginning of the Q wave to the beginning of the T wave) and the recovery phase, i.e., rapid repolarization (duration of the T wave). In newborns, more time is spent on recovery processes in the myocardium than on the excitation phase. In young children, these phases take approximately the same time. In 2/3 of preschoolers and most schoolchildren, as well as in adults, more time is spent on the arousal phase.
Features of ECG in different age periods of childhood
Newborn period (Fig. 2).
1. In the first 7–10 days of life, there is a tendency towards tachycardia (heart rate 100–120 beats/min), followed by an increase in heart rate to 120–160 beats/min. Pronounced heart rate lability with large individual fluctuations. 2. A decrease in the voltage of the QRS complex waves in the first 5–10 days of life with a subsequent increase in their amplitude. 3. Deviation of the electrical axis of the heart to the right (angle α 90–170°). 4. The P wave is relatively larger (2.5–3 mm) in comparison with the teeth of the QRS complex (P/R ratio 1: 3, 1: 4), often pointed. 5. PQ interval does not exceed 0.13 s. 6. The Q wave is unstable, as a rule, absent in standard I and in the right chest leads (V1-V3), it can be deep up to 5 mm in standard III and aVF leads. 7. The R wave in standard lead I is low, and in standard lead III it is high, with RIII > RII > RI, high R waves in aVF and right precordial leads. The S wave is deep in standard I, II, aVL and in the left precordial leads. The above reflects the deviation of the EOS to the right. 8. Low amplitude or smoothness of T waves in the limb leads is noted. In the first 7–14 days, the T waves are positive in the right chest leads, and in the I and left chest leads they are negative. By 2–4 weeks. life, an inversion of the T waves occurs, i.e. in the I standard and left pectorals they become positive, and in the right pectorals and V4 they become negative, remaining so in the future until school age.
Infant age: 1 month. – 1 year (Fig. 3).
1. Heart rate decreases slightly (on average 120–130 beats/min) while maintaining rhythm lability. 2. The voltage of the QRS complex teeth increases, often higher than in older children and adults, due to the smaller thickness of the chest. 3. In most infants, the EOS goes into a vertical position, some children have a normogram, but significant fluctuations in the α angle are still allowed (from 30 to 120°). 4. The P wave is clearly expressed in standard leads I and II, and the ratio of the amplitude of the P and R waves decreases to 1:6 due to an increase in the height of the R wave. 5. The duration of the PQ interval does not exceed 0.13 s. 6. The Q wave is recorded inconsistently and is often absent in the right precordial leads. Its depth increases in standard III and aVF leads (up to 7 mm). 7. The amplitude of the R waves in standard I, II and in the left thoracic (V4-V6) leads increases, and in standard III it decreases. The depth of the S waves decreases in standard I and in the left chest leads and increases in the right chest leads (V1-V3). However, in VI, the amplitude of the R wave, as a rule, still prevails over the magnitude of the S wave. The listed changes reflect the shift of the EOS from the correct position to the vertical position. 8. The amplitude of the T waves increases, and by the end of the 1st year the ratio of the T and R waves is 1: 3, 1: 4.
ECG in young children: 1–3 years (Fig. 4).
1. Heart rate decreases to an average of 110–120 beats/min, and in some children sinus arrhythmia appears. 2. The high voltage of the QRS complex teeth remains. 3. EOS position: 2/3 of children maintain a vertical position, and 1/3 have a normogram. 4. The ratio of the amplitude of the P and R waves in standard leads I and II decreases to 1: 6, 1: 8 due to the growth of the R wave, and after 2 years it becomes the same as in adults (1: 8, 1: 10) . 5. The duration of the PQ interval does not exceed 0.14 s. 6. Q waves are often shallow, but in some leads, especially in standard III, their depth becomes even greater (up to 9 mm) than in children of the 1st year of life. 7. The same changes in the amplitude and ratio of the R and S waves that were noted in infants continue, but they are more pronounced. 8. There is a further increase in the amplitude of the T waves, and their ratio with the R wave in leads I and II reaches 1: 3 or 1: 4, as in older children and adults. 9. Negative T waves remain (options: biphasic, smooth) in standard III and right chest leads up to V4, which is often accompanied by a downward shift of the ST segment (up to 2 mm).
ECG in preschool children: 3–6 years (Fig. 5).
1. Heart rate decreases to an average of 100 beats/min, and moderate or severe sinus arrhythmia is often recorded. 2. The high voltage of the QRS complex teeth remains. 3. EOS is normal or vertical, and very rarely there is a deviation to the right and a horizontal position. 4. PQ duration does not exceed 0.15 s. 5. Q waves in various leads are recorded more often than in previous age groups. The depth of the Q waves in standard III and aVF leads remains relatively large (up to 7–9 mm) compared to that in older children and adults. 6. The ratio of the size of the R and S waves in standard leads changes towards an even greater increase in the R wave in standard leads I and II and a decrease in the depth of the S wave. 7. The height of the R waves in the right chest leads decreases, and in the left chest leads it increases. The depth of the S waves decreases from left to right from V1 to V5 (V6). ECG in schoolchildren: 7–15 years (Fig. 6).
The ECG of schoolchildren is close to the ECG of adults, but there are still some differences:
1. Heart rate decreases on average in younger schoolchildren to 85–90 beats/min, in older schoolchildren – to 70–80 beats/min, but heart rate fluctuations within wide limits are noted. Moderate and severe sinus arrhythmia is often recorded. 2. The voltage of the QRS complex teeth decreases somewhat, approaching that of adults. 3. Position of the EOS: more often (50%) – normal, less often (30%) – vertical, rarely (10%) – horizontal. 4. The duration of ECG intervals approaches that of adults. The PQ duration does not exceed 0.17–0.18 s. 5. The characteristics of the P and T waves are the same as in adults. Negative T waves persist in lead V4 up to 5–11 years, in V3 – up to 10–15 years, in V2 – up to 12–16 years, although negative T waves in leads V1 and V2 are also allowed in healthy adults. 6. The Q wave is recorded inconsistently, but more often than in young children. Its value becomes smaller than in preschool children, but in lead III it can be deep (up to 5–7 mm). 7. The amplitude and ratio of the R and S waves in various leads approach those in adults. Conclusion
To summarize, we can highlight the following features of the children's electrocardiogram: 1. Sinus tachycardia, from 120–160 beats/min during the newborn period to 70–90 beats/min by high school age. 2. Greater variability of heart rate, often sinus (respiratory) arrhythmia, respiratory electrical alteration of QRS complexes. 3. The norm is considered to be mid- and lower-atrial rhythm and migration of the pacemaker through the atria. 4. Low QRS voltage in the first 5–10 days of life (low electrical activity of the myocardium), then an increase in the amplitude of the waves, especially in the chest leads (due to the thin chest wall and the large volume occupied by the heart in the chest). 5. Deviation of the EOS to the right up to 90–170º during the newborn period, by the age of 1–3 years – transition of the EOS to a vertical position, by adolescence in about 50% of cases – normal EOS. 6. Short duration of intervals and waves of the PQRST complex with a gradual increase with age to normal limits. 7. “Syndrome of delayed excitation of the right supraventricular crest” – splitting and deformation of the ventricular complex in the form of the letter “M” without increasing its duration in leads III, V1. 8. Pointed high (up to 3 mm) P wave in children in the first months of life (due to the high functional activity of the right side of the heart in the prenatal period). 9. Often – deep (amplitude up to 7–9 mm, more than 1/4 of the R wave) Q wave in leads III, aVF in children up to adolescence. 10. Low amplitude of T waves in newborns, increasing by the 2nd–3rd year of life. 11. Negative, biphasic or smoothed T waves in leads V1-V4, persisting until the age of 10–15 years. 12. Shift of the transition zone of the chest leads to the right (in newborns - in V5, in children after the 1st year of life - in V3-V4) (Fig. 2–6).
Bibliography
: 1. Heart disease: A guide for doctors / ed. R.G. Oganova, I.G. Fomina. M.: Litterra, 2006. 1328 p. 2. Zadionchenko V.S., Shekhyan G.G., Shchikota A.M., Yalymov A.A. Practical guide to electrocardiography. M.: Anaharsis, 2013. 257 pp.: ill. 3. Isakov I.I., Kushakovsky M.S., Zhuravleva N.B. Clinical electrocardiography. L.: Medicine, 1984. 4. Kushakovsky M.S. Cardiac arrhythmias. St. Petersburg: Hippocrates, 1992. 5. Orlov V.N. Guide to electrocardiography. M.: Medical Information Agency, 1999. 528 p. 6. Guide to electrocardiography / ed. h. Doctor of Science RF, prof. V.S. Zadionchenko. Saarbrucken, Germany. Lap Lambert Academic Publishing GmbH&Co. KG, 2011. P. 323. 7. Fazekas T.; Liszkai G.; Rudas LV Electrocardiographic Osborn wave in hypothermia // Orv. Hetil. 2000. Oct. 22.Vol. 141(43). P. 2347–2351. 8. Yan GX, Lankipalli RS, Burke JF et al. Ventricular repolarization components on the electrocardiogram: Cellular basis and clinical significance // J. Am. Coll. Cardiol. 2003. No. 42. P. 401–409.
Signs on ECG
{banner_banstat9}
- A characteristic sign on the cardiogram is deformation of the atrial P wave (pointed, in the normal state it is round, without notches) and its widening.
- Change in contraction frequency. First towards tachycardia, in the later stages the heart rate drops to 60 and below.
The assessment is carried out by a diagnostician, then again by a cardiologist at the appointment.
Hypertrophy of the right atrium on the ECG is manifested by an increase and sharpening of the P-wave. The remaining points play a secondary role and allow us to assess the very nature of the accompanying violations.
Treatment
{banner_banstat10}
Carried out under the supervision of a cardiologist. In the early stages, if there are no catastrophic defects yet, dynamic monitoring is indicated. Every 3-6 months, cardiography and ECHO-CG, also changes in pressure, heart rate.
Deterioration and progression are grounds for urgent prescription of medications. According to indications, surgical treatment of pathology is used.
List of medications for symptomatic and etiotropic, cardiac action:
- Cardioprotectors. Normalize metabolism in cells.
- Antiarrhythmic. With extrasystole, fibrillation, paroxysmal tachycardia.
- Beta blockers. To correct blood pressure levels and relieve sinus arrhythmia.
- Cardiac glycosides. Stabilize myocardial contractility. But they are used in small courses, with caution. They are not prescribed after a heart attack.
- Diuretics. To remove excess fluid and reduce the load on the heart.
- Hepatoprotectors. To prevent damage to liver cells.
Other names are indicated for non-cardiac causes.
Surgery is a last resort. Prescribed for vascular defects, the heart itself and valves. Tumors, aneurysms, etc.
Attention:
You cannot resort to traditional methods; at best they are useless, then they are not worth the time and money spent, at worst they are dangerous.
As part of rehabilitation and further treatment, smoking and alcohol cessation is indicated. Normalization of the diet (table No. 10).
The working or physiological variety does not require therapy at all. The patient must be constantly monitored. Cardioprotectors are used if necessary.
Progression of pathology is associated with poor outcome. Only organ transplantation can help.
Cardiac hypertrophy
Cardiac hypertrophy
Cardiac hypertrophy is an enlargement of the heart muscle, which occurs mainly due to an increase in the number of cardiomyocytes - specialized muscle cells of the heart. This condition occurs in children, adolescents, young adults and the elderly.
Cardiac hypertrophy is a manifestation of a special state of the body: physiological or pathological. That is, it is not a disease, but a symptom.
Physiological
Physiological hypertrophy of the heart is observed in athletes and people who lead an active lifestyle. For regular physical activity, the body requires large amounts of oxygen. Oxygen is delivered through the blood. And to meet the increased oxygen needs, the heart increases the frequency and strength of contractions. And this requires greater metabolism in the heart muscle itself. This gradually increases the volume and mass of cells (cardiomyocytes). More often in athletes, cardiac hypertrophy begins from the left ventricle. Sports that can lead to cardiac hypertrophy are rowing, hockey, football, cross-country skiing, cycling, long-distance running, etc. When you stop training, this condition reverses. That is, the hypertrophied heart again becomes of normal size with normal wall thickness.
Pathological
Pathological hypertrophy of the heart occurs due to various diseases of the body. The human heart consists of four sections: two atria and two ventricles. The atria are reservoirs where blood enters from the body's circulation (blue vessels). The ventricles are a buoyant force that pushes blood through the vessels (red vessels). So each department has its own reasons for increasing.
Causes:
- Left ventricle – enlarges due to arterial hypertension, aortic valve stenosis, aortic atherosclerosis, general obesity, diabetes mellitus
- Right ventricle – due to congestive heart failure, chronic pulmonary failure
- Left atrium – with arterial hypertension, general obesity, aortic and mitral valve defects
- Right atrium - due to pulmonary diseases (when there is stagnation in the pulmonary circulation).
Development
The above reasons force us to maintain normal blood flow by increasing the mass of the heart. It must be taken into account that an increase in one part of the heart leads to hypertrophy of another. In addition to cardiomyocytes, the heart also contains connective tissue. With cardiac hypertrophy, it also grows, and this leads to a decrease in the elasticity of the walls and disruption of the heart.
If the load on the heart does not decrease, then the myocardium is gradually depleted because the blood flow cannot cope with the nutrition of the enlarged heart. This can lead to disruption of nerve impulses (arrhythmia), sclerosis and atrophy of the heart muscle.
Symptoms
- An asymptomatic course of cardiac hypertrophy is possible.
- If the left half of the heart is affected: pain in the heart area (increases after physical activity), arrhythmia, loss of consciousness, shortness of breath, dizziness.
- If the right half of the heart is affected: cough, shortness of breath, cyanosis (cyanosis) or pallor of the skin, swelling, arrhythmia.
Diagnostics
- Ultrasound examination of the heart
- ECG (electrocardiography)
- X-ray of the chest organs.
Treatment It is necessary to eliminate the cause of cardiac hypertrophy.
If it is arterial hypertension, it is necessary to take antihypertensive and diuretic drugs. Severe heart valve defects require surgical treatment and prosthetics. Respiratory diseases require anti-inflammatory and bronchodilator therapy. In any case, the approach is always individual. To monitor blood pressure and early detect arrhythmia, I recommend using automatic tonometers from the manufacturer Microlife, presented in our online store.
The author of the article is a practicing neurologist Maxim Nikolaevich Starshinin.
Forecast
Depends on the underlying pathological process. Early forms provide 100% survival rate. The way of daily living is almost unaffected, the patient can continue the same activities with minor restrictions.
When defects are added, progression is many times faster. Death occurs in 30% of cases.
Arterial hypertension, increased pulmonary pressure and other incurable pathologies do not guarantee early death. Depends on the start of supervision.
The possibility of radical intervention is characterized by a sharp improvement in prognosis.
Questions about the likely outcome should be directed to the leading physician. Therefore, it is recommended to contact the same cardiologist. He will take into account all factors and give an approximate answer.