In defibrillation, the shock is delivered randomly in relation to the phase of the cardiac cycle. As a matter of common sense, the use of defibrillation should be limited to cardiopulmonary resuscitation. But situations are different. And sometimes defibrillation has to be used for the same indications as cardioversion. In this case, there is always a risk of developing ventricular fibrillation (about 0.4%). Repeated defibrillation, which must be carried out as soon as possible, usually restores the rhythm.
A defibrillator is a device that generates an electrical impulse of the required duration and power (measured in Joules). Based on the pulse shape, defibrillators are divided into monophasic and biphasic. The latter are considered the most effective. Medical advice: If you do not know what type of device your defibrillator is, consider it monophasic.
Defibrillation
It is performed for the following rhythm disturbances. When performing cardiopulmonary resuscitation, defibrillation for these rhythm disturbances should be performed as early as possible. If more than 3 minutes have passed since the fatal cardiac arrhythmia, defibrillation should be preceded by chest compressions.
Children: initial power approximately 2 J/kg body weight, repeated defibrillation - 4 J/kg body weight.
Contraindications: refusal of resuscitation measures.
| Indications for defibrillation and recommended initial shock power for adult patients: | |||
| Type of arrhythmia | Pulse power in joules (J) | ||
| monophasic | biphasic | ||
| Ventricular fibrillation | 360 J or maximum power | 150-200 J | |
| Polymorphic ventricular tachycardia | 360 J or maximum power | 150-200 J | |
| Pulseless ventricular tachycardia | 360 J or maximum power | 150-200 J | |
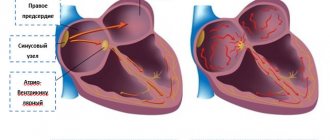
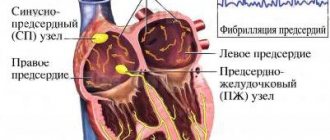
The term "electrical cardioversion" refers to a method of restoring normal heartbeat in cases of heart rhythm disturbances, such as atrial fibrillation. The goal is to return the heart to what is called sinus rhythm—a normal, regular heartbeat. Atrial fibrillation is a functional disorder in which the propagation of excitation occurs uncoordinated. Based on sinus rhythm, the rhythmic movement of the heart is regulated. Electrical cardioversion attempts to restore orderly activity to the sinus node, the electrical clock generator of cardiac activity, so that the heart beats at the correct rhythm again.
What should be considered before performing electrical cardioversion in patients with atrial fibrillation?
If atrial fibrillation is diagnosed, the therapeutic goal may be to control the heart rhythm. Electrical cardioversion is a non-invasive intervention, that is, without surgery, to normalize the heart rhythm.
Since electrical cardioversion for atrial fibrillation is associated with an increased risk of embolism, before each intervention it is necessary to determine in the case of each individual patient whether this method of treatment is personally suitable for him.
In patients with atrial fibrillation, blood clots called thrombi may form in the atria of the heart due to irregular blood flow. If they break off and travel with the bloodstream to the brain, such blood clots can block an artery and thereby lead to a stroke. The reasons for a thrombus leaving the atrium with the blood flow may be different. For example, such a reason may be a current pulse, which is also given during electrical cardioversion. Therefore, before performing electrical cardioversion, it is so important to exclude the presence of a thrombus in the atrium. Transesophageal echocardiography (TEE) can clarify the situation. In this case, we are talking about an ultrasound examination, during which certain areas of the heart are especially clearly visualized from the esophagus, which makes it possible to confidently determine the presence of blood clots. This preliminary examination is largely painless for the patient, since local anesthesia of the larynx is performed before it using an anesthetic spray.
How is electrical cardioversion performed?
For patients whose atrial fibrillation has been present for more than 48 hours or whose duration is unknown, the European Society of Cardiology recommends oral anticoagulation therapy for at least three weeks before electrical cardioversion. After the intervention, anticoagulant therapy continues for another four weeks.
Typically, electrical cardioversion is performed on an outpatient basis. In order to eliminate the possibility of ingesting food debris or anything similar directly during the intervention, it is necessary that the patient comes to the clinic or medical practice at the appointed time on an empty stomach. Also, to conduct the study, patients must bring the following documents with them:
- results of previous studies, if available (possibly results of transesophageal echocardiography, during which no pathological features were detected)
- patient's medication passport or list of prescribed medications (you may need to ask your family doctor)
- referral for testing from a family doctor
Electrical cardioversion is performed under short-term anesthesia and therefore the procedure is painless for the patient. During the entire treatment, the patient's ECG is constantly monitored. With the help of current pulses (the dose of which is much lower than, for example, defibrillation), the heart rhythm returns to sinus rhythm. The impulse generator for the current impulses is the heart's own beat, which is recorded during the ECG. In this way, the risk of ventricular fibrillation can be reduced.
After successful electrical cardioversion, the patient has time to calmly recover from the short-term anesthesia. Although the drug effect is minor, the patient should no longer work or drive a car that day.
During the final conversation, the attending physician sets a date for the first follow-up examination, during which an ECG will be used to check whether the correct heart rhythm is maintained. Regardless of whether sinus rhythm is maintained after electrical cardioversion, patients with an existing risk factor for stroke or with recurrent atrial fibrillation are advised to undergo lifelong oral anticoagulation therapy.
Cardioversion
Indications
1.Fibrillation (atrial fibrillation) or atrial flutter
A. Atrial fibrillation or flutter for more than 48 hours (or unknown duration) subject to anticoagulant therapy for 3-4 weeks with maintenance of MHO in the range of 2-3;
b. Paroxysm of atrial fibrillation or flutter, accompanied by hemodynamic disturbances or other dangerous conditions:
- angina pectoris;
- myocardial infarction;
- pulmonary edema;
- arterial hypotension;
- heart failure.
V. Atrial fibrillation or flutter of any duration in the absence of thrombi in the left atrium and left atrial appendage according to transesophageal echocardiography;
d. Atrial fibrillation or flutter less than 48 hours old (the appropriateness of anticoagulant therapy depends on the risk of embolic complications).
2. Atrial tachycardia;
3. AV nodal reciprocal tachycardia;
4. Reciprocal tachycardia with the participation of additional pathways.
Selecting the initial discharge power
| Indications for cardioversion and recommended initial shock power for adult patients: | |||
| Type of arrhythmia | Pulse power in joules | ||
| monophasic | biphasic | ||
| Stable monomorphic ventricular tachycardia | 100 J | 100 J | |
| Atrial fibrillation | 360 J | 200-360 J | |
| Atrial flutter | 50-100 J | 50-100 J | |
| Paroxysmal supraventricular tachycardia | 50-100 J | 50-100 J | |
Contraindications
1. Thrombi in the atria in the absence of indications for emergency cardioversion;
2. Sinus tachycardia;
3. Tachycardias caused by increased automaticity:
- Polytopic atrial tachycardia;
- Accelerated AV nodal rhythm.
4. Glycoside intoxication;
5. Severe electrolyte disturbances in the absence of indications for emergency cardioversion;
6. Atrial fibrillation of unknown duration in the absence of anticoagulant therapy and transesophageal echocardiography data;
7. Contraindications to anesthesia.
Preparing for elective cardioversion
- The patient must sign consent for cardioversion;
- Before anesthesia, the patient should not take food or liquid for 4 hours;
- In patients undergoing elective cardioversion, transesophageal echocardiography is indicated to identify thrombi in the left atrium. Standard echocardiography is not informative enough in this regard;
- It is recommended to discontinue cardiac glycosides 3-4 days before the procedure;
- Potassium levels should be 4.0-5.0 mmol/L.
Anesthetic care
Patients undergoing cardioversion need to switch off consciousness. Preparation, preoperative examination, equipment are generally accepted in anesthesiology. Monitoring is standard. Features : intravenous anesthesia is superficial and short-term - pay attention to the recommended doses of anesthetics. Anesthesia is usually carried out while maintaining spontaneous breathing in the patient.
Cardioversion is performed as soon as the patient loses consciousness (floating eyeballs, loss of speech contact) - under conditions of superficial anesthesia. Due to decreased cardiac output, the onset of anesthesia may be delayed. Doctors are in no hurry to increase the dose of anesthetic above the recommended values - this is fraught with the development of hypotension and respiratory depression. Kits for tracheal intubation and temporary pacemaker should be ready.
It is recommended to pre-dilute 1 mg of epinephrine in a syringe in 10.0 ml of 0.9% sodium chloride in case of a sharp drop in blood pressure - administer 1 ml as a bolus if necessary. Advice to doctors: do not include narcotic analgesics and atropine in premedication.
Performance
1. Preoxygenation;
2. Intravenous anesthesia, one of the following drugs is used:
- Propofol 40-80 mg, drug of choice;
- Midazolam 5-15 mg, not very convenient due to prolonged sedation;
- Sodium thiopental 1% – 100-200 mg;
- Ketofol (propofol 100 mg + ketamine 100 mg) – 3-6 ml of mixture, indicated for hypotension in the patient.
All of these drugs should be administered very slowly.
Equipment
- Defibrillator with ECG monitor and external pacemaker;
- Spare defibrillator;
- ECG monitor with electrodes;
- Gel for electrodes.
Attention. A defibrillator can break down at the most inopportune moment, which can have unpredictable consequences for the patient. A spare defibrillator, even a simple one, will avoid problems.
How to correctly position defibrillator electrodes during defibrillation and cardioversion
The standard location is the anterolateral arrangement of electrodes: one on the right under the collarbone near the sternum, the second on the left above the apex of the heart. But with the same effectiveness, depending on the situation, you can use other options for the location of electrodes, for example, anterior-posterior, when one electrode is located near the sternum on the left approximately at the level of the fourth intercostal space, and the second is opposite it from the back. Or: anterior-left subscapular and anterior-right subscapular.
If the patient has an implanted pacemaker or cardioverter-defibrillator
During defibrillation and cardioversion in patients with implanted pacemakers, the electrodes are usually installed in the anteroposterior or anterolateral position. Do not place the electrode directly over the implanted device. They try to choose a position so that the distance between the electrodes and the pacemaker is > 8 cm. After the procedure, the operation of the pacemaker or cardioverter-defibrillator is checked.
Publications in the media
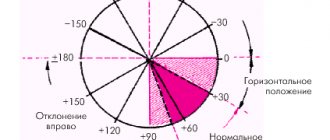
Cardioversion is the termination of tachyarrhythmia with a defibrillator discharge synchronized with the least vulnerable phase of the electrical ventricular systole (usually 20–30 ms after the apex of the R wave).
• Unlike ventricular fibrillation (VF), when eliminating tachyarrhythmia, there is a danger of delivering an electric shock in the most vulnerable phase of the cardiac cycle. In order to prevent VF in the treatment of a permanent form of atrial fibrillation or paroxysmal tachyarrhythmias, a cardioverter was proposed - a complex of a direct current defibrillator and an electronic synchronizer that delivers a discharge at a certain moment of the electrical activity of the heart.
• Electrical defibrillation and cardioversion are usually combined under the term electrical impulse therapy (EPT).
EIT methods
• External (transthoracic) EIT is the main method. Both electrodes are placed on the chest so that the heart is covered by the electric field of the capacitor discharge. For adults, the discharge value is from 50 to 360 J (4–7 kV). In children, shocks are used at a rate of 2 J/kg body weight.
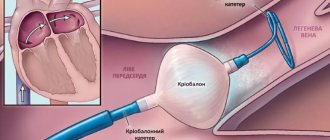
• Internal EIT - electrodes are applied directly to the heart. In this case, a significantly smaller discharge value is required (for an adult patient - about 500 V or 12.5–25 J).
• Transesophageal EIT - one of the electrodes is inserted into the esophagus to the level of the atria, the other is placed in the precordial region. Discharge energy is 12–25 J. Transesophageal EIT is indicated for severe supraventricular tachyarrhythmias that are resistant to transthoracic discharges, as well as for suppressing severe ventricular tachyarrhythmias with low-energy discharges.
• Transvenous intracardiac EIT using a multipolar electrode, which is installed in the right ventricle, is used in intensive care units for recurrent ventricular tachycardia. The discharge energy during endocardial EIT varies from 2.5 to 40 J. To relieve atrial fibrillation, intracardiac EIT can also be used, which can be of two types: high and low energy •• When using high energy (200–400 J), one electrode is placed in the right atrium, the other - on the surface of the body. Efficiency up to 100% •• When using low energy 2–4.5 J, one electrode is placed in the right atrium, the other in the coronary sinus.
• Implantable cardioverter-defibrillators use low-energy cardioversion-defibrillation; they are used to treat paroxysmal ventricular tachycardia and recurrent VF, paroxysmal atrial fibrillation.
Indications for planned EIT • Intolerance to antiarrhythmic drugs • Lack of effect of drug antiarrhythmic therapy • Heart failure progressing due to tachyarrhythmia, symptoms of deterioration of blood supply to the heart, brain, peripheral circulatory disorders • Indication in the anamnesis of the positive effect of EIT in the treatment of tachyarrhythmias.
Contraindications to planned EIT • Intoxication with cardiac glycosides • Supraventricular tachyarrhythmias in thyrotoxicosis before correction of the level of thyroid hormones in the blood • Supraventricular tachyarrhythmias in patients with sick sinus syndrome or impaired AV conduction • EIT is not performed when thrombi are detected in the cavities of the heart during transthoracic or transesophageal Echo-CG • Hyperkalemia (possible development of bradyarrhythmia and asystole when the rhythm is restored).
Preparation for planned EIT • Transesophageal echocardiography is indicated for all patients before planned cardioversion to detect thrombosis of the left atrium • Cancellation of cardiac glycosides 3–4 days before the procedure • Normalization of electrolyte balance (EIT for hypokalemia is less effective and is more often complicated by VF) • If hypokalemia is detected, prescribe glucose-potassium mixture (10 ml 7.5% or 4 ml 20% potassium chloride solution) intravenously • Use of anticoagulants 2–3 weeks before EIT to prevent thromboembolism that occurs immediately after restoration of sinus rhythm in 2– 3% of patients with chronic atrial fibrillation.
Methods of pain relief during planned EIT • Mononarcosis with ketamine, propanidide or fast-acting barbiturates, as well as combinations of ketamine or narcotic analgesics with benzodiazepines. Kits for tracheal intubation and temporary pacemaker should be ready.
Complications of EIT • VF • Normalization embolism • AV block • Ventricular asystole • Vagotonic shock • Arterial hypotension • Pulmonary edema • Respiratory disorders • Skin burns.
Medicines after successful cardioversion • After relief of atrial fibrillation, anticoagulants for 2-3 weeks, especially if there is a history of thromboembolism, as well as with mitral heart disease, dilated cardiomyopathy, left ventricular failure; patients over 60 years of age.
Abbreviations. VF - ventricular fibrillation, EIT - electrical pulse therapy.