The heart is a four-chamber organ, consisting of two atria and two ventricles. The atria are divided by the interatrial septum into left and right. The left and right ventricles of the heart are separated by the interventricular septum. Blood in the heart normally moves only in one direction, which is ensured by the functioning valvular apparatus of the heart, consisting of four valves: tricuspid, pulmonary, mitral and aortic.
- The tricuspid valve is located between the right atrium and the right ventricle and allows unidirectional blood flow from the right atrium to the right ventricle.
- The pulmonary valve is located at the exit of the right ventricle and allows blood to flow into the pulmonary artery.
- The mitral valve is located between the left atrium and the left ventricle, through it blood flows from the left atrium to the left ventricle.
- The aortic valve is located at the exit of the left ventricle and allows blood to flow into the aorta and further into the systems and organs of the body.
Structure, localization, anatomy of the tricuspid heart valve
The tricuspid heart valve is located in the area of the atrium and ventricle on the right side.
Its structure is represented by the following elements:
| Name | Description |
| Fibrous ring | Consists of a large number of elastic fibers. Attached to the interatrial septum. A large number of cardiac conduction channels pass through the annulus fibrosus. Some part of this element is represented by muscle fibers and has a loose structure. As the annulus fibrosus moves away from the interatrial septum, its thickness gradually becomes smaller. |
| Doors | In most cases, the normal development of the heart valve involves 3 main leaflets (anterior, posterior and septal). Sometimes their number increases, according to experts, due to the bifurcation of the rear valve. They all vary in size. The largest door is the main one. The structure of these elements provides for the presence of a base, a body and a closure section. |
| Chordae tendons | There are 3 main elements, each of which performs its own specific functions. |
| Papillary musculature | The muscle is located on top of the interatrial septum. The chordae tendineae emerge from it. |
Tricuspid and other heart valves
The condition and functioning of the tricuspid valve is important for normal blood circulation. It prevents the backflow of blood into the right atrium.
Heart and blood vessels
The human cardiovascular system is closed. This means that the blood moves only through the vessels and there are no cavities into which the blood flows. Thanks to the work of the heart and the branched system of blood vessels, every cell in our body receives oxygen and nutrients that are necessary for life.
Pay attention to the established name - cardiovascular system. The first place is taken by the heart muscle, which performs the most important function. We move on to studying this unique organ.
Heart
The branch of medicine that studies the heart is called cardiology (from the ancient Greek καρδία - heart and λόγος - study). The heart is a hollow muscular organ that contracts with a certain rhythm throughout a person’s life.
The outside of the heart is covered by a pericardial sac - the pericardium. Consists of 4 chambers: 2 ventricles - right and left, and 2 atria - right and left. Remember that between the ventricles and atria there are leaflet valves.
Between the right atrium and the right ventricle there is a tricuspid (tricuspid) valve, and between the left atrium and the left ventricle there is a bicuspid (mitral) valve.
In the heart, blood moves unidirectionally: from the atria to the ventricles, thanks to the presence of leaflet (atrioventricular) valves (from the Latin atrium - atrium and ventriculus - ventricle).
The largest human vessel, the aorta, with a diameter of 2.5 cm, departs from the left ventricle, in which blood flows at a speed of 50 cm per second. The pulmonary trunk departs from the right ventricle. Between the left ventricle and the aorta, as well as the right ventricle and the pulmonary trunk, there are semilunar valves.
The muscle tissue of the heart is represented by single cells - cardiomyocytes, which have transverse striations. The heart has a special property - automaticity: isolated from the body, the heart continues to contract without external influences. This is due to the presence of special cells in the thickness of muscle tissue - pacemaker cells (pacemaker cells, atypical cardiomyocytes), which themselves periodically generate nerve impulses.
The heart has a conduction system due to which the excitation that arises in one part of the heart gradually covers other parts. The conduction system includes the sinus node, atrioventricular node, His bundle and Purkinje fibers. It is thanks to the presence of these conducting structures that the heart is capable of automation.
Cardiac cycle
The work of the heart consists of three phases successively replacing each other:
- Atrial systole (from the Greek systole - compression, contraction)
Lasts 0.1 sec. During this phase, the atria contract, their volume decreases, and blood flows from them into the ventricles. During this phase, the leaflet valves are open, the semilunar valves are closed.
Lasts 0.3 seconds. The leaflet (atrioventricular) valves close to prevent blood from flowing back into the atria. The muscle tissue of the ventricles begins to contract, their volume decreases: the semilunar valves open. Blood is expelled from the ventricles into the aorta (from the left ventricle) and the pulmonary trunk (from the right ventricle).
Total diastole (from the Greek diastole - expansion)
Lasts 0.4 seconds. In diastole, the cavities of the heart expand - the muscles relax, the semilunar valves close. Flap valves are open. During this phase, the atria fill with blood, which passively flows into the ventricles. Then the cycle repeats.
We have already discussed the cardiac cycle, but I want to focus your attention on some details. In total, one cycle lasts 0.8 seconds. The atria rest for 0.7 seconds during ventricular systole and total diastole, and the ventricles rest for 0.5 seconds during atrial systole and total diastole. Thanks to this energetically beneficial cycle, the heart muscle gets less tired during work.
Heart rate (HR) can be measured using the pulse - the jerky vibrations of the walls of blood vessels associated with the cardiac cycle. The normal average heart rate is 60-80 beats per minute. An athlete's heart rate is lower than that of an untrained person. With heavy physical exertion, heart rate can increase to 150 beats/min.
Changes in the heart rate are possible in the form of its excessive slowdown or increase, respectively, they are distinguished: bradycardia (from the Greek βραδυ - slow and καρδιά - heart) and tachycardia (from the ancient Greek ταχύς - fast and καρδία - heart). Bradycardia is characterized by a decrease in heart rate to 30-60 beats/min, tachycardia - above 90 beats/min.
The regulatory center of activity of the cardiovascular system lies in the medulla oblongata and spinal cord. The parasympathetic nervous system slows down and the sympathetic nervous system speeds up heart rate. Humoral factors also have an influence (from the Latin humor - moisture), mainly hormones: adrenal glands - adrenaline (strengthens the heart), thyroid gland - thyroxine (accelerates heart rate).
Vessels
Blood moves to tissues and organs inside the vessels. They are divided into arteries, veins and capillaries. We will discuss their structure and functions in general terms. I would like to note: if you think that venous blood flows through the veins and arterial blood flows through the arteries, you are mistaken. In the following article you will find specific examples that refute this misconception.
Arteries carry blood from the heart to internal organs and tissues. They have thick walls containing elastic and smooth muscle fibers. The blood pressure in them is the highest compared to the veins and capillaries, which is why they have the aforementioned thick wall.
The inside of the artery is lined with endothelium - epithelial cells that form a single layer of thin cells. Due to the presence of smooth muscle cells in the thickness of the wall, arteries can narrow and widen. The speed of blood flow in the arteries is approximately 20-40 cm per second.
For the most part, arteries carry arterial blood, but we must not forget about exceptions: venous blood flows from the right ventricle through the pulmonary arteries to the lungs.
Veins carry blood to the heart. Compared to the arterial wall, veins have fewer elastic and muscle fibers. The blood pressure in them is low, so the wall of the veins is thinner than that of the arteries.
A characteristic sign of veins (which you will always notice on the diagram) is the presence of valves inside the vein. The valves prevent the reverse flow of blood in the veins - they ensure unidirectional blood flow. The speed of blood flow in the veins is about 20 cm per second.
Work of the organ
The function of the tricuspid heart valve is to maintain normal blood circulation throughout the human body. Passing through all cells and internal organs, the blood gives off oxygen and receives carbon dioxide back. It is also saturated with decay products, due to which it acquires a dark color.
The work of the tricuspid valve is necessary for the separation of jointly functioning elements (left and right ventricles, atria). Venous blood returns through these sections to the pulmonary circulation. Saturated with oxygen through the left atrium, the ventricle flows into the systemic circulation.
Valve functions
The tricuspid heart valve is located on the right side and is an important element in the functioning of the pulmonary circulation.
It performs the following functions:
- During heart contractions, it prevents blood flow from the lower right ventricle to the atrium.
- Takes direct part in the blood circulation process. The tricuspid valve is responsible for the delivery of venous blood to the vessels located in the bronchi.
- Supports gas exchange in the alveoli of lung tissue and heat transfer.
Continuous blood circulation in the human body throughout his life is responsible for the rapid and timely delivery of oxygenated blood to all internal organs and tissues. Through venous outflow, carbon dioxide and decay products leave the body. In medicine, this mechanism is called the cardiovascular system.
The systemic circulation begins from the left ventricle and ends in the right atrium. The pulmonary circulation is directed from the right ventricle to the left atrium.
Diagnosis of aortic stenosis before TAVI
The following diagnostic measures can help determine aortic stenosis in a patient:
- electrocardiogram (arrhythmia, blockades are determined);
- exercise electrocardiogram;
- radiography (the expansion of the aortic section located above the stenotic area is visualized, an enlargement of the left ventricle of the heart is detected, and calcification of the orifice is determined);
- echocardiography (an increase in size and thickening of the walls of the aortic valve is visualized, left ventricular hypertrophy is established);
- Doppler echocardiography;
- catheterization of cardiac chambers;
- coronary angiography.
Normal valve performance
The tricuspid heart valve is located between the right ventricle and the atrium. When the heart muscle relaxes, it opens. When the myocardium contracts, the valve closes. The valves close tightly due to the presence of chordae and muscles. During normal operation of the tricuspid valve, venous blood passes from the right side of the heart to the left. It is then sent to the lungs for gas exchange.
The backflow of blood into the heart cavity from large vessels is not observed due to the correct functioning of this valve. With the development of pathological processes, the entire mechanism is disrupted, as evidenced by the emerging clinical symptoms.
Pathologies of the 3-leaf heart valve, causes and symptoms
In most cases, pathological changes in the functioning of the tricuspid valve provoke heart failure or the development of stenosis. Degenerative processes impair blood circulation, resulting in characteristic clinical signs.
| Name | Description |
| Failure | A disease characterized by insufficient closure of the tricuspid valve. In this situation, the blood returns back to the atrium. |
| Stenosis | The pathological condition is characterized by narrowing of the holes located in the tricuspid heart valve. In most cases, problems arise against the background of rheumatism, congenital defects, or after prolonged mechanical impact on the chest. |
| Congenital defects | Pathological changes occur during the period of intrauterine development of the human body, often against the background of hereditary diseases in the mother’s body. |
Pathological processes in the area of the tricuspid heart valve develop as a result of the following provoking reasons:
- complication of rheumatism;
- severe thyrotoxicosis;
- development of myocarditis;
- infective endocarditis;
- cardiomyopathy;
- carcinoid syndrome;
- mechanical trauma to the chest, resulting in damage to the heart;
- surgical intervention in the area of the mitral valve, due to which its leaflets enlarged;
- myocardial infarction;
- increase in diameter of the fibrous ring.
Congenital defects in most cases develop together with other hereditary abnormalities (patent foramen ovale, atrial septal defect).
Tricuspid valve dysfunction is also provoked by tumor growths that have appeared on various internal organs. In this situation, disruption of the functioning of the cardiovascular system occurs as a result of the toxic effects of malignant processes.
Developing pathological changes, taking into account the main reason for their appearance, provoke the appearance of certain clinical signs. Symptoms will help the cardiologist determine the degree of damage to the cardiovascular system and assess its ability to function.
Tricuspid valve dysfunction is accompanied by the following symptoms:
- the shade of the skin on the face changes;
- shortness of breath appears;
- breathing is impaired;
- the face swells;
- general weakness occurs in the body;
- the patient is bothered by vomiting; the discharge contains blood impurities;
- metabolism in the intestinal area is disrupted;
- a person gets tired quickly;
- Painful sensations appear in the area on the right side under the ribs.
The liver also enlarges, not only the face, but also the lower and upper limbs swell.
Excess fluid accumulates in the lungs. The intensity of the clinical picture and the presence of certain signs depends on the degree of development of pathological processes. It is important, if any symptom appears, to go to the hospital and undergo a full examination to establish an accurate diagnosis. Properly selected therapy will prevent serious consequences.
Bicuspid aortic valve
Bicuspid aortic valve (BAV) is the most common congenital heart defect (CHD), occurring in 1–2% of people.
Anatomy
In a healthy human heart, the aortic valve normally has three leaflets. They ensure normal blood flow to the heart.
When the fetal heart develops, around the eighth month of pregnancy, two valves may join into one, and instead of three valves there will be two. Therefore, during the first trimester, women are advised to overload and expose themselves to less stress.
Pathogenesis and genetics.
BAV is the result of a violation of the formation of aortic valves during valvulogenesis. Adjacent valves fuse and form one large valve; it is larger than the opposite one, but less than 2 normal ones. BAV is a consequence of a complex defect in the developmental process. The genetic theory of the occurrence of BAV is more substantiated, therefore this defect is often associated with congenital pathologies of the aorta - patent ductus arteriosus and coarctation of the aorta. And subsequently, the disease is often associated with dilatation, aneurysm or aortic dissection. Also, a lack of fibrillin protein at the stage of valvulogenesis leads to the formation of a bicuspid aortic valve.
Clinic
One of the characteristic symptoms of BAV is disruption of blood flow. Accordingly, the main manifestations of the disease include:
- sensation of pulsation in the head;
- sinus tachycardia;
- dizziness, even fainting;
- dyspnea;
- vision problems;
- short-term pain in the heart area, which appears due to ventricular hypertrophy.
Prognosis and complications
When the right coronary and non-coronary leaflets fuse, stenosis can form if there is no excess leaflet tissue, and AV insufficiency if there is prolapse or excess leaflet tissue. Aortic stenosis develops in 15−71%, aortic regurgitation in 1.5−3%, infective endocarditis in 9.5−40%, dilatation and dissecting aneurysm in 5%. Aortic stenosis is more common in middle age, infective endocarditis in young people.
Aortic stenosis
In many cases, developed aortic stenosis requires implantation of a prosthesis. Patients with BAV are prone to premature fibrosis, increased leaflet stiffness and calcium deposition. Echo studies have shown that sclerosis of the BAV begins in the 2nd decade of life, and calcification in the 4th decade, with the valvular gradient increasing by approximately 18 mmHg every 10 years. Also, the development of stenosis can be influenced by hypercholesterolemia and smoking, which contribute to faster wear of the leaflets.
Aortic regurgitation
The etiology of aortic regurgitation in patients with BAV is more complex than in aortic stenosis. Aortic regurgitation can be isolated and occurs when a larger, eccentrically located leaflet prolapses or when the aortic root expands due to the fact that the elastic properties of the valve ring are lost. Because of the association with associated lesions, patients with BAV and aortic regurgitation have a worse prognosis than patients with aortic stenosis.
Infective endocarditis (IE)
IE may develop in 10–30% of patients with BAV. More often at a young age, so tetralogy of Fallot, ventricular septal defect, BAV and mitral valve prolapse are the substrate for 80−90% of cases of the disease in young people.
Conclusions:
To a patient with BAV and aortic dilatation, it is necessary to explain:
- BAV is the most common congenital heart defect;
- An echocardiography study in relatives is necessary, since BAV is a genetically determined disease;
- BAV is often accompanied by aortic root pathology and is prone to valvular and aortic complications that require surgical intervention
- Infectious endocarditis is a common complication of the disease, so prophylaxis with antibiotics is required;
- Early referral to cardiac surgery can facilitate surveillance and prevent life-threatening complications;
- The patient should undergo an annual examination by a cardiologist with echocardiography to identify the progression of aortic dilatation and prevent dissection. Hypercholesterolemia and hypertension should be carefully monitored. Smoking should be avoided.
Be healthy!
Sign up for functional diagnostics
Functional diagnostics doctor - Andrienko Olga Leonidovna
You can make an appointment by calling (391) 205−00−48 or through your personal account
Stages of dysfunction
The tricuspid heart valve is located on the right side of the organ. Pathological changes develop gradually. In medicine, disorders of the functioning of the tricuspid valve are distinguished, taking into account the complexity of pathological changes and the possibility of their reversal.
There are the following stages of development of organ damage:
| Name | Description |
| Stage I | At this stage of pathological processes, minor disturbances occur that affect the movement of the pulmonary and systemic circulation. |
| Stage II | Pathological processes progress, but if treatment is started in a timely manner, degenerative changes can be reversed. |
| Stage III | Significant problems in the functioning of the tricuspid valve provoke the appearance of specific symptoms, for example, increased blood pressure. |
| IV stage | At the last stage of the disease, the valve structure is affected. The person’s condition is deteriorating, progressive symptoms require urgent hospitalization and strict supervision by the attending physician. |
At the last stage of valve damage, pathological processes are irreversible. Properly selected therapy will improve the patient’s quality of life and prevent complications.
Diagnostic methods
A comprehensive examination will help the doctor establish the correct diagnosis and select the most effective treatment regimen.
Patients with damage to the tricuspid heart valve are prescribed the following diagnostic methods:
| Name | Description |
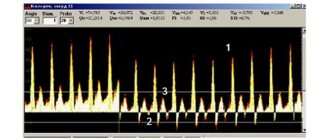
| Electrocardiogram (ECG) | An examination method that will assess the functioning of the heart and identify existing pathological abnormalities. Also determine the volume of the atria. |
| Phonocardiogram | During the examination, the specialist identifies systolic murmurs. |
| X-ray examination | Using the images, the doctor will determine the dilatation of the affected ventricle or atrium, the size of the organ itself, and identify congestion. |
| Echocardiography | The cardiac septa and their movements are observed. Deformation of the valves and the appearance of new formations are also revealed. |
| Spiral computed tomography (CT) | The specialist evaluates the functioning of the main muscle in the human body. |
| Catheterization | The diagnostic method is carried out to determine the pressure in the right side of the heart. |
An important determining point in the diagnosis is the systolic murmur during exhalation. Its presence indicates the development of tricuspid valve insufficiency. Additionally, or before surgery, patients are prescribed coronocardiography. A diagnostic method that will allow you to evaluate blood circulation and detect pathological changes.
Methods of treating diseases
The tricuspid heart valve (located between the right atrium and the ventricle) is treated depending on the degree and stage of its damage, how extensively the pathological processes develop, and the area of their localization. During the period of therapy, it is important to strictly follow all the doctor’s recommendations, without exception, since the disease is life-threatening for the patient.
Drug therapy for damage to the tricuspid heart valve involves the use of the following drugs:
| Group of drugs | Name | Application |
| Diuretics | Britomar, Hydrochlorothiazide | Medicines reduce congestion in the patient’s body and remove excess fluid. The tablets are taken orally, regardless of food, and washed down with plenty of water. Adult patients are prescribed 10-20 mg once a day. If necessary, the dosage is increased to 20-40 mg. |
| Potassium preparations | Panangin, Asparkam | The drugs prevent the accumulation of excess fluid in the patient’s body. The medicine is taken orally 1-2 tablets 3 times a day after meals. The minimum course of therapy lasts 2-3 weeks. In severe situations, the medicine is administered intravenously through a drip. |
| Venous dilators | Corvaton, Nitrosorbide | The drugs reduce the load on the heart and help it accumulate a certain amount of blood. It is recommended to take the tablets at regular intervals and wash down 0.5 tbsp. water. Adult patients are prescribed 1 tablet 1-2 times a day. |
| Anticoagulants | Warfarex, Warfarin | The standard dosage of the drug is 5 mg 1-2 times a day. It is preferable to take the medicine before or after a meal. The course of therapy lasts 6-12 months. |
| Cardiac glycosides | Digoxin, Corglicon | The drugs help eliminate arrhythmia. The medicine should be taken before or after meals. Swallow the tablets whole and take them with plenty of liquid. Take the first dose in a volume of 0.5-1 mg, then every 6 hours at 0.25-0.75 mg for 2-3 days. The maintenance dosage is 0.125-0.5 mg 1-2 times a day. |
| Beta blockers | Diltiazem, Carvedilol | Medicines reduce the contraction of the left ventricle. Adult patients are prescribed 1 tablet 1-2 times a day. The drug is swallowed whole and washed down with a small amount of water. |
During specially selected therapy, patients should also follow the strict recommendations of the attending physician:
- Completely give up bad habits (alcohol, cigarettes).
- Always dress appropriately for the weather to prevent hypothermia or overheating.
- Avoid emotional situations, nervous tension, and severe stress.
- Follow a specially selected diet to reduce the load on a diseased heart.
- Reduce the intensity of physical activity.
Compliance with these recommendations will help not only achieve a positive result in treatment, but also prevent the occurrence of serious complications.
Pulmonary valve insufficiency
Pulmonary insufficiency occurs extremely rarely as a congenital anomaly. However, pathology often occurs as a complication after surgery or percutaneous angioplasty for pulmonary stenosis, as well as treatment for tetralogy of Fallot. Also, pulmonary valve insufficiency can develop as a result of a dilated pulmonary valve ring due to pulmonary hypertension or Marfan syndrome.
Significant pulmonary insufficiency can be caused by primary pulmonary hypertension, secondary pulmonary hypertension, infective endocarditis, rheumatic heart disease, carcinoid heart disease, Marfan syndrome and certain drugs, for example, methysergide, pergolide.
Pulmonary valve insufficiency is a serious pathology that is usually asymptomatic and is not accompanied by signs of right ventricular failure. With this pathology, a soft diastolic murmur is heard in the left upper region of the sternum and hypertrophy of the right ventricle is observed.
When diagnosing this pathology, the following studies are carried out:
- ECG;
- chest x-ray;
- color Doppler echocardiography;
- cardiac catheterization.
Treatment of pulmonary valve insufficiency
Pulmonary insufficiency usually does not require special treatment, but to monitor the pathology, it is necessary to conduct cardiograms every 1-3 years, depending on the severity and cause of the pathology. If symptoms or right ventricular dilatation are present, surgical pulmonary valve replacement is necessary. If severe right ventricular failure and pulmonary hypertension are detected, a heart transplant may be required.
Pulmonary insufficiency is usually well tolerated in childhood. Long-term studies have shown that pulmonary valve regurgitation can lead over time to progressive right ventricular dilatation, right ventricular dysfunction, exercise intolerance, gastric tachycardia, and, in extreme cases, sudden death.
Indications and types of operations
The indication for surgical intervention is the second degree of pathological changes in the area of the tricuspid heart valve. The same applies to the lack of positive dynamics after drug therapy.
The tricuspid heart valve, depending on the location of the pathological foci, is operated on using the following methods:
| Name | Description |
| Annuloplasty | During medical procedures, the fibrous ring of the tricuspid valve is mobilized. U-shaped sutures are placed on the expanded commissures. |
| Semicircular annuloplasty | The operation is performed in case of severe expansion of the fibrous ring of the tricuspid valve. The surgeon uses a purse string suture. |
| Bicuspidization | Suture annuloplasty of the tricuspid valve, which involves placing U-shaped sutures on the fibrous ring in the area of the posterior leaflet. Teflon gaskets are used during this operation. |
| Prosthetics | A method of surgical treatment that is most often used for stenosis or insufficiency of the tricuspid valve. During surgery, the surgeon excises all the main valves and installs artificial prostheses in their place. |
Surgical treatment is carried out using an artificial device that maintains blood circulation in the patient’s body. The surgical method is selected taking into account the anatomical characteristics of the patient’s body and the provoking factors that caused the development of the pathological mechanism.
Diagnosis of heart valve defects
Often, patients learn about problems with heart valves after a full, adequate examination by a doctor, who, during auscultation, identified a heart murmur, after which the patient is prescribed a number of tests that have different diagnostic value:
- transesophageal echocardiography (more complex and more expensive study);
- ECG;
- transthoracic echocardiography (ultrasound of the heart) is the most informative, common and inexpensive way to diagnose pathology of the heart valve apparatus;
- aortoventriculography;
- chest x-ray;
- multislice computed tomography with contrast.
At the initial stage of the disease, the patient may be prescribed medications that help the heart compensate for the excessive load due to valve disease. The selection of optimal therapy in this case should be carried out by an experienced cardiologist. However, heart valve disease is a problem that over time may require surgery to repair or replace the damaged valve.
Indications for heart valve replacement surgery:
- progressive heart failure;
- hemodynamically significant valve lesions;
- ineffectiveness of drug therapy;
- risk of severe complications.
Surgical treatment: heart valve replacement
In recent years, significant progress has been made in the surgical treatment of heart valves. Improvements in technology (including artificial blood circulation machines), the development of uniform standards and protocols for both preoperative examination and the course of the operation have made it possible to reduce the risks of perioperative complications, making the operation on the heart valve apparatus safer than refusing surgery and trying to live with valve dysfunction.
There are basically two types of heart valve surgery:
- prosthetics with artificial or biological prosthesis,
- reconstructive interventions.
It is quite natural that a person’s own valve, after successful reconstruction, functions better than an artificial prosthesis.
Reconstruction of the valve apparatus
The purpose of valve repair is to eliminate the cause of its dysfunction. One of the options for plastic surgery of the mitral valve in case of mitral insufficiency is the removal of part of its posterior leaflet with subsequent annuloplasty or only annuloplasty (strengthening the fibrous ring of the valve using special support rings or reducing the diameter of the fibrous ring using special sutures - plastic according to De Vega, according to Batista, according to Alfieri).
In case of prolapse of the anterior leaflet of the mitral valve, it is possible to perform prosthetic replacement of the anterior leaflet chords, which normally ensure tight closure of the mitral valve. In case of aortic insufficiency, it is possible to perform an operation to normalize the closure of the valve leaflets - plastic according to El-Khoury. In case of valvular stenosis and the absence of calcification of the leaflets and fibrosis of the leaflets and subvalvular structures, it is possible to perform an open commissurotomy (separation of the areas of fusion of the valve leaflets).
Prognosis for pathologies
In most cases, progressive pathological processes with damage to the tricuspid valve lead to serious complications within 5-10 years.
Among the dangerous consequences it is necessary to highlight:
- pulmonary embolism;
- fatal atrial fibrillation;
- congestive heart failure;
- the occurrence of ascites;
- damage to the liver or blood vessels of internal organs;
- development of severe pneumonia;
- the occurrence of gastrointestinal bleeding due to portal hypertension.
As a result of secondary infectious damage to the human body against the background of defects, the risk of complete cardiac arrest increases. Life expectancy for patients with tricuspid heart valve disease is 20-30 years. It is important to constantly be under the supervision of a doctor.
Timely diagnosis of the location of the pathological focus and treatment of the tricuspid heart valve is the main prevention against complications and consequences.
At an early stage of dysfunction, drug therapy will help to cope with disorders. Late stages of disease require surgical intervention. Modern medicine offers enough methods to avoid death and prolong a person’s life.