Lung cancer is a malignant tumor of the main organ of the respiratory system, capable of growing into the surrounding tissues, destroying them and creating metastases - additional foci of the disease in other organs. Fighting it is an extremely difficult task, since its cells develop rapidly, multiply uncontrollably and move throughout the body through the blood and lymphatic vessels. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes, which act as “filters,” hazardous substances are neutralized and removed from the body. systems
Today, there are many methods to destroy, inhibit the growth or reduce dangerous tumors, but the only way to completely remove them from the body is surgery.
Who should undergo surgery for lung cancer?
Surgery is rarely used as the primary treatment for small cell tumors
, accounting for 15% to 20% of all lung cancer cases. This approach is explained by their very rapid development - in most cases, by the time they are detected, they manage to affect a large number of body tissues, which makes it extremely difficult to combat them. In less than 1 out of 20 patients, they are detected as a single focus that has not spread its cells to the lymph nodes. Lymph nodes are tiny organs of the lymphatic system that detect and neutralize substances dangerous to the body. or other organs. Patients with a similar diagnosis in the initial stages may be prescribed surgery followed by chemotherapy - taking medications that destroy the changed cells. In addition, they are carried out not only with the aim of completely removing the cancer, but also as part of palliative therapy, the goal of which is to relieve symptoms and improve a person’s quality of life.
For non-small cell tumors
the prospects are more optimistic - usually in the early stages such tumors can be completely cured with surgery.
Folk remedies
There are many “folk” methods for treating pulmonary edema. Among the recipes that should help relieve swelling, the most common are formulations based on the following plants:
- Cherry
- Linen
- Liquorice root
- Juniper fruits
- Lovage root
- Steelwort root
- St. John's wort
- Dog-rose fruit
- nettle leaves
- Plantain leaves
- bearberry leaf
These and some other plants in various proportions are offered to be brewed, steamed or infused. Such a solution should help in the treatment of pathology. [3]
Some substances contained in these plants may indeed help relieve symptoms, but are not very effective as a primary treatment.
What is lung and why is it needed?
In a healthy human body there are two such soft, elastic, spongy organs. The right lung consists of 3 main parts - lobes, and the smaller left lung, located next to the heart, consists of two.
How do we breathe?
The air enters the mouth or nose, and then into the trachea, which bifurcates into bronchi, which divide and form small branches - bronchioles. At the end of them are alveoli - tiny sacs that absorb - transfer oxygen into the blood and remove carbon dioxide from it during exhalation. Both organs are surrounded by a thin protective film called the pleura, which helps them slide back and forth along the chest wall during expansion and contraction. Below them is the diaphragm, a thin, dome-like muscle that separates the chest from the abdomen, which contains major vital organs such as the intestines, liver, kidneys, spleen and others. As you breathe, it moves up and down, allowing the lungs to expand and contract in volume, taking in and releasing air.
Lifestyle
In addition to quitting smoking, lifestyle changes can help prevent the progression of COPD and CHF.
- For example, if you are overweight, losing weight will reduce the excess strain on your heart and lungs.
- Stress contributes to hypertension, which worsens the course of CHF. Also, stress triggers repeated exacerbations of COPD, and repeated exacerbations cause COPD to worsen. Thus, stress management plays an important role in slowing the progression of both conditions.
COPD and heart failure are both life-threatening conditions, and although they often occur independently, it is important to understand the connection between them. If you have previously been diagnosed with COPD, you should be aware of your increased risk of developing heart failure. And, if you are a smoker, you need to understand that you are at higher risk of developing both diseases.
Is it possible to remove a lung?
Most people can get by with just one lung, as long as the other is healthy, intact, providing enough oxygen and clearing out carbon dioxide.
The respiratory system plays a very important role, and its improper functioning can affect a person's quality of life. That is why doctors try to preserve a maximum of tissue and remove a minimum - only a small area, or segment. Unfortunately, such intervention is not always sufficient. In case of serious injuries, tuberculosis, severe fungal infections, certain diseases, as well as cancer and its metastases, complete removal of the lung may be necessary.
Causes of fluid in the lung
Pulmonary edema can occur not only with cancer. All causes of this condition are divided into two large groups:
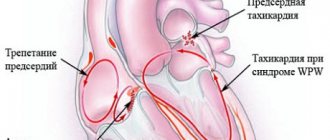
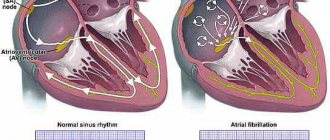
- Cardiogenic - associated with disruption of the heart.
- Non-cardiogenic - associated with other pathological processes in the body, for example, with an increase in the permeability of pulmonary capillaries.
Read more about possible causes of edema:
- Oncological diseases of internal organs
- Various diseases causing sepsis, pneumonia, circulatory congestion
- Overdose of a number of drugs, as well as narcotic drugs
- Effects of radiation on lung tissue
- Heart disease in the stage of decompensation
- Thromboembolism of blood vessels and capillaries of the lungs
In cancer, there are both cardiogenic and non-cardiogenic causes. [2]
Preparing for surgery
Before undergoing surgery, it is necessary to undergo preparation:
- A complete examination, during which doctors assess the patient’s health status, the size and contours of the tumor, the number of tissues affected by the disease, and identify metastases - additional cancerous tumors in various organs. It includes taking tests and performing a whole range of diagnostic procedures:
- blood and urine tests to detect infections and malfunctions of internal organs;
- esophagoscopy – assessment of the condition of the esophagus;
- bronchoscopy - examination of the bronchiBronchi are branches of the trachea through which air passes into the lungs.;
- thoracoscopy - examination of the respiratory organs through small incisions on the chest and back;
- or MRI, during which the doctor receives a clear image of the internal organs, determines the size of the tumor, its exact location and contours;
- sputum cytology - detection of cancer cells in the mucus produced by the respiratory tract;
- mediastinoscopy – study of the condition of the lymph nodes;
- assessment of the condition of the cardiovascular system and other vital organs;
- functional pulmonary tests, which allow us to determine the quality of the respiratory system and the ability to provide the body with oxygen to the tissues remaining after the operation;
- if necessary, the doctor prescribes other procedures.
biopsy - sampling of tumor tissue to study the properties of its cells;
No smoking.
- About bleeding disorders.
Before the operation begins, the doctor talks about the planned intervention, its progress, goals, possible risks, consequences and complications. After which the patient or his legal representative signs a document - informed voluntary consent to medical intervention.
Possible complications
A large volume of fluid in the pleural cavity can provoke a serious complication - acute respiratory failure. It occurs due to compression of the lung tissue by accumulating exudate. The situation can lead to the following adverse consequences:
- Poor circulation and the development of severe cardiac pathology.
- There is a high risk of displacement of organ structures in the middle parts of the chest cavity.
- Attachment of an infectious factor. Empyema of the pleura develops - a purulent process in the pleural cavity.
If an infection occurs, hydrothorax can be complicated by pleural empyema - a diffuse purulent lesion of the pleural layers.
Surgeries to treat lung cancer
Doctors use several methods of surgical treatment of cancer, each of which requires hospitalization in the clinic. The choice of type of intervention depends on the location of the tumor, its size, damage to nearby tissues and lymph nodes - the “filters” of our body that retain and neutralize dangerous substances. Often, specialists prefer to do more extensive surgery to remove as many of the altered cells as possible, since this approach increases the chances of a full recovery.
All such procedures are performed under general anesthesia - using a drug that puts the patient into a deep sleep with loss of consciousness - and are usually performed through a large incision between the ribs on the chest or back. In their course, not only the affected lung tissue is removed, but also the nearest lymph nodes. Such intervention is necessary to identify damage to their altered cells and the spread of oncology beyond the tissues of the respiratory system.
Depending on the type and size of the tumor, the following are used to treat cancer: Lobectomy
– removal of one lobe containing a dangerous neoplasm.
Bilobectomy
– removal of two lobes of the right lung.
Segmental resection
- during this, the surgeon cuts out only the affected segment - a small part of the lobe.
This procedure is suitable for patients whose respiratory system cannot cope with its function if the entire lobe is removed. Pulmonectomy
– complete removal of the lung.
Surgery may be required if the tumor is located near the center of the chest. Sleeve lobectomy
is the removal of a large lesion of cancer located in the main or lobar bronchus. During this procedure, the doctor removes the damaged part of the airway and sews together the remaining tissues located above and below the affected area. This type of intervention can be prescribed as an alternative to pneumonectomy, allowing maximum lung function to be preserved.
Video-assisted thoracoscopic surgery -
VATS
VATS is a minimally invasive procedure for the treatment of early stage cancer, during which a minimal amount of tissue is damaged. Traditional surgeries are performed through a large incision, while video-assisted surgeries are performed through several small punctures in the chest. They introduce special instruments and a thoracoscope - a device with a light source and a camera that displays a clear image on the monitor. The surgeon controls and controls his movements based on real-time video data.
Robotic Assisted Thoracoscopic Surgery –
RATS
RATS is a minimally invasive treatment of small tumors using a robotic system. When performing it, a specialist sits at a console in the operating room and controls the actions of manipulators that remove tumors through small punctures in the patient’s chest. The procedure provides even greater maneuverability and precision when moving instruments than VATS.
VATS and RATS are complex operations, the result of which depends entirely on the skill of the surgeon. They have several important advantages over traditional interventions: they allow minimal tissue trauma, shorten recovery time, shorten hospital stay, reduce blood loss and pain. In addition, they do not leave large scars or scars on the skin.
How is traditional surgery to remove a lung tumor performed?
The prepared patient is brought to the operating room, where he is given anesthesia - a drug that allows him not to feel pain and puts him into a state similar to deep sleep. A tube is then inserted into his throat and connected to a ventilator, and sensors are attached to his body to measure his heart rate, blood pressure and other data. A catheter is inserted into the bladder - a soft flexible tube that drains urine. The skin in the operated area is treated with a disinfectant, after which an incision is made on the front of the chest, running along the rib and ending on the back. A special instrument spreads the ribs, after which a lobe, a small fragment of it - a segment, or the entire lung is removed. One or more tubes are placed in the chest to remove any air or fluid that may form during healing. The wound is sutured or closed with staples, a bandage is applied to it, and the patient continues to be closely monitored until he comes to his senses and all indicators of his body return to normal.
Causes
Sometimes COPD and CHF occur together. They may also develop independently due to overlapping risk factors such as smoking, sedentary lifestyle and obesity. Despite this, the specific physical damage to health that leads to each disease is different. Damage to the lungs causes COPD, and damage to the heart causes CHF. In both cases, the damage occurs slowly and gradually and is irreversible.
| Risk factors | COPD | CHF |
| Smoking | Yes | Yes |
| High blood pressure | No | Yes |
| Heart diseases | No | Yes |
| Genetics | Yes | No |
| Passive smoking | Yes | No |
| High levels of fat and cholesterol | No | Yes |
| Recurrent lung infections | Yes | No |
| Obesity | Yes | Yes |
| Sedentary lifestyle | Yes | Yes |
Surgeries to improve quality of life in lung cancer
Surgery is used not only to completely remove cancer from the body, but also as part of palliative treatment in advanced stages of the disease, the goal of which is to relieve symptoms and improve quality of life.
For example, when a pleural effusion occurs, an accumulation of fluid in the chest outside the lungs, the patient has difficulty breathing. In such cases, the following may be prescribed:
- Thoracentesis
, or
thoracentesis
, is the insertion of a hollow needle into the space between the ribs to drain fluid. - Pleurodesis
is a procedure that prevents its re-formation. During this procedure, a small incision is made in the skin, through which the fluid is removed, after which a substance is injected, causing the mucous membrane of the lung and the chest wall to stick together. This intervention seals the space and limits further accumulation of effusion. - In some situations, it is possible to get by by inserting a catheter
- a thin flexible tube that is inserted through a small puncture and drains the liquid into a special container.
In some patients, pericardial effusion is formed - an accumulation of fluid in the space between the heart and the surrounding membrane, which leads to disruption of the main “pump” that pumps blood throughout the body. In such cases, the following can be done:
- Pericardiocentesis
- Creating a pericardial window
is an operation to remove part of the pericardium - the cardiac membrane. During its course, a hole is created that allows fluid not to accumulate, but to drain into the chest or abdomen.
– removal of effusion using a needle inserted under ultrasound guidance.
Prevention
Prevention of fluid accumulation in the pleura during oncology consists of measures aimed at eliminating the disease that can provoke it. Fluid in the lungs during cancer can accumulate due to diagnoses such as pulmonary tuberculosis, other pulmonary diseases of non-tuberculous origin (pneumonia), and rheumatism. Other measures to prevent it are related to general recommendations for improving the health of the body: a balanced diet, regular exercise, hardening, maintaining a sleep schedule and giving up bad habits that can reduce immunity. [9,11]
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Ilnitsky R.I., Sakharchuk I.I., Dudka P.F., Pleural effusion syndrome: differential diagnosis and treatment tactics. — Ukrainian Pulmonology Journal. 2004, No. 3. - 2004.
- Chuchalin A.G. Pulmonary edema: clinical forms. – Pulmonology 5'2005.
- Montse Rigata, Joan Vallèsa, Jaume Iglésiasb and Teresa Garnatjec. — Traditional and alternative natural therapeutic products used in the treatment of respiratory tract infectious diseases in the eastern Catalan Pyrenees (Iberian Peninsula). — https://dx.doi.org/10.1016/j.jep.2013.04.022
- IN. Sarzhevsky, V.Ya. Melnichenko, V.P. Tyurin. — Pulmonary complications of high-dose chemotherapy and autologous bone marrow transplantation for oncohematological diseases. — Clinical oncohematology, VOLUME 7, NUMBER 1, 2014.
- Mulabecirovich A, Gaulhofer P, Auner H et al. Pulmonary infiltrates in patients with hematologic malignancies: transbronchial lung biopsy increases the diagnostic yield with respect to neoplastic infiltrates and toxic pneumonitis. Ann Hematol.2004; 83: pp.420-422.
- A.G. Chuchalin. — Pulmonary edema: treatment programs. — Pulmonology 6'2005.
- Andrew Baird. — Australian Family Physician Vol. 39, no. 12, December 2010
- Eduardo Henrique Genofre, Francisco S. Vargas, Lisete R. Teixeira. - Reexpansion pulmonary edema. - J pneumol 2003; 29(2):101-6.
- Marco Maggiorini. — Prevention and Treatment of High-Altitude Pulmonary Edema. — Progress in Cardiovascular Diseases 52 (2010) 500–506.
- Susan Davidson. — Diagnosis and treatment of negative pressure pulmonary edema in a pediatric patient: A case report. -AANA Journal/October 2004/Vol. 72, No. 5.
- Mazur Karol, Machaj Dominik, Jastrzębska Sandra. Prevention and treatment of high altitude pulmonary edema (HAPE). — Journal of Education, Health and Sport. 2020;10(2):114-119. eISSN 2391-8306. DOI https://dx.doi.org/10.12775/JEHS.2020.10.02.015.
Removal of metastases from lung cancer
Unlike ordinary, normal cells, cancer cells are able to move throughout the body. They enter the blood and lymphatic vessels. The lymphatic system complements the cardiovascular system. The lymph circulating in it - the intercellular fluid - washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes, which act as “filters,” hazardous substances are neutralized and removed from the body. systems, with their help they spread to various areas, become established in them and create metastases - additional tumors. As a rule, there are several of them, they damage a large number of tissues, and even the most experienced doctor cannot remove all the affected areas. Usually, surgery makes sense only if there is only one such lesion, it is located in the brain, it can be removed without damaging the vital parts of the organ, and the main tumor in the lung can be completely cured surgically or with the help of radiation and chemotherapy.
Research methods
- Spirometry is a test of pulmonary function that will show changes characteristic of COPD, and can also show impaired pulmonary function in CHF.
- Tests such as a chest x-ray, computed tomography (CT) scan, or magnetic resonance imaging (MRI) may show signs of CHF or COPD.
Often with CHF, the heart looks enlarged. When CHF worsens, fluid accumulates in or around the lungs, which can be seen on chest imaging.
Imaging tests may show changes in the lungs consistent with COPD, including thickening, inflammation, and bullae (air-filled spaces in the lungs that compress healthy tissue).
- Echocardiography (ultrasound of the heart) is an ultrasound examination of the structure, structure and mechanical activity of the heart. Using the echo, your doctor can examine the structure of your heart, the blood flow in your coronary (heart) arteries, and the pumping function of the heart muscle itself.
If cardiac function is reduced (often described as low ejection fraction), this may indicate CHF. An echo is not part of the diagnosis of COPD.
Where are surgeries to remove lung tumors performed?
Removing a lung cancer tumor or metastases is a complex intervention that can only be performed by experienced surgeons in specialized clinics, public or private.
Large budget medical organizations have all the capabilities to carry out such operations, but the timing of their implementation and the conditions of stay in the hospital often leave much to be desired. For those who do not want to waste precious time and days of their lives waiting, we offer treatment at an oncological center. We have all the necessary doctors - true professionals with extensive experience in the field of diagnosing and fighting cancer, the most modern equipment and our own laboratory, which reduces the time required to obtain research results to a minimum. We do not create queues, quickly perform all procedures and provide not only surgical but also other oncology treatment, including chemotherapy, immunotherapy and targeted therapy using original drugs that give predictable results. Our specialists are fluent in the most advanced innovative techniques and perform any interventions, and the staff does everything to make the stay in the Center as comfortable as possible for every visitor.
Discharge after surgery for lung cancer
Once the patient’s well-being has stabilized and allows for discharge, doctors confirm the timing of the next appointment and send him home. As a rule, this occurs 5-10 days after the intervention. The rehabilitation period depends on the type of surgery undergone and the amount of tissue removed. For example, it may take several weeks to a month to return to your normal lifestyle and complete recovery after a pneumonectomy.
What should you do after returning from the clinic?
- Get up and walk at least several times a day - movement is extremely important for restoring and establishing proper functioning of the respiratory system.
- Avoid lifting anything heavy for several weeks.
- Follow all of your doctor's instructions about medications, diet, wound care, and drainage—a soft tube that drains fluid that forms during healing.
- Perform prescribed breathing exercises.
- Call your doctor immediately if you have difficulty breathing, fever, swelling - fluid accumulation in some areas of the body, shortness of breath - a feeling of shortness of breath, nausea or vomiting, or cough with or without phlegm.
- Contact your doctor if you have any questions about your symptoms, how you are feeling, or taking any medications, including vitamins and supplements.
You should seek emergency medical help if:
- Coughing up blood or brown sputum.
- Dizziness, fainting or lightheadedness.
- Violation of heart rate.
- Severe pain in the chest area.
- Swelling, redness, pain, or tenderness in the leg.
- When a wound opens, becomes red, swollen, or discharges pus.
Thoracoabdominal department of the Lapino-2 cancer center.
Exacerbations
Both conditions can include exacerbations, which are episodes characterized by worsening symptoms.
- In general, COPD exacerbations are characterized by severe shortness of breath and a feeling of suffocation. They can be triggered by infections, smoke and harmful fumes.
- As a rule, exacerbations of CHF progress more slowly and can be triggered by changes in diet (for example, excessive salt intake).
Worsening of both conditions can occur if you do not take your medications as directed by your doctor. Of even greater concern is that exacerbations of CHF and COPD can occur without an obvious trigger. Both types of exacerbations can be life-threatening and require medical attention.
If you have already been diagnosed with CHF or COPD, you may not notice early signs of the other disease due to the similarity of symptoms. If you notice a change in your symptoms, be sure to tell your doctor - it is possible that you have developed another condition in addition to the one you have already been diagnosed with.
Risks and side effects of lung cancer surgery
Surgery to remove a lung cancer tumor is a serious procedure that can lead to serious side effects. The number and severity of such consequences depend, among other things, on the volume of tissue removed and the general health of the person. During the first few days after the procedure, the patient may feel not only discomfort, but also pain - in the chest, arm, in the area of the incision or in the drainage tube that removes the fluid formed during wound healing.
Risks and possible side effects of surgical procedures for respiratory cancer include:
- undesirable reactions to an anesthetic - a drug that puts the patient into a state of deep sleep and allows you not to feel pain;
- development of bleeding;
- empyema - accumulation of pus in the cavity surrounding the lungs;
- infections;
- damage to organs and structures near the area where surgery was performed, including the heart, nerves, and blood vessels;
- prolonged pain;
- accumulation of air or gas in the chest;
- formation of a bronchopleural fistula - an opening connecting the bronchi with an internal organ or the surface of the chest wall;
- leakage of air from the lung, which leads to compression of the organ and deterioration of gas exchange - disruption of the supply of oxygen and the removal of carbon dioxide.
Treatment methods in Medscan
The Medscan clinic provides all the necessary treatment used for oncology of the lungs, pelvic organs and other internal organs:
- Surgical intervention.
- Radiotherapy.
- Chemotherapy.
- Targeted therapy.
- Immunotherapy.
- Hormone therapy.
Treatment of excess fluid in the lungs during acute pulmonary edema involves intravenous diuretics and the use of an oxygen mask. The patient is recommended cardiological and vascular drugs to stabilize chronic heart diseases.
If fluid in the lungs is a side effect of radiation therapy or chemotherapy, we will resolve this issue as quickly as possible. Our specialists will select the safest oncological treatment options for your health.