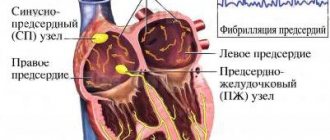
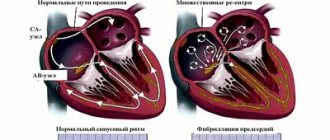
The essence of arrhythmia is similar to atrial fibrillation (AF), but with atrial flutter (AF), instead of chaotic waves, one or more stable paths of circular motion of the impulse arise in the atria. As a result, the atria contract more coordinatedly than in AF, and therefore rhythmic F waves similar in shape are recorded on the ECG.
It should be noted that atrial flutter (AFL), under certain circumstances, can progress to AF and vice versa. Sometimes it is impossible to distinguish them. In such cases, it is legitimate to give the conclusion: “atrial fibrillation-flutter.” But before going to extremes, you still need to try to differentiate one arrhythmia from another.
So, the main signs of atrial flutter are:
1. Absence of P waves.
2. The presence of a sawtooth wave F instead of P waves, better visible in leads V1 and V2.
In this case, the frequency of atrial contraction ranges from 200 to 400 per minute, that is, the distance between the ridges (FF) = 150 to 300 ms or, practically speaking, from 7.5 mm to 15 mm (at a belt speed of 50 mm/s).
Anything more than 400 beats per minute is atrial fibrillation, and anything less than 200 is supraventricular tachycardia.
Of course, TP also has other features in several different forms, which we will now consider in the practical part.
ECG No. 1
Pay attention to leads V1 and V2; instead of an isoline, F waves, similar to saw teeth, are clearly visualized in them. They move rhythmically at an interval of FF = 8.5 to small cells, that is, their frequency is about 350 per minute . Of course, under normal conditions * , the AV node is not able to transmit such a frequency to the ventricles, and therefore some of the waves are blocked. If there is one ventricular complex for every two waves, this flutter is called 2:1, if there are three waves, then 3:1, etc.
In this case, every fourth wave is carried out to the ventricles, that is, we are talking about a 4:1 flutter.
This is what a typical flutter looks like, and in this form its diagnosis is not difficult. But when the contraction frequency (AV conduction) increases, say 2:1, difficulties may arise. Look at ECG #2.
Basic principles of treatment
Modern therapy for arrhythmia is based on methods of restoring the heart rhythm to sinus and preventing new attacks of paroxysms with the prevention of thrombus formation. The provisions of the medical care protocol include the following items:
- antiarrhythmic drugs are used as medicinal cardioversion to normalize heart rhythm;
- beta-blockers are prescribed to control heart rate and the quality of contraction of the heart muscle (contraindication - patients who have a pacemaker implanted);
- anticoagulants prevent the formation of blood clots in the heart cavity and reduce the risk of stroke;
- metabolic drugs act as a stabilizer and improve metabolic processes;
- Electrical cardioversion is a method of electrical impulse relief of an attack of atrial fibrillation. To do this, atrial fibrillation is recorded on an ECG and defibrillation is performed under the control of vital signs. The only criterion for prohibiting such a procedure is severe bradycardia and persistent fibrillation for more than two years.
ECG No. 2
This is a typical flutter of 2:1 and 3:1, the F waves are poorly visible, but if you look, you can notice them (note that I separately highlighted the F wave in red . This is how the impulse passes through the atria, turn on your imagination and superimpose this segment on the main ECG and everything will become clear.
As you can see, the wave frequency is 375 per minute. Some alteration of the R waves is confused with irregularity, in which case it is probably not a big mistake to call it “atrial fibrillation-flutter”. But still, this is trembling.
Atrial flutter
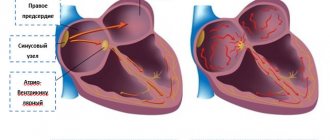
There are typical (classical) and atypical variants of atrial flutter. In the classic version of atrial flutter, the circulation of the excitation wave occurs in the right atrium in a typical circle; in this case, a flutter frequency of 240-340 per minute develops. Typical atrial flutter is isthmus-dependent, i.e., it can be stopped and restored to sinus rhythm using cryoablation, radiofrequency ablation, transesophageal pacing in the area of the cavo-tricuspid isthmus (isthmus) as the most vulnerable link of the macro-re-entry loop.
Depending on the direction of circulation of the excitation wave, two types of classic atrial flutter are distinguished: counterclockwise - the excitation wave circulates around the tricuspid valve counterclockwise (90% of cases) and clockwise - the excitation wave circulates in the macro-re-entry loop clockwise (10% of cases ).
Atypical (isthmus-independent) atrial flutter is characterized by the circulation of an excitation wave in the left or right atrium, but not in a typical circle, which is accompanied by the appearance of waves with a flutter frequency of 340–440 per minute. Taking into account the place of formation of the macro-re-entry circle, right atrial (multicycle and upper loop) and left atrial isthmus-independent atrial flutter are distinguished. Atypical atrial flutter cannot be treated with TEE due to the absence of a slow conduction zone.
From the point of view of the clinical course, a distinction is made between newly developed atrial flutter, paroxysmal, persistent and permanent forms. The paroxysmal form lasts less than 7 days and resolves on its own. The persistent form of atrial flutter lasts more than 7 days, and independent restoration of sinus rhythm is impossible. A permanent form of atrial flutter is said to occur if drug or electrical therapy does not bring the desired effect or is not carried out.
The pathogenetic significance of atrial flutter is determined by heart rate, on which the severity of clinical symptoms depends. Tachysystole leads to diastolic and then systolic contractile dysfunction of the left ventricular myocardium and the development of chronic heart failure. With atrial flutter, there is a decrease in coronary blood flow, which can reach 60%.
ECG No. 3
And here an unusual flutter is presented, the F waves are not at all similar to the usual saw, but their rhythm is clearly visible, the FF frequency is approximately 270 per minute, which clearly indicates atrial flutter (after all, with supraventricular tachycardia, the pulse frequency rarely exceeds even 200 per minute). As you can see, the F waves merge in some places with the T (F+T) and R (R+T) waves, deforming them.
* In the presence of additional conduction pathways, 1:1 conduction may occur, which will entail a high frequency of ventricular contractions, which they are not able to “withstand,” and ventricular flutter or fibrillation develops with all the ensuing consequences.
Now we complete the TASK. Good luck.
Types of atrial fibrillation and an example of a diagnosis
Clinically, atrial fibrillation manifests itself in several forms:
- paroxysmal, when an attack of fibrillation lasts no more than 48 hours in the case of successful treatment (cardioversion), or paroxysm is restored within 7 days;
- persistent - arrhythmia lasts more than a week, or fibrillation can be eliminated later than 48 hours with drug therapy and electrical stimulation;
- permanent form, when chronic fibrillation is not eliminated by cardioversion. Drug assistance in this case is ineffective.
Taking into account the heart rate data and signs of typical atrial fibrillation on the ECG, three variants of fibrillation are determined:
- normosystolic form - heart rate within 60-100 beats per minute;
- tachysystolic - heart rate more than 90 beats per minute;
- bradysystolic - heart rate less than 60 beats per minute.
The clinical diagnosis of the patient includes the characteristics of the arrhythmia and ECG data, which are deciphered: atrial fibrillation, persistent form, tachysystolic variant.
Symptoms
An attack of arrhythmia is manifested by rapid heartbeat. The patient feels pain in the chest, feels as if the heart is not working properly, experiences anxiety and even fear. His vision darkens, his head begins to spin, weakness appears, and shortness of breath develops.
Sometimes more severe clinical manifestations appear - low blood pressure, fainting.
In addition, signs of diseases that cause arrhythmia may worsen.
In rare cases, flutter is asymptomatic and is accidentally discovered during an examination due to the presence of another health problem.
Complications of the disease
In atrial fibrillation, the upper chambers of the heart are not fully filled with blood, causing reduced output and heart failure.
WPW syndrome with early excitation of the ventricles provokes the development of supraventricular arrhythmia, worsening the course of the disease and making it difficult to diagnose cardiac arrhythmias.
In addition to reducing the blood filling of the cavities of the heart, the chaotic contraction of the atria forms clots and thrombi, which, with the blood flow, enter the small and large vessels of the brain. Thromboembolism is dangerous due to complete closure of the arteriole and the development of ischemia, which requires resuscitation measures and initiation of treatment as soon as possible.
ECG 3
Bradysystolic form of atrial fibrillation. The f waves are not very clearly visible, but they are there. Alteration at low heart rate is also lost, but the absence of P and irregularity indicate atrial fibrillation.
Perhaps it can be noted that the most difficulties with interpretation may arise with the bradyform of AF. In such cases, you have to “try on” other arrhythmias on the ECG, and act “on the contrary” if they do not suit, AF remains.
Frequently asked questions about atrial flutter
How does atrial flutter manifest?
At first, the heart rate increases very quickly. There is discomfort in the chest, weakness, and a feeling of fatigue. It gets dark in the eyes. Sometimes shortness of breath occurs. Possible fainting.
In what cases does cardiac arrhythmia occur?
In 60% of cases, arrhythmia is accompanied by hypertension or coronary heart disease. But non-cardiac diseases and conditions can also cause the disorder, for example, hyperthyroidism, electrolyte imbalance, hypoxia, use of alcohol or psychostimulant substances and medications.
Why is atrial flutter dangerous?
If left untreated, arrhythmia can lead to heart failure, ischemic stroke and acute respiratory failure, which can be fatal.
Treatment tactics
- Drug therapy is the prescription of special drugs to relieve attacks of arrhythmia and prevent their occurrence.
- Radiofrequency ablation is a minimally invasive surgical treatment for cardiac arrhythmias. The procedure begins with constructing an electrical model of the atrium and determining the localization of sources of pathological excitation. During the intervention, a catheter is inserted through the patient's femoral vein into the atrium cavity. Electrical isolation of the pulmonary veins is then performed using catheter radiofrequency lesions. The procedure is performed under local anesthesia and takes about two hours.
Radiofrequency ablation (RFA)
When a person has an abnormal pulse and develops arrhythmia as a result of a number of cardiovascular diseases, he needs to undergo a comprehensive examination. Doctors often recommend using the catheter ablation method, that is, RFA of the heart. They made this choice largely due to the wide list of advantages of the technique with a minimum number of disadvantages. Therefore, this heart operation is considered one of the best.
It involves neutralizing cells that cause rhythm disturbances with electric current. The latter's access to the heart is provided by a catheter. The operation is not surgical and is considered minimally invasive. It is performed under local anesthesia.
The source of arrhythmia is destroyed using high-frequency (or radio frequency) current of 400-500 kHz.
Causes
The immediate cause of this form of arrhythmia is a violation of the conduction of electrical impulses through the atrium. The atria often contract, which is why not all impulses reach the ventricles. In 30% of cases, this is observed with damage to the coronary arteries of the heart (coronary artery disease), and in another 30% with hypertension. Rare cardiac factors are congenital and rheumatic heart defects, cardiomyopathy, mitral valve prolapse, pericarditis, acute myocardial infarction.
In other cases, people with arrhythmia do not have heart disease. Other possible causes and risk factors:
- hyperthyroidism;
- chronic lung diseases, such as obstructive disease or pulmonary emphysema;
- adrenal tumor;
- reduced oxygen content in the body;
- obesity;
- alcohol abuse;
- imbalance of electrolytes, including due to diseases of the digestive tract, malnutrition, dehydration, overdose of diuretics;
- treatment with digitalis glycosides;
- use of psychostimulants, including drugs and certain medications;
- surgical interventions.
Ongoing research
The following methods are used to diagnose atrial flutter:
- ECG - allows you to record the type of rhythm disturbances
- Daily (Holter) ECG monitoring allows you to estimate the pulse rate at different times of the day, incl. during sleep, record paroxysms, if any
- EchoCG - ultrasound of the heart - allows you to assess the size of the heart chambers, myocardial contractility, the condition of the heart valves (they also affect arrhythmia)
- Blood tests can reveal a lack of electrolytes (potassium), dysfunction of the thyroid gland (increased levels of thyroid hormones), signs of acute rheumatism or myocarditis
- Sometimes there is a need to conduct an electrophysiological study (EPS) of the heart
to the top of the page
History of the development of ideas about atrial flutter
IN 1918
Mr.
T. Lewis
suggested the focal theory of atrial fibrillation, which assumed the formation of a high-frequency electrically active focus in the atria.
However, already in 1925
d. This author changes his ideas and speaks out in favor of intraatrial re-entry as a substrate of AFL.
The theoretical concept of TP has undergone changes in subsequent years from the original focal theory to the electrical excitation reentry theory:
— 1947
g. -
A. Rosenblueth
and
Garcia-Ramos,
in a surgical experiment, accidentally expanded the incision between the inferior and superior vena cava into the area of the free wall of the RA. The result was the manifestation of TP, the mapping of the cycle of which revealed the circulation of a re-entry wave along the perimeter of the cut being performed.
— 1949
g. -
D. Scherf
developed the focal theory of TP.
— 1954
Mr. -
E. Kimura
also put forward the focal theory.
— 1986
g. -
L. Frame
postulated re-entry as the initiating mechanism of TP.
L.Frame
performed the so-called Y-shaped incision, shown in Figure 5, and for the first time verified the topographic separation of the atrial incision from the area of re-entry wave circulation underlying AFL.
— 1982-1984
gg.
— M. Allessie,
based on the use of the acetylcholine model, speaks in favor of the re-entry mechanism underlying TP.
— 1981-1988
gg.
— P. Boyden
creates a model of tricuspid regurgitation and a model of pulmonary artery clipping. Evidence for the nature of re-entry TP.
— 1986
g. —
A. Waldo,
based on a sterile pericardial model, verifies re-entry as the leading mechanism of TP.
— 1991
g. -
J. Cox
, using the model of mitral regurgitation, advocates the re-entry theory underlying TP.
The evolution of clinical ideas about the nature of TP is similar:
— 1951
g. -
M. Prinzmetal,
based on the use of photographic technology, spoke in favor of the focal nature of TP.
— 1971
g. -
H.Wellens
, using the epicardial mapping method, confirms the position about the focal nature of AFL.
— 1986-1990
gg.
— F. Cosio
and
B. Olshansky
verify re-entry as the basis of TP.
Thus, the 90-year journey from the focal theory to the idea of re-entry has taken place.
Cardiac resynchronization therapy
Bipolar pacemaker in the treatment of heart failure
Look
indications, use in clinical practice