UZ "Mogilev City Emergency Hospital"
1. What is Warfarin?
Warfarin belongs to a class of drugs known as anticoagulants. They reduce the blood's ability to form clots in blood vessels. For warfarin to help you, it must be taken correctly, with all the necessary precautions, and strictly following the instructions and advice of your doctor.
It is very important that you understand why you are taking this medicine and follow all your doctor's instructions.
The body functions normally if blood circulates freely through the vessels. Blood clots that interfere with its normal flow are called thrombi. Warfarin slows down the formation of blood clots. Blood clots can form anywhere in the body. During normal operation of the blood coagulation system, only when a blood vessel is damaged, a small clot forms, which stops the bleeding. But if blood clots form spontaneously in the bloodstream, this means that something has gone wrong in the coagulation system. The formation of blood clots is called thrombosis or thromboembolism.
Types of diseases.
This table shows where blood clots form and
| Thrombophlebitis | Blood clots in veins |
| Embolism | Blood clots moving through blood vessels |
| Venous thrombosis | Blood clots in the legs |
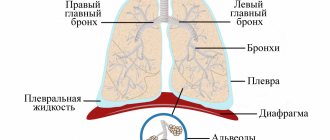
| Pulmonary embolism | Blood clots in the lungs |
| Stroke | Blood clots in the arteries of the brain |
| Atrial fibrillation | Irregular heartbeat, arrhythmia |
| Myocardial infarction | Blood clots in the arteries of the heart |
| Heart failure | Blood clots in the chambers of the heart |
2. Rules for taking warfarin.
- Take warfarin in the dose prescribed by your doctor at the same time. Do not double the dose if you miss a dose, as the risk of bleeding may increase.
- Warfarin is taken according to a specific regimen, selected individually for each patient by a doctor (daily, every other day, or according to another regimen).
You cannot change the order of taking Warfarin on your own.
- Follow the frequency of blood tests for INR recommended by your doctor to monitor the state of blood clotting. After each test, visit your doctor or contact him by phone.
- Use a Warfarin diary and write down each dose of the drug. The form for such a diary is located at the end of this brochure. In a notebook or notebook according to the proposed form, draw the corresponding columns. Show your diary at every doctor's visit.
- Store Warfarin in a cool, dark place and keep out of the reach of children.
- Do not store the medicine in the bathroom, near the kitchen sink, or other damp places. Warfarin can be spoiled by heat and moisture.
- Do not keep the medicine if it is expired or if you no longer take it.
3. WARNINGS.
3.1. Signs of a Warfarin overdose.
If you take Warfarin incorrectly or change your lifestyle, diet, or take other medications, signs of side effects or Warfarin overdose may appear.
If you have:
- bleeding gums when brushing teeth
- unexplained nosebleeds or bruising of the skin
- heavy bleeding from cuts, wounds, menstruation
- blood in urine or black (bloody) stool
- hemoptysis
- severe or prolonged pain
- joint pain, swelling or lumps
- bloody or dark-colored vomit
You need to see a doctor immediately.
3.2. Mode
Avoid vigorous sports, heavy lifting, or other activities that could cause falls or injuries.
Visiting the bathhouse (steam room), manual massage, Charcot shower is not recommended.
Eliminate alcohol, snacks and condiments containing vinegar from your diet.
Avoid exposure to the sun. Swimming in the pool, warm pearl baths, and terrincourt are allowed.
3.3 Be sure to tell your dentist, gynecologist and other doctors, especially if you are undergoing surgery, that you are taking Warfarin.
Some medicines can change (strengthen or weaken) the anticoagulant effect of Warfarin: this includes drugs that
that you buy without a prescription, including aspirin or headache medications, including fever reducers.
Do not take any of the following medications without consulting your doctor.
Medicines that enhance the activity of Warfarin:
- preparations containing aspirin (askofen, citramon, askaf, cardiomagnyl, etc.)
- medications used for arthritis, arthrosis: ibuprofen, indomethacin, naproxen, diclofenac, diclobern, voltaren, xefocam, ketorolac, etc.
- In addition, the following can enhance the anicoagulant effect of Warfarin: glibenclamide, thyroxine, ticlopidine.
Medicines that reduce the activity of Warfarin:
Barbiturates, antihistamines, haloperidol, oral contraceptives, antacids.
Therefore, do not take new or stop taking existing medications without talking to your doctor.
3.4 Diet
Always eat a balanced diet. Vitamin K, found in many foods, reduces the effect of Warfarin, and any changes in your daily diet may change the amount of this vitamin. It is best to keep the amount of vitamin K you receive constant. When you are taking Warfarin, it is especially important not to significantly change the amount of these foods in your daily diet.
A sufficient daily dose of vitamin K is 70-140 mg. If the patient eats large amounts of food high in vitamin K, this food will weaken the effect of Warfarin. A diet with a constant allowed amount of foods containing vitamin K is recommended.
Vitamin K content in the product
| Products | Vitamin K (mg/100g) | Vitamin K content |
| FRUITS | ||
| Applesauce | 2 | Low |
| Banana | 2 | Low |
| Orange | 1 | Low |
| Peach | 8 | Low |
| Raisin | 6 | Low |
| Strawberry | 10 | Low |
| FATS | ||
| Soybean oil | 193 | High |
| Corn oil | 3 | Low |
| Chicken eggs | 11 | Low |
| MEAT AND MEAT PRODUCTS | ||
| Beef liver | 92 | High |
| Bacon | 46 | Average |
| Chicken liver | 7 | Low |
| Ground beef | 7 | Low |
| Ham | 15 | Low |
| Pork liver | 25 | Low |
| Pork fillet | 11 | Low |
| MILK AND DAIRY PRODUCTS | ||
| Oil | 30 | Average |
| Cheese | 35 | Average |
| Cow's milk | 1 | Low |
| GREATS AND CEREALS | ||
| Bread | 4 | Low |
| Corn | 5 | Low |
| Oatmeal | 10 | Low |
| Rice | 3 | Low |
| Wheat flour | 4 | Low |
| Whole wheat grains | 17 | Low |
| BEVERAGES | ||
| Green tea | 712 | High |
| Coffee | 38 | Average |
| Black tea | — | Low |
| Cola | 2 | Low |
| VEGETABLES | ||
| Turnip greens | 650 | High |
| Spinach | 415 | High |
| Broccoli | 175 | High |
| Brussels sprouts | From 800 to 3000 | High |
| Cabbage | 125 | High |
| Cauliflower | 191 | High |
| Salad | 129 | High |
| Asparagus | 57 | Average |
| Green peas | 29 | Average |
| Green beans | 40 | Average |
| Watercress | 80 | Average |
| Tomatoes | 10 | Low |
| Pumpkin | 2 | Low |
| Potato | 1 | Low |
Are you receiving WARFARIN? This drug requires not only weekly INR measurements, but also special nutrition. Deviating from the diet risks thrombosis or bleeding. A natural antagonist of warfarin is vitamin K, which is also found in many foods. Our daily requirement for vitamin K is small. The average person takes 60 to 80 micrograms (mcg) of vitamin K per day. It is necessary for those taking warfarin to control the intake of vitamin K into the body with food. Even a small excess of vit. K, may reduce the effect of warfarin in the body. If you eat foods high in vitamin K, I LOWS!
Increase the risk of thrombosis!
The following foods are very high in vitamin K (more than 200 mcg) and should be eliminated from the diet or strictly controlled: Brussels sprouts, leafy greens, coriander, endive, kale, liver, parsley, red lettuce, spinach, Swiss chard, black and green teas, turnip, watercress. This helps to reduce the INR and the risk of thrombosis increases. If you do eat something high in vit. K, you need to measure the INR and, if the INR drops, immediately consult your doctor.
The following foods have lower levels of vitamin K (100-200 mcg) but can be eaten in small quantities: basil, broccoli, maruli (lettuce), canola oil, green onions, coleslaw, cucumbers (with peel). ), mustard greens, soybean oil, olive oil, blueberries.
The following have an average vitamin K content (50-100 mcg): apples (green), asparagus, cabbage, cauliflower, mayonnaise, nuts (pistachios), summer squash. You have to be careful with them.
Some spices, herbs and dietary supplements may raise the INR and increase the risk of bleeding while taking warfarin: currants, grapefruit, anise, garlic, ginger, asafoetida, chamomile, echinacea, fenugreek, feverfew, ginkgo biloba, ginseng, cordyceps, horse chestnut, sweet clover , cassia, reishi mushroom, red clover, chlorella, wort, martinia (devil's claw), arnica, garlic grass, fish oil (Omega-3), angelica, burdock, alfalfa, chitosan, sage root, omega 3 fatty acids, vitamin E , dandelions. They should also be avoided in your diet if you are receiving warfarin!
This is not a complete list of foods that can interact with warfarin. If you are traveling, it is better not to deviate from your normal diet and be very careful about exotic fruits and berries.
What are anticoagulants? INR indicator
Laboratory diagnostics doctor (head of clinical diagnostic laboratory) Lavitskaya T.V.
Anticoagulants are drugs whose effects on the body reduce blood clotting. They prevent the formation of blood clots (thrombi).
To prevent or treat thrombotic complications, it may be necessary to reduce blood clotting, i.e. cause the blood to clot slightly slower than normal. It is in such cases that anticoagulants are used.
Mechanism of action of anticoagulants:
The synthesis of a number of blood coagulation factors is associated with the influence of vitamin K. Anticoagulants disrupt the connection of vitamin K with the precursors of coagulation factors II, VII, IX and X, disrupting the synthesis of the normal final forms of these substances in the liver.
Anticoagulants currently used.
Currently, there are a number of anticoagulants available in tablets. However, more and more specialists are prescribing warfarin, which has low toxicity and, in terms of its duration of action, is most easily amenable to laboratory monitoring. Warfarin blocks the synthesis of vitamin K-dependent blood coagulation factors in the liver, namely factors II, VII, IX, X and natural blood anticoagulants. The concentration of these components in the blood decreases, and the clotting process slows down. The onset of the anticoagulant effect is observed 36-72 hours after the start of taking the drug, with the development of the maximum effect on days 5-7 from the start of use. After stopping the drug, restoration of the activity of vitamin K-dependent blood coagulation factors occurs within 4-5 days. Warfarin is excreted from the body in the form of inactive metabolites in bile, which are reabsorbed in the gastrointestinal tract and excreted in the urine.
Monitoring the level of coagulation during warfarin therapy.
A patient receiving anticoagulant therapy is constantly balancing between an insufficient dose of the drug, when thrombotic complications may develop, and an excessive decrease in coagulation, when the risk of bleeding increases. Staying safely within an acceptable coagulation “corridor” requires careful and regular clotting monitoring. The INR indicator (International Normalized Ratio, INR) is currently chosen as the parameter monitored worldwide. It reflects the time it takes for a blood clot to form (prothrombin time) adjusted for the sensitivity of the reagent (thromboplastin) used in a particular laboratory. When selecting therapy, coagulation monitoring is carried out several times a week. Upon reaching indicators acceptable in this situation, regular laboratory monitoring is carried out, on average every 2-4 weeks.
The level of clotting may fluctuate even with a stable dose of the drug. The body's susceptibility to the action of anticoagulants depends on many factors: nutrition, physical activity, concomitant diseases, functional state of the liver and kidneys, and concomitant therapy.
It is recommended to check clotting more often:
1.When concomitant therapy changes
2.For a cold or any other disease
3.When the climate changes
4.When changing your usual diet
5.When changing your usual lifestyle
Indications for warfarin therapy:
| Indications | INR value |
| Prevention and treatment of venous thromboembolism | 2,5 (2,0 – 3,0) |
| Treatment of pulmonary embolism | |
| Prevention of systemic thromboembolism in atrial fibrillation and heart defects | |
| Prevention of systemic thromboembolism with mechanical prosthetic heart valves: | 2,5 (2,0 – 3,0) |
| — bicuspid valves in the aortic position; | |
| - bicuspid and unicuspid valves in the mitral position; | 3,0(2,5 – 3,5) |
| - and atrial fibrillation | 3,0(2,5 – 3,5) |
| — and additional risk factors | 3,0(2,5 – 3,5) |
| Prevention of systemic thromboembolism in bioprosthetic heart valves, acute anterior Q-myocardial infarction | 2,5 (2,0 – 3,0) |
| Secondary prevention of myocardial infarction | |
| Critical ischemia of the lower extremities, trophic ulcers | |
| Prevention of thrombosis in antiphospholipid syndrome | 3,0(2,5 – 3,5) |
| Prevention of thrombosis during chemotherapy of stage IV breast cancer | 1,6 (1,3 – 1,9) |
| Primary prevention of myocardial infarction in people at high risk of coronary heart disease. |
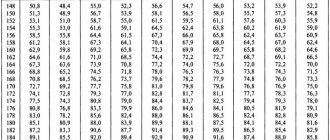
The procedure for selecting the dose of warfarin
Patients taking anticoagulants should keep a diary in which they enter the dose of warfarin, INR level, and the date of INR determination. In most cases, the initial dose of warfarin is 5 mg/day. In the future, the doctor selects the dose of warfarin depending on the INR, which follows after taking two or three initial doses of the drug. Subsequently, INR should be determined daily until stable therapeutic values are obtained, then 2-3 times a week for 1-2 weeks. After achieving stable therapeutic values, INR should be determined at least every 4 weeks (more frequent assessment is advisable in patients with significant fluctuations in the indicator). If adjustment (increase or decrease) of the drug dose is required, the cycle of more frequent INR determination should be repeated until stable indicator values will not be achieved.
INR CONTROL:
Produced in the laboratory in the morning on an empty stomach. Blood is collected from a vein. A reliable result can be obtained if the analysis is carried out in the near future after collecting the material, because Over time, a blood clot begins to form in the blood sample and the true amount of clotting factors decreases.
It is important that you realize that going beyond the “corridor” in either direction is very dangerous.
If coagulability is higher than the limit specified for you, the risk of thrombosis increases. If your clotting rate falls below your limit, your risk of bleeding increases. The full daily dose of warfarin should be taken in one dose, at the same time. The drug is taken orally. If necessary, the tablet or part of it can be chewed and washed down with water.
No two people are alike; the dose prescribed for you depends on your disease and your body’s reaction to the drug.
Tell all doctors, dentists, pharmacists and other health care providers who care for you that you are taking anticoagulants. Do not take aspirin or products containing aspirin without talking to your doctor. Taking medications from this group together with anticoagulants may cause bleeding. Discuss with your doctor which drug you can take as a pain reliever.
DO NOT DO IT:
- independently make changes to the prescriptions made by the doctor;
- change the duration of treatment without the doctor’s instructions;
- take any additional medications without consulting your doctor;
- plan long trips without first consulting a doctor.
Diet: No special diet is usually recommended when taking anticoagulants. However, it must be taken into account that changing the intake of vitamin K can change the effect of the drug. You should not exclude foods containing vitamin K from your diet, but it is recommended to consume them in constant quantities. Alcohol can affect clotting rates. Small doses are probably not harmful, but in large doses and with sudden changes in intake, it significantly increases the risk of bleeding. If you are pregnant, planning a pregnancy, or breastfeeding, discuss this with your doctor! Taking warfarin can negatively affect the development of the child, so during pregnancy you will need to switch to other drugs.
Related medical procedures
Before any medical procedure, be sure to inform your doctor that you are taking anticoagulants and strictly follow his recommendations. On the eve of the procedure, monitoring the level of blood clotting is mandatory. For some dental procedures (filling, canal cleaning, removal of tartar, installation of crowns and bridges), if clotting is within the individual corridor, a change in the therapy regimen is not required. Before tooth extraction, a slight reduction in the dose of the drug taken may be required.
For major surgical interventions, temporary withdrawal of warfarin may be required, but this is only possible in a hospital, under the supervision of a physician. Before a planned surgical operation, the drug is discontinued at least 3 days in advance or the patient is transferred to heparin/low molecular weight heparin injections.
Possible complications of anticoagulant therapy.
The main side effect of oral anticoagulant therapy is bleeding, which can manifest itself in the form of prolonged bleeding from wounds and cuts, nosebleeds, bruising on the body, changes in the color of urine (pink or red) and stool (black, bloody), etc. These complications are rare but can be very dangerous. The risk of complications increases significantly if the INR goes beyond the individual “corridor”. Thus, your efforts should be aimed at maintaining blood clotting within the boundaries of your “corridor”.
Symptoms that should be reported to your doctor immediately
- black coloring of the chair
- pink or red urine
- vomit that resembles “coffee grounds”
- easily occurring bruises and swelling on the body for no apparent reason
- nosebleeds
- excessive bleeding from the gums (especially noticeable when brushing teeth)
- prolonged bleeding from minor wounds and cuts
And:
- shortness of breath, palpitations, chest pain
- dizziness, difficulty speaking
- visual impairment
- numbness or impaired movement of one or more limbs
- sudden cold snap, pain in the limbs
- stomach ache
- sudden increase in body weight
- swelling of the lower extremities
Conclusion
Treatment with warfarin can make your life long and fulfilling. However, the success of therapy largely depends on you. Strict adherence to your doctor's recommendations and regular monitoring of blood clotting levels will ensure a long-term treatment effect and minimize the likelihood of complications.
LOW MOLECULAR HEPARINS
This group of drugs includes dalteparin sodium (Fragmin), nadroparin calcium (Fraxiparin), enoxaparin sodium (Clexane). The drugs affect the activity of factor Xa, as a result of which the formation of thrombin, one of the main components of blood clotting, is suppressed. The advantage of these drugs is that they can be used in outpatient practice with less frequency of monitoring of blood coagulation parameters compared to standard heparin. Low molecular weight heparins are administered intravenously or subcutaneously (into the abdominal area) 1-2 times a day. In community settings, these drugs are most often used for the treatment and prevention of venous thrombosis. Dosages depend on the specific disease, type of drug, and concomitant pathology.
CONTROL - periodically, as prescribed by a doctor, APTT (may be prolonged), prothrombin, platelet count, Xa factor are determined (a special kit is produced for its determination, the analysis is performed in large laboratories).
XARELTO
In outpatient practice, Xarelto (rivaroxaban) is used for the prevention of deep vein thrombosis and the prevention of stroke and arterial thromboembolism in patients with non-valvular atrial fibrillation after orthopedic surgery. The drug is available in tablets of 10, 15 and 20 mg. In most cases, the dosage is 10 mg per day.
CONTROL – periodically, as prescribed by the doctor, prothrombin time, aPTT are determined, Hep Test is performed (performed using a special laboratory kit).
Complexes with this research
Examination during pregnancy.
3rd trimester 9,840 ₽ Composition Female infertility Analysis of women's reproductive health 16,470 ₽ Composition
For those at risk of COVID-19 Diagnosis of diseases complicating the course of coronavirus infection 4,620 ₽ Composition
IN OTHER COMPLEXES
- Women's check-up No. 1 RUB 19,720
- Examination during pregnancy. 1st trimester 17,040 RUR
- Extended coagulogram RUB 4,230
- Coagulogram RUB 2,080
- Men's check-up No. 1 RUB 18,920
Identification of the biologically optimal dose of warfarin
A pharmacogenetic study aimed at determining the individual safe dose of warfarin (an indirect anticoagulant). An analysis is carried out for the presence of mutations in three genetic markers associated with increased sensitivity to warfarin.
Identifying the optimal dose of warfarin allows you to shorten the period of selecting its dose, as well as reduce the risk of hemorrhagic complications.
Synonyms Russian
Coumadin.
What biomaterial can be used for research?
Buccal (buccal) epithelium, venous blood.
How to properly prepare for research?
No preparation required.
General information about the study
Warfarin is the most common indirect anticoagulant drug prescribed for long-term use in a series of cases associated with increased blood clotting, as well as in the postoperative period to prevent the formation of blood clots due to surgery.
It is often practiced to prescribe the drug to people who have suffered strokes or myocardial infarction.
It is generally accepted to determine the effective therapeutic dose of warfarin by the INR value (international normalized ratio). Currently, an increase in INR in the range of 2-3 (up to 3.5 with prosthetic heart valves) is considered a sufficient level of hypocoagulation. It was found that more than a third of patients taking warfarin have INR values outside the accepted range. Excessive or insufficient levels of hypocoagulation may increase the risk of stroke.
With all the advantages of this drug, the selection of an individual dose is of great importance, since exceeding it can lead to hemorrhages and bleeding, and reducing it can lead to strokes and other complications.
Determining the dose using the method of daily INR recording is often ineffective due to the fact that sensitivity to the drug can vary greatly depending on the patient’s diet, lifestyle, and the combined use of other medications. In such cases, the prescribed dose may turn out to be dangerous or ineffective after some time.
Along with clinical data and determination of INR, genetic factors are very important in selecting an individual dose of warfarin. They will allow you to quickly select the physiological dose of the drug and timely adjust the patient’s lifestyle to achieve the required INR values without deviations in the amount of warfarin used beyond the limits of genetically established acceptable norms.
The most significant genes that determine individual response to warfarin therapy are CYP2C9 and VKORC1.
CYP2C9 is a gene that encodes the cytochrome P450 enzyme and regulates the metabolism of warfarin in the body. Genetic markers of CYP2C9 are associated with changes in the functional activity of the cytochrome P450 enzyme, which affects the rate of elimination of warfarin from the body and thereby determines individual sensitivity to anticoagulant therapy.
VKORC1 is a gene encoding subunit 1 of the epoxide reductase-vitamin K complex, the main enzyme of the vitamin K cycle. Warfarin acts by blocking the work of this enzyme, thereby producing an anticoagulant effect (by inhibiting the process of activation of coagulation factors). The genetic marker VKORC1 C(-1639)T is associated with the rate of synthesis and, accordingly, with the concentration of the enzyme in the cell; Based on the genotype, the dose of the drug required to inhibit it, and therefore to reduce the activity of coagulation factors, is determined.
The test is carried out in accordance with the recommendations of the International Warfarin Pharmacogenetics Consortium (Estimation of the warfarin dose with clinical and pharmacogenetic data, The New England journal of medicine, 2009). It is included in the practical recommendations of the European Science Foundation experts on the use of pharmacogenetic testing (2011).
Factors influencing sensitivity to warfarin:
- increasing vitamin K intake with food reduces the anticoagulant effect of warfarin;
- decreased intake of vitamin K from food – potentiates the effect of warfarin (for example, in case of malabsorption syndrome);
- medications that potentiate or inhibit the effect of warfarin.
When is the study scheduled?
- When determining the initial dose of warfarin for patients with thrombosis (pulmonary embolism, acute venous thrombosis, postoperative thrombosis, deep vein thrombosis, arterial thromboembolism, etc.).
- When determining the initial dose of warfarin for patients with a high probability of thrombotic complications (with atrial fibrillation, after myocardial infarction, heart valve and vascular replacement, in the postoperative period, including in orthopedic practice).
What do the results mean?
The result of the analysis is a conclusion on the optimal dose of the drug (mg/day, mg/week), calculated on the basis of the identified genotype for three genetic markers, taking into account the patient’s age, weight, weight, INR value before taking the drug, joint use of drugs (amidarone/ cordarone, fluvastatin) and concomitant pathologies (stroke, diabetes mellitus).
Important Notes
- The information contained in the conclusion of a genetic study should not be used by the patient independently; changing the dose of the drug or discontinuing it occurs only as prescribed by a doctor.
- It is important to discuss diet and lifestyle features during warfarin therapy and the use of other drugs with your doctor.
Genetic markers
- Cytochrome P450 family 2 subfamily C polypeptide 9 (CYP2C9). Detection of the C430T (Arg144Cys) mutation
- Cytochrome P450 family 2 subfamily C polypeptide 9 (CYP2C9). Detection of mutation A1075C(Ile359Leu)
- Vitamin K reductase (VKORC1). Detection of mutation C(-1639)T (regulatory region of the gene)
Also recommended
- Coagulogram No. 1 (prothrombin (according to Quick), INR)
- Coagulogram No. 2 (prothrombin (according to Quick), INR, fibrinogen)
- Coagulogram No. 3 (prothrombin (according to Quick), INR, fibrinogen, ATIII, APTT, D-dimer)
Literature
- Epstein RS. et al. Warfarin genotyping reduces hospitalization rates results from the MM-WES (Medco-Mayo Warfarin Effectiveness study). J Am Coll Cardiol. 2010 Jun 22;55(25):2804-12. [PMID: 20381283]
- Sychev D. A. et al. Anticoagulant effect and safety of warfarin dosing based on the results of pharmacogenetic testing: results of the first Russian prospective study. // Cardiology. – 2010. – No. 5 .
- Sidorenko B. A. Antithrombotic therapy for atrial fibrillation. Moscow, Administration of the President of the Russian Federation, Federal State Institution "Educational and Scientific Medical Center". – 2010.
Reminder for patients taking warfarin.
- The drug is taken daily once a day at the same time in the evening - it is not recommended to take the drug with food, it is better after a meal - it can be taken on an empty stomach - the drug can be prescribed for an unlimited period (the course of treatment is prescribed by your attending physician). Patients taking warfarin should be under strict medical supervision. You will need to regularly and quite often donate blood for INR (especially at the beginning of the prescribed treatment, weekly). The dose of WARFARIN is selected individually, taking into account INR values. WARFARIN is a drug that prevents the formation of blood clots and helps improve blood circulation in organs and tissues; it is directed against blood clotting. The risk of myocardial infarction, stroke, thrombosis of arteries and veins increases if you do not take WARFARIN. WARFARIN can be taken at the same time as other medicines. NEVER CHANGE THE DOSE BY YOURSELF! If you forget to take the drug, take it as soon as you remember, if you do not remember whether you took it today, skip the dose and start taking the drug the next day as prescribed. To be sure that you have taken WARFARIN, we recommend keeping a diary, especially in the initial stages of treatment. HOW TO TAKE CARE OF YOUR SAFETY! When taking warfarin, bruises, bleeding gums, and nosebleeds may occur; with paresis, the blood does not stop for a long time. When signs of increased bleeding appear. Tell your doctor. Your doctor will determine your further actions based on your medical history and concomitant therapy. If there are signs of serious bleeding or loss of consciousness, call an ambulance immediately! Be sure to inform the arriving team, dentist or other doctor that you are taking WARFARIN. Call an ambulance if you experience: -Black (tarry) stools -Pink or red urine -Excessive bleeding from the nose or gums -Unusually heavy or prolonged bleeding during menstruation -Large bruises or swelling on the body for no apparent reason -Prolonged bleeding from small wounds, more than 10 minutes - Appearance of shortness of breath, palpitations, chest pain - Dizziness, difficulty speaking - Visual impairment. Warfarin acts on blood clotting through vitamin K, which is found in varying amounts in food. The maximum amount of vitamin K is found in green leafy vegetables and herbs. There is no need to avoid foods. Nutrition should be complete. Care should be taken to ensure that there are no significant changes in diet, for example depending on the season. If you significantly increase your intake of foods rich in vitamin K while on a stable dose of warfarin, this can greatly weaken its effect and lead to blood clots! The maximum amount of vitamin K is found in dark green leafy vegetables and herbs (spinach, parsley, cabbage in any form), green tea. Mayonnaise, legumes, olive and rapeseed oils contain vitamin K from 300-1000 mcg/kg. Regular consumption of berries and cranberry juice may increase the effect of warfarin. Vitamin K content in products: beef liver………………… ..93 Cheese……………………………………………………….35 Butter………………….30 Egg…… ………………………………..11 Soybean oil……………………….193 Broccoli………………………………175 Cabbage………………… ………………125 Salad…………………………………….129 Tomatoes…………………………….…80 Beans……………………… ………….45 Cucumbers………………30 Green tea…………………………712 Alcohol is not allowed during treatment with Warfarin. What to avoid: - traumatic sports where blows, bruises, and falls are possible. -intramuscular injections -repeated medication intake during the day. Care should be taken to ensure that there are no significant changes in diet, for example depending on the season. If you significantly increase your intake of foods rich in vitamin K while on a stable dose of warfarin, this can greatly weaken its effect and lead to blood thickening and blood clots (with an INR of less than 2.0)! The maximum amount of vitamin K is found in dark green leafy vegetables and herbs (spinach, parsley, cabbage in any form), green tea. Mayonnaise, legumes, olive and rapeseed oils contain vitamin K from 300-1000 mcg/kg. Regular consumption of berries and cranberry juice can enhance the effect of warfarin (that is, thin the blood - increase the risk of bleeding) and the INR will be more than 3.0. Vitamin K content in products: Beef liver………………… ..93 Cheese……………………………………………………….35 Butter………………….30 Egg…… ………………………………..11 Soybean oil……………………….193 Broccoli………………………………175 Cabbage………………… ………………125 Salad…………………………………….129 Tomatoes…………………………….…80 Beans……………………… ………….45 Cucumbers………………30 Green tea…………………………712 Alcohol is not allowed during treatment with Warfarin.
Indirect anticoagulants: warfarin
20s of the XX century. North America. An epidemic of an unknown disease among... cattle. Death of bulls from bleeding during castration and after removal of horns. Spontaneous bleeding during milking in cows. It's all due to moldy clover.
In 1921, local veterinarian Frank Scholfield noticed that all these animals were feeding on sweet clover (Melilotus) silage, which had become moldy in the damp conditions. Scholfield conducted a series of experiments on rabbits and confirmed his hypothesis: the rabbits actually died from bleeding after feeding with moldy sweet clover.
A group of rabbits that ate uninfected hay were alive, active and healthy. Farmers' financial situation did not allow them to replace feed, and the situation remained deplorable and bleeding. American veterinarian L. M. Roderick in 1929 established exactly how blood stops clotting: this is due to dysfunction of coagulation factor II - prothrombin. What kind of substance affects clotting was discovered only 11 years later, and this merit rightfully belongs to a research group at the University of Wisconsin led by Professor Karl Link. One of the researchers, Harold Campell, isolated dicumarol.
Dicumarol is a derivative of plant coumarin, the smell of which we smell next to freshly cut grass. However, coumarin itself does not affect coagulation, but acquires anticoagulant properties only after fermentation (metabolism by fungi of the genera Fusarium, Stachybotrys, Aspergillus, Monopodium and bacteria Clostridium Perfrigens, Escherichia Coli), which is what happened with moldy clover. The result is a full-fledged mycotoxin - dicoumarin.
People first started talking about it as a medicine in 1941. Karl Link, the same professor from Wisconsin, decided to profit financially from his work and register a new rat poison, which was in great demand on farms at that time. Especially for this purpose, in 1948, a new anticoagulant was synthesized and called it warfarin, not forgetting to reflect the group of discoverers (Wisconsin Alumni Research Foundation) in the name. The ending “-arin” hints at coumarin, of course, of which it is a derivative (4-hydroxycoumarin). And only 6 years later it began to be used for medical purposes. The mechanism of action was unknown for a long time, but today we can fully describe it.
Warfarin is called a vitamin K antagonist because it disrupts the synthesis of vitamin K-dependent blood coagulation factors, which are II (prothrombin), IX (Christmas factor), VII (proconvertin), X (Stuart-Prower factor), as well as proteins C (vitamin K-dependent proteolytic enzyme) and S (plasma glycoprotein). The listed coagulation factors depend on vitamin K functionally: the epoxy (oxidized) form of vitamin K is reduced to its hydroquinone form (reduced vitamin K) under the action of the enzyme vitamin K epoxide reductase. Oxidation to the epoxide form (reverse) occurs with the help of gamma-glutamyl carboxylase. It is this enzyme that converts inactive forms of coagulation factors into biologically active ones by carboxylation of their glutamate residues. After carboxylation, coagulation factors can interact with phospholipids of the vascular endothelium and participate in the hemostatic cascade (Fig. 1).
Figure 1 | The mechanism of action of warfarin
But then warfarin bursts in and irreversibly blocks the enzyme vitamin K epoxide reductase, therefore, vitamin K is not restored, and the entire cycle of transformations stops. Gamma-glutamyl carboxylase does not activate clotting factors. The latter circulate in the blood in a functionally inactive form; they are even given the special name PIVKA (proteins induced by vitamin K absence).
For example, the second factor blocked by warfarin, contained in the blood in an inactive form, is called PIVKA-II. Other indirect anticoagulants (phenindione, acenocoumarol, neodicoumarin) also work by this mechanism, but only warfarin has firmly entered into cardiological practice as the drug of choice for the prevention of thrombosis.
Since all these processes occur in the liver, at a systemic level, it is not possible to recreate the effect of the drug in vitro, as is the case with heparin. For the same reason, the effect of hypocoagulation does not occur immediately (after 5–6 days for warfarin, 4–5 days for acenocoumarol), but when the reserves of active coagulation factors in the blood are depleted.
Pharmacokinetics
The drug is used primarily for oral administration, as it is well absorbed from the gastrointestinal tract (80–90%) - therefore, it is convenient for long-term self-administration, but is also used in the form of intravenous injections.
Bioavailability when taken orally reaches 100%. The maximum concentration in the blood is after 4 hours. Capable of accumulation, both material (in the liver, especially with its pathology), and functional, reducing the rate of synthesis of coagulation factors. An important aspect is that warfarin binds to plasma albumin by 97–99%, and the drug has its effect only in free form.
Thus, it is necessary to be careful when combining warfarin with other drugs that also actively bind to blood proteins, since they can displace warfarin from binding to the protein, which increases the level of free (active) warfarin in plasma, and therefore increases the risk of bleeding.
Other drugs that increase the risk of bleeding when used together with warfarin:
- Antidepressants (serotonin reuptake inhibitors). They block platelet aggregation, and their administration together with warfarin increases the risk of bleeding.
- Antibiotics that inhibit the intestinal microflora that synthesizes vitamin K,
- Acetaminophen. Its active metabolite (N-acetylbenzoquinoneline) blocks vitamin K carboxylase even at a therapeutic dose, which is reflected when measuring INR.
99% of the drug undergoes biotransformation in the liver, and this is another pressing issue regarding the combination of drugs. Warfarin, in particular its active S-form, is metabolized in the liver with the participation of cytochrome P450.
Some drugs (for example, cotrimoxazole, metronidazole, ciprofloxacin, norfloxacin, pefloxacin, amiodarone, etc.) block cytochrome P450 and interfere with the biotransformation of warfarin in the liver, resulting in an increase in its concentration in the blood and an increased risk of bleeding.
But there are also drugs that increase the activity of cytochrome, for example, rifampicin, when taken the opposite occurs: warfarin is actively metabolized and excreted from the body, as a result of which the risk of thrombosis increases. Metabolites do not have anticoagulant activity and are excreted by the kidneys (90%) and bile (10%). The drug penetrates the placenta and, as you understand, we will return to this point in the “contraindications” section.
A minute of personalized medicine
The CYP2C9 gene encodes an enzyme involved in the metabolism of warfarin - cytochrome P450. Some alleles of this gene (CYP2C9*2 and CYP2C9*3) determine low enzyme activity, which means slow metabolism of warfarin, high concentration of the drug in the blood and its long-term presence there, hence a strong anticoagulant effect. Such patients require lower doses of the drug to achieve a therapeutic effect.
The VKORC1 gene is also known, encoding the enzyme vitamin K epoxide reductase, the “target” of warfarin. Patients with a G to A substitution at position 1639 of the polynucleotide express less enzyme and are more sensitive to warfarin, and therefore lower doses of the drug are indicated for them.
It seems that this does not find clinical use in modern realities, but the figures vary strikingly: 95% of the population of Asian countries have the A allele and are sensitive to low doses, while among Africans only 14% have it. Mutations in this gene can lead to complete resistance to warfarin.
Indications
The drug is used to prevent thrombosis and thromboembolism. Four pathologies are absolute indications for the use of warfarin for the prevention of thromboembolic complications:
- Atrial fibrillation;
- Venous thrombosis;
- TELA;
- Prosthetic heart valves.
It is also possible to use it in combination with antiplatelet agents to prevent thromboembolic complications in patients with myocardial infarction. It is also used in patients with AF after stenting in the form of triple antiplatelet therapy in combination with acetylsalicylic acid and a P2Y12 inhibitor (clopidogrel/ticagrelor).
However, recent studies show that replacing warfarin with dabigatran in TAT in the combination of aspirin + clopidogrel/ticagrelor has undeniable advantages due to a reduced risk of major or clinically significant minor bleeding.
Dosage regimen
To select the dose and monitor efficacy and safety, the international normalized ratio (INR) is used. This is an assessment method based on comparing the patient’s prothrombin time with the norm, which is expressed by the ratio (note - ISI - international sensitivity index, factory indicator of thromboplastin activity, written on the reagent label):
Prothrombin time, as we know from the course of normal physiology, is the time during which a fibrin clot forms in the blood when calcium chloride and thromboplastin are added to it, thanks to which it is possible to evaluate the external path of hemostasis and the activity of factors I, II, V, VII and X, three of which are blocked by warfarin.
The INR norm for a healthy person not taking warfarin is: 0,8–1,2.
The target INR values when taking warfarin are different for each pathology: for atrial fibrillation, the target INR range is 2–3 , for patients with a prosthetic valve, the INR is 2.5–3.5 .
It is worth remembering that when the INR increases above the recommended figures, there is a high probability of bleeding; when the INR decreases below 2, there is a risk of thrombosis, therefore, when treating with indirect anticoagulants, its strict control is necessary.
Since indirect anticoagulants reveal their therapeutic potential approximately on the 4th day of administration, to prevent thrombosis after cardiovascular accidents, its combination with LMWH (enoxaparin) is recommended according to the following scheme:
In case of asymptomatic risk of bleeding, proceed according to the following scheme:
- INR = 3.5–4.0 : reduce the single dose of the drug by a quarter of a tablet, check the INR after 1 day;
- INR = 4.0–5.0 : reduce the dose by half a tablet, control the INR every other day;
- INR more than 5 : discontinue the drug for a day, control after one day, start therapy with INR less than 3.5; subsequently the dose is reduced by 1 tablet.
If it is necessary to switch to NOAC therapy, it is necessary to bring the INR to <2 (drug discontinuation and daily monitoring of the INR). For your convenience, dear subscribers, we invite you to familiarize yourself with two algorithms for prescribing warfarin: British and American.
Side effects of warfarin
- Bleeding (mainly from the gastrointestinal tract, genitourinary system and even into the ventricles of the brain)
- Liver dysfunction;
- Allergic reactions;
- Necrosis of the skin of the extremities due to thrombosis in the first days of taking the drug (anticoagulant activity appears on the 4th day of use, therefore a combination of low molecular weight heparins and indirect anticoagulants according to the above scheme is necessary);
- Purple toe syndrome (big toe) - it is believed that indirect anticoagulants contribute to the deposition of cholesterol in the veins of the extremities, resulting in impaired blood flow, blood stagnation and soft tissue swelling;
- Teratogenic effect (warfarin penetrates the placenta and can affect the fetus, as it blocks osteocalcin, which leads to hypoplasia of the skull bones, in particular the nose);
- Miscarriages, uterine bleeding, fetal bleeding: all these are terrible consequences of taking warfarin during pregnancy.
Contraindications to taking warfarin
- Pregnancy;
- Erosive diseases of the gastrointestinal tract (erosive gastritis, peptic ulcer and duodenum, ulcerative colitis), the combined use of warfarin with NSAIDs for the listed pathologies increases the likelihood of bleeding from the gastrointestinal tract;
- Urolithiasis, hematuria;
- With caution - in case of liver pathology;
- Age over 80 years;
- Hemorrhagic stroke.
However, it is possible to use warfarin for chronic kidney disease of any stage, unlike NOACs. In case of massive bleeding (often gastrointestinal bleeding), a transfusion of fresh frozen plasma is necessary.
Also, in case of an overdose of warfarin, vitamin K preparations are used. A careful study of the mechanism of action of warfarin begs the question: it is not the vitamin that is blocked, but the enzyme that restores it - how can taking vitamin K change the situation?
The fact is that in addition to vitamin K-epoxide reductase, epoxide can also be reduced by DT-diaphorase, the action of which requires a significantly larger amount of vitamin K, which we will provide by introducing a vitamin K preparation, for example, Vicasol (menadione) or phytomenadione.
Vikasol is administered intramuscularly at a dose of 10–15 mg 2–3 times a day; oral administration of 15–30 mg three times a day is possible. It is also used three days before surgery to prevent massive bleeding. Phytomenadione is taken orally at 0.01–0.02 mg 3–4 times a day. Strict INR control is necessary to prevent thrombosis.
In conclusion, I would like to note that despite the fact that warfarin is the drug of choice for the prevention of thromboembolic complications of cardiovascular accidents, it is imperfect in many aspects: narrow therapeutic window, frequent laboratory monitoring, the influence of food and other drugs on the anticoagulant effect, slow onset and the end of the action.
They were replaced by NOACs, but were never forced out of use: warfarin is cost-effective, it can be used for CKD of any stage, and it is possible to assess the level of coagulation and select the dose, despite the obligation to frequently monitor them.
Sources:
- Wardrop D., Keeling D. The story of the discovery of heparin and warfarin //British journal of haematology. – 2008. – T. 141. – No. 6. – pp. 757-763.
- Kester M., Karpa KD, Vrana KE Elsevier's Integrated Review Pharmacology E-Book: with Student consult Online Access. – Elsevier Health Sciences, 2011.
- Kukes V. G., Mosolov S. N. Clinical pharmacology. – 2004.
- Richard D.H. et al. Lippincott's illustrated reviews: Pharmacology //Philadelphia. – 2006. – T. 3. – P. 413-415.
- Kharkevich D. A. Pharmacology. – GEOTAR-MED, 2003.
- Dean L. Warfarin therapy and the genotypes CYP2C9 and VKORC1. – 2016.
- Juurlink DN Drug interactions with warfarin: what clinicians need to know //Canadian Medical Association Journal. – 2007. – T. 177. – No. 4. – pp. 369-371.
- Martsevich S. Yu., Lukina Yu. V. Warfarin and its significance in the era of new oral anticoagulants. Issues of monitoring the effectiveness and safety of treatment // Rational pharmacotherapy in cardiology. – 2017. – T. 13. – No. 5.
Warfarin and surgery
Warfarin is an anticoagulant - a drug that interferes with the blood's ability to clot by inhibiting the synthesis of vitamin K in the liver. This ability helps prevent the formation of blood clots in certain conditions and diseases.
The fact that Warfarin saves lives and preserves health is also its disadvantage.
By reducing blood clotting, Warfarin increases the risk of bleeding not only from household injuries, but also from surgical interventions, which may be necessary for patients who take it.
In order to minimize both the risk of bleeding and the risk of thromboembolism, before some surgical interventions, patients are switched from the convenient but poorly controlled Warfarin to the inconvenient (because injectable) but well controlled heparin (Fraxiparin).
After discontinuation of Warfarin, INR returns to normal within 3-6 days.
Action plan for planned surgical treatment
- Determine MHO one week before the scheduled surgery.
- Stop taking Warfarin 1–5 days before surgery.
- In case of a high risk of thrombosis, low molecular weight heparin is administered subcutaneously to the patient for prophylaxis (depending on the intervention and the type, heparin is discontinued 6-12-24 hours before surgery).
- The duration of the pause in taking Warfarin depends on the MHO. Warfarin is stopped:
- 5 days before surgery, if MHO >4;
- 3 days before surgery, if MHO is from 3 to 4;
- 2 days before surgery, if MHO is from 2 to 3.
- In the postoperative period, it is necessary to continue subcutaneous administration of low molecular weight heparin for 5–7 days while reinstating Warfarin.
- Continue taking Warfarin:
- with the usual maintenance dose on the same day in the evening after minor operations and on the day,
- after major operations, when the patient begins to receive enteral nutrition.
- Once the target INR is reached, heparin is discontinued.
Dental extraction/treatment does not require any preparation. Warfarin discontinuation is not required.
It is necessary to ensure that the INR value does not exceed the therapeutic range.
In case of bleeding, you can use a 5% aqueous solution of aminocaproic acid to rinse the mouth up to 4 times a day for one to two days.
Aspirin, other non-steroidal anti-inflammatory drugs and COX-2 inhibitors should be avoided.
Discontinuation of Warfarin without heparin coverage for tooth extraction carries an ~1% risk of thromboembolic complications.
When considering endoscopic surgery, the doctor evaluates two parameters: the risk of bleeding from the procedure and the risk of thromboembolic complications for which the patient is taking Warfarin.
Examples of high-risk bleeding procedures:
- Polypectomy or endoscopic resection
- Coagulation or other thermal effects on tissue
- Endoscopic sphincterotomy
- Dilatation (widening) of strictures (narrowings)
- Endoscopic gastrostomy
- Endoscopic biopsy of parenchymal organs
Examples of low bleeding risk procedures:
- Diagnostic gastroduadenoscopy, rectoromanoscopy, colonoscopy (with or without biopsy)
- Retrograde cholangiopancreatography (ERCP)
- Biliary tract stenting without sphincterotomy
Conditions and diseases with a high risk of thromboembolism:
- Atrial fibrillation associated with heart disease (including after mitral valve replacement)
- Atrial fibrillation associated with congestive heart failure or left ventricular ejection fraction <35 percent
- Atrial fibrillation, with a history of thromboembolic events
- Atrial fibrillation associated with hypertension, diabetes mellitus, or age >75 years
- Mechanical valves in mitral position
- Mechanical valves in patients with a history of thromboembolic events
- Coronary stenting within one year
- Acute coronary syndrome
- Percutaneous intervention on the coronary arteries without stenting (balloon angioplasty)
Conditions and diseases with a low risk of thromboembolism:
- Deep vein thrombosis
- Chronic or paroxysmal form of atrial fibrillation that is not associated with heart disease
- Bioprosthetic valves
- Mechanical valves in aortic position
By balancing the risk of bleeding from the procedure and the risk of thromboembolic complications in a particular patient, the doctor will recommend the appropriate course of action.
If the procedure is associated with a low risk of bleeding, then discontinuation of Warfarin is not required.
If there is a high risk of bleeding, preparation is carried out under the cover of heparin.
If a patient has a situation requiring emergency surgery , then the main task of doctors is to neutralize the effect of Warfarin.
For this purpose, vitamin K preparations are used (the use of provitamin K, Vicasol, is not justified for these purposes) and fresh frozen plasma.
After neutralization of Warfarin, emergency surgery is performed.
Surgeon
Kachan L.N.