Therapist
Berezhko
Olga Igorevna
35 years of experience
General practitioner of the highest category, member of the Russian Scientific Medical Society of Therapists
Make an appointment
Vasculitis is a group of vascular diseases that are characterized by the development of an inflammatory process and subsequent necrosis of the vascular walls. The disease is also called arteritis or angiitis. As the disease progresses, a significant deterioration in blood circulation occurs. Pathology can affect arteries, veins, capillaries, venules and arterioles.
Types and classification of vasculitis
Vasculitis is divided into types:
- primary;
- secondary;
- systemic.
In the first case, we are talking about an independent and still just beginning disease. The second type may appear with other pathologies, for example, tumors. It can also occur as a reaction to an infection. Systemic vasculitis can occur in different ways. It leads to inflammation of blood vessels and damage to their walls, and tissue necrosis cannot be ruled out. Without proper treatment, complications usually occur, including death.
Based on the caliber of the affected vessels, a classification of vasculitis was identified. It may be in the form:
- arteritis (affects large vessels);
- phlebitis (affects the walls of the veins);
- arteriolitis (inflames the arteries and arterioles);
- capillaritis (affects capillaries).
Also included in a separate category is vasculopathy, which is characterized by the absence of clear signs of inflammation and infiltration of the vascular walls.
The degree of vascular damage can be mild, moderate and severe.
Main primary vasculitis:
- Takayasu arteritis (synonyms: “nonspecific aortoarteritis”,
- "aortic arch syndrome")
- giant cell arteritis (synonyms: “temporal arteritis”,
- "senile arteritis", "Horton's disease")
- polyarteritis nodosa
- Kawasaki disease
- granulomatosis with polyangiitis (synonym: “Wegener’s granulomatosis”)
- microscopic polyangiitis
- eosinophilic granulomatosis with polyangiitis (synonym: “Churg-Strauss syndrome”)
- cryoglobulinemic vasculitis
- IgA vasculitis (synonyms: “hemorrhagic vasculitis”, “Henoch-Schönlein purpura”)
- Hypocomplementary urticarial vasculitis (synonym: “anti-C1q-associated vasculitis”)
- Anti-BMK-associated disease (synonym: “Goodpasture syndrome”)
Primary vasculitis is an independent disease that falls primarily within the competence of rheumatologists, although the diagnosis and treatment of these diseases is impossible without the participation of doctors of other specialties: otolaryngologists, ophthalmologists, neurologists, dermatologists, etc.
The caliber of affected blood vessels in different forms of vasculitis is not the same and varies from large arteries (with a diameter of 1.0 cm or more) to the smallest arterioles, capillaries and venules, visible only under a microscope. The type of inflammation is also different. All this explains the extremely pronounced diversity of clinical manifestations of primary systemic vasculitis and their dissimilarity from each other.
Causes of the disease
The reasons for the formation of primary vasculitis are still unknown to science. Secondary disease can occur against the background of:
- acute or chronic infection;
- genetic (hereditary) predisposition;
- thermal effects (overheating or hypothermia of the body);
- various injuries;
- burns;
- contact with chemicals and poisons.
Another cause of vasculitis can be viral hepatitis. One or more risk factors are enough to change the antigenic structure of tissues. In this case, the immune system begins to secrete antibodies, which further damage the tissue, in this case the blood vessels. This leads to an autoimmune reaction and inflammatory and degenerative processes.
Causes of vasculitis
Doctors cannot yet fully determine the causes of primary vasculitis. There is an opinion that this disease is hereditary in nature and is associated with autoimmune disorders (autoimmune vasculitis), plus negative external factors and infection with Staphylococcus aureus play a role.
The cause of the development of secondary (infectious-allergic vasculitis) in adults is a previous infection.
Other causes of vasculitis include the following:
- allergic reaction (to medications, pollen, book dust, fluff);
- autoimmune diseases (systemic lupus erythematosus, thyroid diseases);
- vaccination;
- abuse of sunbathing;
- consequences of injuries;
- negative reaction of the body to various chemicals, poisons;
- hypothermia of the body;
1 Consultation with an ophthalmologist
2 Consultation with a neurologist
3 ENT consultation
Symptoms of vasculitis
Regardless of the type and form of the disease, the symptoms of vasculitis are similar. These include:
- decreased body temperature;
- joint pain;
- pale skin;
- regularly recurring sinusitis;
- vomiting;
- nausea;
- myalgia;
- rash in the form of spots, urticaria, subcutaneous nodules, hemorrhagic purpura, ulcers or blisters;
- sudden mood swings;
- convulsions;
- intoxication;
- drowsiness;
- sometimes pleurisy, bronchial asthma;
- loss of sensation (insemination);
- exacerbation of cardiovascular diseases;
- weakness;
- lack of appetite followed by weight loss.
Depending on the location, vasculitis can also manifest itself through a sharp deterioration in vision, inflammation and swelling of the eyes, pain in the lower back, in the kidney area, abdominal cramps and disruption of the gastrointestinal tract.
Are you experiencing symptoms of vasculitis?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Systemic vasculitis
Hepatitis
Allergy
Ulcer
Cold
21882 08 December
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Vasculitis: causes, symptoms, diagnosis and treatment methods.
Definition
Systemic vasculitis is a large group of heterogeneous acute and chronic diseases, which are based on inflammation and necrosis of the vascular wall. The term “systemic” means that several organs and tissues are involved in the pathological process. Systemic vasculitis is a rare disease, its prevalence ranges from 0.4 to 14 cases per 100,000 population, but throughout the world the number of people with vasculitis is growing every year.
Causes of vasculitis
The reasons for the development of vasculitis are not yet known exactly. There are primary systemic vasculitis, which are independent diseases, and secondary, which develop against the background of other diseases.
The formation of primary vasculitis is based on genetic defects, and the triggering factors are latent (hidden) infectious processes (hepatitis B, parvovirus, staphylococcus, mycobacteriosis, ARVI), immune hypersensitivity to certain drugs (antibacterial, antiviral, ACE inhibitors, aminazine, etc. .), hypersensitization to certain compounds included in tobacco, etc.
Secondary systemic vasculitis occurs as a syndrome in various diseases, for example, infective endocarditis, rheumatoid arthritis, certain tumor processes, infectious lesions, and drug-induced diseases.
The development of systemic vasculitis is based on various pathological mechanisms, for example, the damaging effect of circulating immune complexes (CIC). In other words, when an antigen enters the body (it can be any microbial agent, a medicinal substance, or its own modified protein), the corresponding immunoglobulin is attached to it. Together they form an immune complex. These complexes begin to circulate throughout the body, deposit on the inner wall of blood vessels and cause inflammation. The more of these complexes and the longer they circulate in the blood, the more damaged the vascular wall is. Increased intravascular pressure, slowing blood flow, and imbalance in the functioning of the immune system contribute to damage.
Other pathological mechanisms underlying vasculitis are the production of pro-inflammatory cytokines by platelets and cells of the inner wall of blood vessels (endothelium) and the appearance in the blood of autoantibodies - proteins that behave aggressively towards the body’s own antigens. These autoantibodies can have a direct damaging effect on the endothelium (antiendothelial antibodies), on the cytoplasm of neutrophils (ANCA - antineutrophil cytoplasmic antibodies), and contribute to the activation of the blood coagulation cascade (antiphospholipid autoantibodies).
Classification of vasculitis
There are a large number of classifications of systemic vasculitis, of which the main one today is the one based on the caliber of the affected vessels and the main mechanisms of their damage:
1. Vasculitis with damage to large vessels:
- Takayasu arteritis (nonspecific aortoarteritis),
- giant cell arteritis (Horton's disease) and polymyalgia rheumatica.
2. Vasculitis with damage to medium-sized vessels:
- polyarteritis nodosa,
- Kawasaki disease.
3. Vasculitis with damage to small vessels:
3.1. Vasculitides associated with antineutrophil cytoplasmic antibodies (ANCA):
- microscopic polyangiitis,
- granulomatosis with polyangiitis (Wegener's),
- eosinophilic granulomatosis with polyangiitis (Churgia-Strauss).
3.2. Immune complex vasculitis:
- diseases associated with antibodies to the basement membrane of the glomerulus (Goodpasture syndrome),
- cryoglobulinemic vasculitis
- IgA-associated vasculitis (hemorrhagic vasculitis, Henoch-Schönlein purpura),
- hypocomplementemic urticarial vasculitis (anti-C1q vasculitis).
4. Variable vasculitis:
- Behçet's disease
- Cogan's syndrome.
5. Vasculitis with damage to the vessels of a single organ:
- cutaneous leukocytoclastic angiitis,
- cutaneous arteritis,
- primary vasculitis of the central nervous system,
- isolated aortitis,
- other.
6. Vasculitis associated with systemic diseases:
- vasculitis in systemic lupus erythematosus,
- rheumatoid vasculitis,
- sarcoid vasculitis,
- other.
7. Vasculitis associated with certain etiological factors:
- cryoglobulinemic vasculitis associated with hepatitis C virus,
- vasculitis associated with hepatitis B virus,
- aortitis associated with syphilis,
- drug-induced immunocomplex vasculitis,
- drug-induced ANCA-associated vasculitis,
- paraneoplastic vasculitis,
- other.
Symptoms of vasculitis
Symptoms of systemic vasculitis depend on which vessels are affected. When skin vessels are involved, symmetrical rashes appear (primarily on the legs), prone to swelling, hemorrhage, and necrosis. Gangrene may develop.
A characteristic skin symptom is “vascular butterfly” - a rash on the cheeks and bridge of the nose (observed in systemic lupus erythematosus).
Hemorrhagic rashes, ulcers and necrosis may also appear on the mucous membranes. Ischemic syndrome in vasculitis is manifested by intermittent claudication - pain in the calf muscles that occurs when walking and forces a person to stop and wait until the pain subsides (also found in other muscles of the legs, accompanied by numbness and coldness of the extremities, can also be observed with damage to the upper extremities). In addition, ischemic polyneuropathy, ischemic lesions of the central nervous system, and asymmetry of arterial pulsation may develop.
Systemic vasculitis is characterized by the involvement of different organs and systems in the pathological process. Damages to the blood vessels of the cardiovascular system can lead to insufficient blood supply to the heart muscle, myocarditis, damage to the inner lining of the heart - the endocardium, and the pericardium - the pericardium. Various rhythm and conduction disturbances occur, and the risk of developing acute myocardial infarction and heart failure increases.
Damage to the bronchopulmonary system includes the appearance of compactions (infiltrates) in the lungs, the development of infarction pneumonia, bronchospasm, and pleurisy.
Renal vasculitis results from damage to the renal arteries. For example, with periarteritis nodosa, multiple painless infarctions occur in the kidneys (death of part of the kidney as a result of artery blockage), which leads to renal failure. Damage to the renal arteries can result in persistent malignant arterial hypertension. Some vasculitis occurs with the development of severe glomerulonephritis - inflammation of the renal glomeruli.
Abdominal syndrome with vasculitis is accompanied by abdominal pain in combination with dyspeptic disorders (feeling of fullness, bloating), nausea, vomiting, ulcers in the stomach and intestines, and a dangerous complication may develop - thrombosis of the mesenteric arteries supplying the intestines.
Damage to the nervous system is manifested by multiple neuritis, pathology of the central nervous system with psychoses, visual disorders, and acute cerebrovascular accidents.
Hemorrhagic vasculitis (Henoch-Schönlein purpura) typically affects the skin, intestines, kidneys, and joints. Skin lesions are manifested by hemorrhagic syndrome - multiple hemorrhages on the feet, legs, thighs, buttocks, shoulders, forearms, and around the affected joints. But they are especially pronounced on the inner surface of the forearms, thighs, legs, and at the locations of the trouser belt and watch strap. Hemorrhages in the intestines are indicated by colic, nausea, vomiting, and bloody stools.
Cryoglobulinemic vasculitis is characterized by damage to the skin and glomeruli of the kidneys. Pinpoint or confluent hemorrhagic purpura appears most often in the area of the lower extremities, buttocks, and lower back. At the same time, patients experience migrating pain in the small joints of the hands and knee joints.
Wegener's granulomatosis occurs with involvement of the respiratory tract and severe glomerulonephritis, leading to decompensated renal failure and often causes death of the patient.
Eosinophilic granulomatosis with polyangiitis (Churgia-Strauss) occurs with damage to the respiratory tract, paranasal sinuses, and allergies. A characteristic symptom is the development of hypereosinophilic bronchial asthma. The kidneys are usually not affected by this vasculitis.
With periarteritis nodosa, medium-sized arteries are mainly affected - aneurysms, blood clots, bleeding due to rupture of aneurysms are formed, and there is a high risk of infarction of the affected organs and tissues. Patients experience severe pain in the muscles (usually the legs), migrating pain in large joints, and damage to the skin, gastrointestinal tract and heart is observed.
With microscopic polyangiitis, small vessels are affected. The disease is characterized by skin manifestations, polyneuritis, inflammatory processes in the respiratory tract, as well as necrotizing glomerulonephritis.
Kawasaki disease/syndrome often occurs in children and is accompanied by fever, inflammation of the mucous membranes, skin, lymph nodes and various systems, primarily the cardiovascular system, which is manifested by tachycardia, arrhythmia, aneurysms and narrowing of the coronary arteries, myocarditis, pericarditis, valvular damage may occur. apparatus.
With Takayasu's disease, or nonspecific aortoarteritis, joints (mainly the upper extremities) and skin suffer with the development of ulcers. Aortic arch syndrome is characteristic - it includes damage to the subclavian arteries, which is manifested by pain, muscle weakness, chilliness of the hands, a sharp decrease or complete absence of pulse in the radial arteries, and stenosis of the carotid arteries. In addition, symptomatic arterial hypertension occurs (due to narrowing of the renal arteries), pressure in the pulmonary artery increases, the arteries of the heart narrow until a heart attack develops, and intermittent claudication is observed.
With giant cell temporal arteritis, the aorta and the large arteries branching from it are affected. A characteristic symptom is inflammation of the temporal artery, which causes a constant, very intense headache, usually on one side of the head.
Diagnosis of vasculitis
There are no specific laboratory tests for most systemic vasculitis. Attention is paid to the clinical picture of the disease, identifying symptoms characteristic of a particular vasculitis.
Then the doctor finds out the systemic nature of the pathological process, which may be indicated by symptoms such as fever, weight loss, muscle and joint pain, anemia, and increased ESR.
Then it is determined whether the disease is primary or secondary, after which clinical and instrumental confirmation of vascular damage is required.
For this purpose, instrumental and x-ray diagnostic methods are used:
- Vascular ultrasound:
- upper limbs;
Diagnostics
It is necessary to try to diagnose vasculitis even in the presence of the very first signs. The disease is serious and dangerous and requires immediate treatment.
If you suspect an illness, you must perform a series of examinations and tests. Appointed:
- angiography;
- general blood and urine tests;
- ECHO-cardiography;
- blood biochemistry;
- Ultrasound of the heart, abdominal organs and kidneys;
- X-rays of light.
The problem is that it is very difficult to diagnose vasculitis in the early stages. But more striking signs of the disease and a reason to sound the alarm appear even when several organs are affected at once.
In severe and rapid progression of the disease, an additional biopsy is performed, followed by a detailed study of tissue samples.
Treatment of vasculitis
Treatment of vasculitis is prescribed depending on the type of organs affected and concomitant diseases. If the primary form of the disease appears against the background of an allergy, it usually disappears on its own and does not require additional measures.
If the source of the disease affects vital organs, such as the heart, brain, kidneys or lungs, then the patient is prescribed a course of intensive therapy.
To stabilize blood circulation, treatment can be carried out both at home and in a hospital setting. Pregnant women, children and patients with severe forms of the disease are required to be hospitalized.
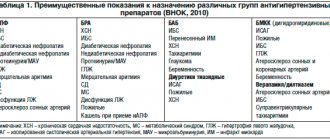
Use:
- chemotherapy;
- corticosteroids;
- NSAIDs;
- anticoagulants;
- enterosorbents;
- antiplatelet agents;
- antihistamines;
- cytostatics.
Additionally, plasmapheresis, hemosorption and immunosorption are included.
FAQ
What is the prognosis for vasculitis?
With timely consultation with a doctor, patient survival is 90%.
Is it possible to treat vasculitis at home?
If the patient’s condition and the identified stage of disease development allows this, then it is possible. Only the most difficult cases are hospitalized. Others can take medications on their own.
If you suspect vasculitis, who should you turn to for help?
First of all, you should make an appointment with a therapist, who, after collecting an anamnesis, will refer the patient to specialized specialists: a vascular surgeon, cardiologist, hematologist, etc.