Normal blood pressure: what is upper and lower pressure
Blood pressure is measured using a device called a tonometer. A cuff (a wide band that compresses) is placed on the arm. This cuff is attached to a device that measures the pressure inside your arteries. When you turn on the blood pressure monitor, the cuff tightens and then slowly relaxes again. It's quick and painless. Eventually, the device will show your blood pressure.
Blood pressure is measured in millimeters of mercury. The blood pressure reading consists of two numbers, for example 120/75. The first (top) number is the pressure when the heart beats (systolic pressure). The second (lower) number is when the heart relaxes (diastolic pressure).
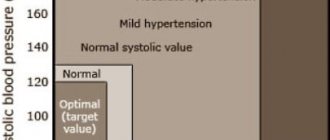
High blood pressure usually does not cause symptoms. The only way to know if your blood pressure is elevated is to measure it. For example, a value of 110/70 is within the normal range for blood pressure; 126/72 – high blood pressure; value 135/85 – stage 1 hypertension (mild), etc. (see table).
Dizziness as a sign of hypotension
Dizziness with low blood pressure is caused by a lack of oxygen in the brain tissue due to a slowdown in the functioning of the hematopoietic system. At the same time that a person feels dizzy, he experiences the following symptoms of exacerbation of hypotension:
- pain in the forehead area that is pressing in nature;
- weakness and loss of performance;
- trembling of hands and feet;
- cold sweat;
- panic attack;
- ringing and squeaking in the ears.
These manifestations of low blood pressure occur for a variety of reasons. In women, the cause may be the menstrual cycle or pregnancy, aggravated by iron deficiency anemia. Blood pressure also drops with chronic lack of sleep, when the body is not provided with a full 8-hour rest.
Low blood pressure (BP) can also be caused by dietary errors, when the body does not receive the necessary nutrients to ensure adequate oxygen access to the brain and internal organs. Also, deterioration of health can occur as a result of poisoning with low-quality and expired products, chemicals, and alcoholic beverages. The situation worsens when a viral or bacterial infection penetrates into a weakened body.
Hypotonic people regularly suffer from weather changes; this phenomenon is called meteosensitivity. The pressure drops especially noticeably in such people when the weather suddenly changes from sunny to rainy or when magnetic storms begin. If during this period a person experienced a stressful or conflict situation, during which there was a significant increase in adrenaline in the blood, after calming down it falls and aggravates the hypotensive state.
Also, a decrease in blood pressure levels is observed after taking certain groups of medications or may be due to an overdose of medications. In this case, you need to monitor the condition of the hypotensive person and consult a doctor in time if more dangerous signs are added to dizziness and weakness. For example, fainting, vomiting and seizures.
What causes high blood pressure
For most people, there is no single cause for high blood pressure. However, there are a number of factors that increase the likelihood of developing hypertension. These are the so-called risk factors - controllable and uncontrollable. You can adjust:
- . When a person smokes, the incoming nicotine increases blood pressure. Over time, this damages the arteries, increasing the risk of heart attack or stroke.
- Eating excess processed foods and salt. Many processed foods contain a lot of salt. Excess salt intake causes the body to store excess water, which increases blood pressure.
- Drinking excess alcohol too often. Drinking alcohol temporarily increases blood pressure. Excessive alcohol consumption on a regular basis can lead to hypertension.
- Excess weight. Excess weight increases the risk of high blood pressure. Even losing just a few pounds can lower your blood pressure.
- Insufficient activity. If a person moves more and sits less, blood pressure decreases.
- . Hormones produced by the body during stress increase blood pressure. Researchers are still trying to understand the exact link between long-term high blood pressure and ongoing stress.
Uncontrollable risk factors include:
- . If a patient has type 1 or type 2 diabetes, they are twice as likely to develop high blood pressure.
- Kidney disease or other gland problems. Sometimes a serious disease that affects the kidneys, arteries, heart, or endocrine system can cause high blood pressure.
- Aging. Blood pressure naturally increases with age.
- Taking certain medications, such as birth control pills.
- A parent or sibling with high blood pressure. High blood pressure runs in families, so if parents or siblings have problems, the risk of hypertension increases.
How often should you check your blood pressure readings?
Blood pressure is usually measured when visiting a doctor (for example, a therapist). There is no need to specifically visit a specialist for this; it is enough to ensure that the pressure is measured at least once every 2 to 5 years, starting from the age of 18 (with normal blood pressure and no increased risk of cardiovascular diseases).
People over 40 years of age, and people 18–40 years of age at risk of high blood pressure, should have their blood pressure checked at a healthcare facility at least once a year. If a diagnosis of arterial hypertension has been established or a person has other risk factors for developing cardiovascular diseases, it is recommended to measure blood pressure more often and not neglect monitoring at home. Your doctor will help you choose a device for measuring blood pressure (tonometer).
For children 3 years of age and older, blood pressure is measured regularly during annual routine examinations.
Caution: The American Heart Association does not recommend the use of wrist- or finger-worn blood pressure monitors, which are less accurate.
If recommended, measure blood pressure at home twice a day on the left and right arm: in the morning before breakfast (but not immediately after waking up) and before taking any medications, and in the evening, preferably at the same time. In each case, you need to measure the pressure 2-3 times (at short intervals, 1-3 minutes) for a confident, accurate result. 30 minutes before, do not smoke, do not eat, do not drink coffee (and alcohol), do not exercise, and empty your bladder. During the measurement, you must sit in a comfortable position, leaning back in a chair or armchair, do not cross your legs and ankles, and do not talk. The arm on which the cuff is worn must be freed from clothing and held at heart level; it is most convenient to place it on a table or armrest of a chair. Don't forget to write down your measurement results.
Symptoms of high blood pressure
High blood pressure is often called the "silent killer" because in most cases it causes no symptoms. The only way to find out if it is there is to measure it with a tonometer. High blood pressure can sometimes be accompanied by one or more of the following symptoms:
- Strong headache;
- dyspnea;
- dizziness;
- nosebleeds;
- severe anxiety.
Usually the headache is in the back of the head; during crises, one often feels dizzy and is accompanied by nausea and vomiting.
Hypertension and its symptoms
Hypertension syndrome is a condition in which a sustained increase in blood pressure develops.
Each person has their own norm, but high blood pressure has an extremely negative effect on the body. This leads to vascular disorders, the heart works harder, which means the risk of heart attack and stroke increases significantly. Important:
Hypertension can develop even in children.
This is due to common birth injuries. You can learn more about this phenomenon from other videos on Dr. Shishonin’s channel
.
Today, hypertension is not a disease of older people. The disease is getting younger, and every year more and more middle-aged and even young people are becoming chronic hypertensive patients. Bad habits, poor environmental conditions, constant stress and a sedentary lifestyle take their toll.
In the early stages, the disease manifests itself with the following symptoms:
- headache;
- the appearance of “flies” before the eyes;
- noise in ears;
- sleep disorders.
The progressive disease not only damages blood vessels, but also negatively affects the condition of the liver, kidneys, and can destroy the retina. However, dizziness is not among the symptoms of hypertension.
What to do with high blood pressure
There are two types of hypertensive crises - both require immediate attention, as they threaten serious complications. It is important to know what to do if you have high blood pressure at home, and how to provide first aid.
If your blood pressure is 180/120 or higher, wait about five minutes and try again. If the second reading is as high and you do not experience any other associated end-organ symptoms such as chest pain, shortness of breath, back pain, numbness or weakness, vision changes or difficulty speaking, it will be considered an uncomplicated hypertensive crisis . Your doctor may simply adjust or add medications, but the condition rarely requires hospitalization.
If your blood pressure is 180/120 or higher, a high pulse with high blood pressure, you are experiencing any other symptoms of end organ damage such as chest pain, shortness of breath, back pain, numbness/weakness, vision changes, or difficulty with a speech, it is important to know what to do. This is a complicated crisis. Don't wait for your blood pressure to drop on its own; call an ambulance.
Dizziness due to hypertension
Professor Olga Dmitrievna Ostroumova gave a lecture “Dizziness with arterial hypertension: is antihypertensive therapy sufficient?”
00:00
Drapkina Oksana Mikhailovna , executive director of the Internet Session, secretary of the interdepartmental council on therapy of the Russian Academy of Medical Sciences:
— Now we are moving on to a new, very interesting section “Dizziness in the practice of a therapist.”
Section consisting of one lecturer and discussion. Professor Ostroumova Olga Dmitrievna. The lecture is called “Dizziness with arterial hypertension: is antihypertensive therapy sufficient?”
Olga Dmitrievna Ostroumova , professor:
— Good afternoon, dear colleagues.
We will talk to you about dizziness. Dizziness is at least one of the most common complaints that patients present (if not the most common complaint).
If you look at any manuals on internal medicine (and not only internal medicine), the description of the clinical picture of almost every disease will contain dizziness. It turns out that the number of diseases that cause dizziness runs into the thousands, if not tens of thousands.
But dizziness is not always correctly diagnosed. It is very difficult to treat it. This is the kind of complaint that almost always remains the last. Other complaints are already going away, but the patient keeps complaining and complaining about dizziness. It feels like this is a saving straw.
Issues of polypharmacy. In order to relieve dizziness, doctors use many medications off-label. In general, the problem, at first glance, is simple, but it turns out to be very complex.
The main problem is that what the patient understands by dizziness, what the doctor understands by dizziness and the formal definition of dizziness are completely different things.
In fact, the patient uses the word “dizziness” most often where it does not exist. He has “lightheadedness”, weakness, darkening of the eyes, and a faint state. The complex of sensations preceding fainting is called the beautiful word “lipothymia”. This is either a decrease in cerebral blood flow or a change in the direction of reducing its supply of oxygen and glucose.
This happens with orthostatic hypotension, with hypoglycemia and a number of diseases of the cardiovascular system (CVS): aortic stenosis, sick sinus syndrome, tachyatrythmia.
02:41
By dizziness, the patient very often understands instability, unsteadiness. When walking, he staggers and throws, especially when turning, changing the pace of walking, or when initiating walking. In particular, this happens with damage to the cerebellum, with peripheral neuropathy, and with a number of diseases of the spinal cord.
Vague sensations that are difficult for the patient to describe: a feeling of heaviness, intoxication, discomfort inside the head. The patient also uses the word “dizziness” very often. In such a situation, most often we will talk about psychogenic dizziness (depression, phobia, anxiety). But not only this, of course. These are the most common options.
The first moment when the patient utters this word, you must try very carefully, with leading questions, to understand what complex of sensations is bothering him. Is it really dizziness?
True dizziness is the illusion of movement of surrounding people or objects around a person. Or, conversely, a person around people or objects. This is understood as true dizziness.
Accordingly, all diagnostic search algorithms, which are described in various manuals and monographs, relate to true dizziness. Once again, as taught in propaedeutics. Very thorough history taking. Try to understand, I emphasize again, with leading questions, what kind of complex of sensations the patient has, whether this is really true dizziness.
Believe me, most likely it will not be true dizziness. Further, based on the complex of sensations, the diagnostic search will go in completely different directions, completely inconsistent with the algorithm for true dizziness.
Our task is to talk about true vertigo. If this is really dizziness, if we completely simplify it without harming the patient, then we distinguish between vestibular dizziness (true, which is associated with the vestibular apparatus) and non-vestibular, that is, beyond it.
Vestibular vertigo. Vestibular apparatus. What is it, what are the options. The first is peripheral (damage to the labyrinth). The second is intermediate (vestibular nerve, transmission of impulses from receptors to the brain). Finally, the central one is where impulses about the position of our body in space come (this is the central nervous system).
05:54
Arterial hypertension is almost the most common complaint of dizziness among patients. Moreover, both before the start of antihypertensive therapy and during it. Including with formal stabilization of blood pressure, when we reach target numbers. It seems that this complaint haunts both patients and doctors.
If you look at whether these are really interconnected things, it turns out that, most likely, according to available data, arterial hypertension itself is not the cause of dizziness. We need to look for other reasons. For now, examine not the disease, but the patient, then treat.
We have already agreed that dizziness is a strictly defined thing - the illusion of the movement of objects around a person or, conversely, a person around objects or other people. The most common cause of true present dizziness in patients with arterial hypertension coincides with that in the population.
Relatively speaking, since hypertension occurs often in older people (more than 80%), the most common cause of true dizziness that exists in the population is involuntarily transferred to this population of patients with hypertension. This is benign paroxysmal positional vertigo. We will return to it later.
The most common cause of non-systemic (non-vestibular) dizziness is psychogenic dizziness. We will not comment on this.
Much more often, it is not hypertension that leads to dizziness, but, on the contrary, an excessive decrease in pressure. I would say, not even so much in terms of numbers (although this also occurs, they reduced the millimeters of mercury too much), but rather would focus your attention on the excessively rapid decrease in blood pressure. Pace, pace and more pace. Even in a state of hypertensive crisis.
Of course, if there is concomitant diabetes mellitus, this is hypoglycemia, rhythm and conduction disturbances, which are partly associated with hypertension, if there is myocardial hypertrophy. But very often with concomitant cardiovascular diseases (CVD) in the patient.
Of course, orthostatic reactions. They generally occur with arterial hypertension. But much more often in elderly hypertensive patients and when arterial hypertension is combined with diabetes mellitus. They happen without treatment. One of the features of hypertension in the elderly is an increase in orthostatic reactions.
Some antihypertensive drugs cause orthostatic hypotension and collapse as side effects. These are β-blockers. We rarely use these drugs to treat hypertension. But now these drugs are gaining popularity among urologists. Very often we began to encounter this indirectly.
09:29
In my opinion, extremely indicative and one of the fundamental works is the work carried out under the guidance of Professor V. A. Parfenov. This is a professor at the Department of Nervous Diseases of the First Moscow Medical University. The department is headed by Academician Yakhno. He deals with this problem a lot.
A very interesting, carefully executed study. 60 hypertensive patients were taken with a complaint of dizziness. The vast majority of situations (80%, four out of five patients) – nothing was found in the patients at all during the most thorough examination. There are no somatic or neurological disorders.
Thus, the first assumption that needs to be confirmed is psychogenic dizziness (anxiety, depression, phobias, and so on).
17% – diseases of the peripheral part of the vestibular apparatus (benign paroxysmal positional vertigo or vestibular neuronitis). We'll talk about it a little.
A most thorough examination revealed a tumor of the cerebellar angle in one patient, and migraine in one patient. One patient had AV block. He was given a pacemaker, after which the dizziness disappeared.
11:03
None of the patients showed a connection between dizziness and increased blood pressure.
Let’s just say a few words about this peripheral dizziness. True dizziness is a defeat of the labyrinth. Peripheral cause, vestibulatory apparatus.
There are also several reasons for dizziness. But we are internists, not specialists in ENT diseases and not neurologists. A few words about benign paroxysmal positional vertigo (the most common cause of dizziness, in the general population, or in a patient with arterial hypertension. After psychogenic).
How does this dizziness manifest itself? Survey, survey and survey again. I won’t tell you anything new since you completed the propaedeutics course. 50% of the success of a diagnosis is a correctly collected analysis and complaints.
Benign paroxysmal positional vertigo (BPPV) is a short, no more than a minute, attack of systemic vertigo that occurs only with a certain position of the head. Most often in a lying position.
A single attack or a series of attacks at the slightest movement of the head. When you interview, the patient paints approximately this picture for you. Despite the extreme lack of time, do not forget to ask leading questions.
There are no neurological or any other symptoms; with repeated provocation of attacks, their severity decreases.
The presence of freely moving particles in the semicircular canals is the most common cause of dizziness.
There are the simplest tests for diagnosing it, which every internist can master. Treatment consists of special exercises, the effectiveness of which is up to 90%. Usually, drug treatment is not even required.
How to be. Of course, the main treatment should be aimed at eliminating the causes that caused dizziness. Treatment of dizziness is a complex treatment. No matter how safe it may seem (when almost everyone has a symptom, it is involuntarily easy to relate to it), we know how difficult it is to treat. The drugs must be used as a complex.
13:59
We have the drug “Betahistine” - an analogue of histamine. Histamine receptors are found in different organs. I want to pay particular attention to the H3 receptors that have been found in the cerebral cortex of rats. Accordingly, high histamine levels cause negative feedback and decreased histamine release.
Histamine receptors are located not only in the central nervous system (CNS), but also in the vestibular apparatus. The vestibular nuclei are very rich in histamine receptors.
Histamine is a very effective remedy in the treatment of dizziness and Meniere's disease, for example. But it is administered intravenously. It has a number of side effects. I think you represent them perfectly. I won't repeat myself. It is obviously unrealistic to treat patients with dizziness with histamine.
The corresponding searches were underway. Betahistine was created. A major study has begun. The drug has been used for quite a long time.
How it affects different types of receptors. Basically, it acts on the third type of receptors (H3 receptors). A powerful antagonist. Doesn't work on H2 at all. On H1 it is a very weak agonist. This action can also be neglected.
This immediately results in a very good safety profile. Low incidence of side effects. It has no effect on other types of receptors (non-histamine).
The drug that I think you know, Betaserc, shows a complex mechanism of action. It improves regional blood flow in the inner ear area. Normalizes the excitation of peripheral receptors. Normalizes the process of excitation in the area of the vestibular nuclei of the brain stem. Quite a wide range of mechanisms of action.
16:10
Appropriate placebo-controlled studies were conducted, where it was shown that Betaserc was significantly different from placebo. It reduces the frequency of dizziness attacks. It also differs from placebo in reducing dizziness severity and duration.
I think that you all have your own experience with this drug. For the sake of order, we talked about how it differs from placebo. Patients of this kind are very susceptible to placebo effects. We have no doubt about the effectiveness of Betaserk.
Let me very briefly recall the indications: treatment and prevention of vestibular vertigo of various origins, as well as a syndrome including dizziness and headache, tinnitus, progressive hearing loss, nausea and vomiting, Meniere's disease and syndrome.
The only contraindication is hypersensitivity to any of the components of the drug.
Like the vast majority of drugs, Betaserc has a dose-dependent effect, including in the treatment of dizziness. The most effective dose is 48 mg/day.
The drug is very good for the speed of onset of effect. Maybe not completely until the dizziness completely disappears, but it is noticeable. Almost 80% (that's four out of five patients) feel either a complete disappearance of dizziness (depending on the severity) or a decrease in the severity and frequency of attacks. Almost everyone else feels the effect on the second or third day. It is extremely rare that the effect develops during the first week. Basically, the drug works on the first day or in the first days.
Recently a new dosage has appeared - 24 mg. Taken twice a day. There is no need to take the daily dose. The lower the frequency of administration, the better the patient’s adherence to therapy. Accordingly, the effectiveness of treatment is higher. There are economic benefits.
We weren’t lazy, we did the math. It turned out that the new dosage of 24 mg is 13% more economical than the dosage of 16 mg. In the old dosage of 8 mg, almost 50%.
The age-old and very difficult question: brand or generic. We will not go deeper into this painful topic. You understand that price should not come at the expense of quality.
In pharmacoeconomic studies there is such an indicator as “price-effectiveness” (the ratio of quality and price). Do we really gain something by paying less money? Or it will turn out to be “money down the drain.”
There was such a pharmacoeconomic study of a number of generics of the drug Betaserc. In short, the drugs Betaver, Vestibo, and so on have significant differences in clinical effectiveness.
Thus, in pharmacoeconomic terms, the drug “Betaserc” wins. It has proven to be most effective in relieving dizziness. There was better tolerance. Costs also indicate that among the three drugs studied, the original drug Betaserc turned out to be the most cost-effective due to its effectiveness. But, unfortunately, this is a very common reason.
This is what I wanted to discuss with you within the allotted time frame. I wish you to feel dizzy only from success.
20:29
High blood pressure danger
A hypertensive crisis (high blood pressure or BP) is a condition when blood pressure rises quickly and sharply, with readings of 180/120 or higher. The consequences of uncontrolled blood pressure in this range can be serious and include:
- stroke;
- loss of consciousness with dangerous injuries;
- memory loss;
- acute cardiovascular diseases;
- eye damage and visual disturbances;
- loss of kidney function;
- aortic dissection;
- angina pectoris (unstable chest pain);
- Pulmonary edema (fluid reserve in the lungs).
If you have been diagnosed with high blood pressure, monitor your readings and take your medications. During an emergency, having the notes with you can provide valuable information to the medical team providing treatment.
Blood pressure readings
- Normal pressure is from 90/60 mm Hg. Art. up to <120/80 mmHg Art.
- Prehypertension (risk factor for the development of arterial hypertension) - 120–129 mm Hg. Art. / <80 mmHg Art.
- Arterial hypertension 1st degree - 130–139 mm Hg. Art. or 80–89 mm Hg. Art.
- Arterial hypertension 2 degrees - ≥140 mm Hg. Art. or ≥90 mm Hg. Art.*
*American Heart Association classification.
Online blood pressure calculator on the NHS website.
American College of Cardiology online cardiovascular risk (stroke, heart attack and other diseases) calculator (risk of complications for patients with high blood pressure over the next 10 years and beyond).
Orthostatic hypotension
Can you count how many times over the past few days, when getting out of a chair or bed, you felt dizzy, your vision went dark, or you had a slight ringing in your ears? A popular piece of advice comes to mind: don’t stand up abruptly. But you did not notice any excessive sharpness in your movement. Getting up from a lying or sitting position constantly causes you similar problems, which go away after a few seconds. In this case, you suffer from orthostatic hypotension.
Orthostatic hypotension is not a disease. In essence, this is an inadequate response of the body to changes in body position, characteristic of men and women of any age. With a sudden change in position, blood accumulates in the veins of the torso and legs, causing a decrease in blood circulation, a decrease in cardiac output and a temporary decrease in blood pressure.
Typical symptoms of orthostatic hypotension:
- dizziness;
- short-term visual impairment;
- fainting.
If you experience severe dizziness and risk of fainting, the following action will help: sit on a chair, put your elbows on your knees, bend your head between your knees.
Orthostatic hypotension in hypertension
Orthostatic hypotension may occur in patients being treated for hypertension. If this condition occurs, you should consult a doctor. Problems disappear or are significantly reduced after adjusting the dosage of the medication taken (lowering the dose or dividing it into several daily doses).
In most cases, 24-hour ambulatory blood pressure monitoring is required as part of diagnosis and treatment. The patient's condition during a routine visit to the doctor often cannot be objectively assessed, since about 1/3 of patients have white coat syndrome.
Orthostatic hypotension with low blood pressure
Orthostatic hypotension is more common in people suffering from low blood pressure. In these patients, when changing position (from sitting or lying to standing), it decreases even more. There are no universal preventive or therapeutic measures.
The occurrence or current state of orthostatic hypotension is also influenced by external factors. Mostly, we are talking about situations that can lead to dehydration. These include:
- high ambient temperature;
- excessive physical activity;
- overdose of diuretic drugs.
Risks of orthostatic hypotension
More often, young people, especially girls, suffer from orthostatic hypotension. It often intensifies during menstruation. The next group is the elderly, in whom this condition causes severe dizziness and falling.
But orthostatic hypotension can also accompany diseases that damage the nervous system, such as diabetes, diseases of the brain and spinal cord. Therefore, if it suddenly appears (especially if there are no problems with low blood pressure before), it is advisable to consult a doctor.
In other cases, low blood pressure is not considered an emergency, except in cases of loss of consciousness, leading to dangerous falls.