home
Articles
Health
Kurilova Alina Petrovna
Pediatrician
14.05.2019
Before you start taking antipyretics, you need to answer a few questions:
- what age is the child?
- How does a child tolerate an increase in temperature?
- Is there a family or child history of febrile seizures?
- Are there any other symptoms of the disease besides fever?
Increased temperature or fever
is a protective-adaptive reaction of the body in response to the influence of pathogenic stimuli, as a result of which a restructuring of thermoregulation processes occurs, leading to an increase in body temperature, which stimulates the natural resistance of the body.
An increase in temperature affects the child’s body both positively and negatively.
Positive influence
is that when the temperature rises in the child’s body, the immune system is activated, phagocytosis increases, the production of antibodies increases and the level of interferon increases, which helps to stop the proliferation of pathogenic microorganisms and overcome infection.
Bad influence
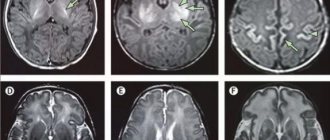
high temperature on a child manifests itself in the occurrence of convulsions (febrile), increased load on the baby’s cardiopulmonary system (heart rate and breathing rate increase). Therefore, fever is dangerous for children with developmental defects of the heart and bronchopulmonary system, and heart rhythm disturbances. Also, when the temperature rises, the functioning of the brain, liver, stomach, kidneys and other internal organs suffers, which is dangerous for children with chronic pathologies of internal organs, symptoms of dehydration, developmental disorders and diseases of the nervous system.
Fever varies:
- with the flow:
- acute (fever up to 2 weeks),
- subacute (up to 6 weeks),
- chronic (over 6 weeks).
- according to the degree of increase in the indicator:
- subfebrile (increase to +38.0 degrees)
- febrile (from +38.0 to +39.0 degrees),
- pyretic (from + 39.0 to +41.0 degrees),
- hyperpyretic (over +41.0 degrees).
- by type of temperature curve:
- constant (temperature fluctuations during the day do not exceed 1 degree).
- laxative (daily fluctuations up to 2 degrees),
- atypical (oscillations are chaotic, varied and irregular),
- debilitating (a combination of laxative and atypical fever with fluctuations during the day of more than 2-3 degrees),
- intermittent (a combination of short-term periods of increase and decrease in temperature to normal values),
- recurrent (alternating periods of temperature increase with periods of temperature normalization from 2 to 7 days).
According to the recommendation of the WHO (World Health Organization), antipyretic drugs are prescribed to children according to age:
- from birth to 2 months at a temperature of +38.0 degrees,
- children from 3 months to 24 months with a temperature of +38.5 degrees,
- children from 1 to 5 years old with a temperature of +39.0 degrees,
- children over 5 years old at + 39.5- +40.0 degrees.
Symptoms of changes in heart rate
Mild to moderate changes in heart rate do not always bother the child. His condition can be satisfactory both in the case of a physiological slowdown or increase in heart rate, and in the case of pathology. Often the appearance of bradycardia is detected on the ECG and is very surprising to parents.
Symptoms indicate that the child needs urgent diagnosis and treatment. Bradycardia is expressed in general weakness, fatigue, drowsiness, dizziness, sweating, and loss of consciousness. Sometimes accompanied by unstable blood pressure readings.
Tachycardia may be accompanied by interruptions and “failures” in the functioning of the heart. The child feels dizzy, sometimes loses consciousness or complains of darkening of the eyes.
In some cases, there is chest pain.
Young children cannot express their discomfort in words. Therefore, parents should always be attentive to the well-being of the child. Lethargy, drowsiness and calmness of the baby may be a sign of a heart rate disorder. If an older child notices any symptoms, then his pulse should be measured.
The athlete's heart rate should recover soon after completing the exercises. If this does not happen, then this is a reason to visit a cardiologist.
On the other hand, the approach to each child should be individual.
If the child
- restless or feeling weak
- cannot tolerate muscle pain, headaches,
- there is nausea,
- no appetite,
then you must first use physical methods to improve the child’s well-being
:
- put to bed - this way the body will retain strength to fight infection and calm the child;
- drink fractionally with water or sweetened warm herbal tea with chamomile, linden, cranberry juice;
- provide access to fresh air;
- If there is an appetite, feed small portions of warm food (for example, soup, thin porridge with water, a light breakfast).
Also, according to the clinical course of the fever, apply additional cooling measures.
For “red” or “pink” fever
- the baby's body feels hot to the touch,
- skin is red or pink, moist,
- The child himself does not complain about his health, is active, and does not lose his appetite.
In this case, the child must
- undress,
- wipe with a towel soaked in water at room temperature,
- apply a cool compress to your forehead,
- drink water at room temperature
- and be sure to call a doctor.
For "white or pale" fever
- the child’s limbs and body feel cold to the touch,
- lips and nail beds take on a bluish tint,
- skin is pale and dry,
- There is a disturbance in well-being: the child is lethargic, delirium is possible.
In this case, the child must
- warm by rubbing the limbs with your hands or using warm water (other means are prohibited!),
- put on socks
- cover with a blanket
- and drink warm tea or water.
The use of antipyretics for such symptoms is ineffective - you need to urgently call a doctor!
The exception is children at risk, whose temperature is reduced above 37.1 degrees. These are kids,
- having diseases of the nervous system,
- experiencing convulsions due to a rise in temperature,
- those suffering from chronic diseases of the circulatory system, respiratory system or hereditary metabolic diseases and other risks (overheating, symptoms of dehydration, etc.).
Febrile seizures are diagnosed more often in children under 6 years of age with temperatures above +38 degrees, as well as in children with pathologies of the nervous system at any temperature. It is recommended for such children to reduce their temperature to febrile levels (not higher than +38.0) or to those values recommended by a neurologist.
Usually, against the background of an increase in temperature, the child’s heartbeat and breathing rate increase: the respiratory rate increases by 4 respiratory movements for every degree above +37.0 degrees, and the pulse rate increases by 20 beats per minute for every degree. However, against the background of diseases of the cardiovascular system and respiratory organs, such as developmental defects or heart rhythm disturbances, inappropriate increases or decreases in pulse and breathing are possible. Such children, on the recommendation of a cardiologist and pulmonologist, are prescribed antipyretics up to febrile levels (i.e., not higher than +38.0 degrees).
Children with hereditary metabolic diseases (diseases of the thyroid gland, kidneys, liver, disorders of the immune system and others) and children with imperfect compensatory mechanisms of thermoregulation during fever (these are some children from birth to 2 months) are also prescribed antipyretics on the recommendation of related specialists funds up to febrile numbers.
Overheating - an increase in body temperature due to additional exposure to heat
- prolonged exposure to the sun,
- wearing too much clothing
- excessively wrapping children).
The risk of overheating is associated with the risk of heat stroke. It manifests itself
- not only at elevated temperatures,
- but also in impaired consciousness, convulsions,
- disorders of the heart and breathing.
First aid is to call the ambulance team “112”.
Before the doctor arrives
- undress the child
- move to a cool place or shade,
- provide access to fresh air or blowing with a fan (but not cooled air!),
- apply a cold compress to your forehead,
- wipe the body with cool water or wrap it in a sheet moistened with cool water.
Antipyretic therapy for children should be prescribed strictly individually, taking into account clinical and anamnestic data.
Tachycardia in children
30.09.2021
Probably, every parent has more than once noticed an increased heart rate in their child, which arose against the background of emotional stress, intense physical activity or elevated temperature. It is important to investigate the cause of the formation of tachycardia , whether it arose as a result of pathological changes or whether its occurrence is physiological and there is no reason for concern.
The word "tachycardia" is translated from Greek as "fast" and "heart", in other words the heart rate is excessively increased. In children, heart rate varies and depends on the age group.
If the heart is functioning properly, then its work is usually not felt, but if it begins to contract at an accelerated rate, the child notices symptoms such as weakness, rapid heartbeat, and tinnitus . Such unnatural rapid contraction of the heart is called tachycardia .
Types of tachycardia. Symptoms and treatment
There are 3 types of childhood tachycardia : sinus; paroxysmal; chronic.
- Sinus tachycardia . With this type of tachycardia, the activity of the sinus node increases, as a result of which the heart rhythm changes. This form of tachycardia can occur as a result of excessive physical activity or due to disturbances in the functioning of the heart . Sinus tachycardia can be both physiological and pathological. Physiological appears with vegetative-vascular dystonia at a time when the child begins to actively grow. Pathological tachycardia occurs due to organic damage to the heart . The main difference between sinus tachycardia in children is that it usually comes and goes gradually. In children, the symptoms are mild and manifest themselves in rapid heartbeat. In order to cure sinus tachycardia it is enough to eliminate the causes of its occurrence.
- Paroxysmal tachycardia is an attack of heartbeat with a frequency of 180-200 beats per minute, suddenly starting and also stopping unexpectedly. During such an attack, the child becomes frightened; he may also be bothered by weakness, abdominal pain , shortness of breath, cyanosis, and sweating. Paroxysmal tachycardia in children is divided into supraventricular (occurs in case of abnormalities in the regulation of the heart ) and ventricular (children get sick in rare cases, but the disease has a disappointing prognosis, especially in infants). to stop supraventricular tachycardia by reflex: hold your breath, squeeze your abdominals, induce vomiting, strain as hard as you can, press on the eyeballs. Cardiac glycosides are used for treatment, and after the attack has stopped, therapy is continued with maintenance medications.
- Chronic tachycardia in children is manifested by chest , low blood pressure, and asphyxia. The attacks are often accompanied by loss of consciousness or convulsions. This type of tachycardia occurs due to congenital heart in a child. Treatment of the chronic form consists of changing lifestyle: following a daily routine; adhere to a healthy diet enriched with vitamins and microelements; perform hardening. It is also important to protect the child from stress and intense physical activity.
Left unattended, tachycardia can cause heart failure. Therefore, it is necessary to carefully monitor your child’s health and pay close attention to his complaints of malaise. If you suspect any disease, you should immediately consult a doctor .
Published in Cardiology Premium Clinic
Our heartbeat has its own rhythm that keeps the heart healthy and functioning properly. Abnormal heart rhythm is not uncommon in children, but sometimes it can be a serious condition.
What is the normal heart rate in children?
The heart rate of a child is different from that of an adult. Typically, children's average heart rate is 60 beats per minute when they are resting, while it can reach 220 beats per minute when they are active. Infants have a higher heart rate than children.
The "normal" average heart rate for children depends on their age group.
Below are the average resting heart rates (pulse rates) for children of different age groups.
Average heart rate at rest (beats per minute):
- From 3 to 4 years - between 80 and 120
- From 5 to 6 years - between 75 and 115
- From 7 to 9 years - between 70 and 110
- From 10 years and older - between 60 and 100
Heart rate depends on the child's age and activity level.
When and how to check a child's pulse?
If your baby has health problems that require regular monitoring of his heart rate, he will have to learn how to check his pulse.
Parents should also check their baby's heartbeat if they:
- Complains of rapid heartbeat
- Feels chest pain
- Suddenly has trouble breathing (not caused by asthma)
- Lips or skin suddenly turn pale gray or blue
An accurate pulse reading is essential to determine if your child is experiencing abnormal heart rhythms.
How to measure a child's pulse?
1. Find out the pulse points - or the places where the artery is close to the skin. The neck and wrist are the two places where the arteries are closest to the skin. You can also check the pulse behind your knees, on the top of your feet, in your groin, at your elbow when your arm is extended, and at your temple.
2. The child should have rested for at least 10 minutes before you checked the pulse.
3. Ask your child to extend his or her arm, palm up. Place your index and middle fingers together on your wrist. You will feel the impact.
4. Use a watch or timer to count the beats pulsing on your hand.
5. Count the number of beats in 15 seconds. To get your heart rate, multiply the number of beats recorded in 15 seconds by 4. For example, if you counted 20 beats in 15 seconds, your heart rate per minute would be 100.
In some people, the thumb may also have a pulse, so avoid using it to check your pulse rate.
The doctor will also check the quality or strength of your pulse to see if it is regular or erratic.
Irregular heartbeat (arrhythmia) in children
When a child is physically active, their heart rate is usually lower, and when they are resting, their heart rate is lower. Likewise, your heart rate can increase significantly during strenuous exercise. But when the rhythm or heart rate changes suddenly without any physiological trigger, it is not normal. This condition is called arrhythmia or irregular heartbeat and may indicate heart problems or other underlying conditions.
Heart palpitations may be accompanied by palpitations (noticeable sudden, hard palpitations), dizziness, and sometimes fainting.
Symptoms of Abnormal Heart Rhythm in Children
Arrhythmia can occur at any age. There are few or no symptoms, so self-diagnosis can be difficult.
Signs and symptoms that may be noticed:
- fast or slow heartbeat;
- dizziness;
- weakness or fatigue;
- chest pain.
The heart must follow a certain rhythm in order to function normally over a long period of time. If this does not happen, biological processes may become disrupted and lead to potential health risks in the future.
Types of arrhythmia
There are many types of arrhythmias that a child can develop. While most of them are not dangerous, some are serious conditions that require ongoing medical attention.
- Tachycardia
With tachycardia, the heart beats too quickly. An adolescent is considered to have tachycardia if the resting heart rate exceeds 90 beats per minute, while tachycardia in children is a condition in which the heart rate may exceed 100 beats per minute. However, since a child's normal average heart rate is usually 100 or more, it may or may not be considered a tachycardia depending on the child's age.
Causes of tachycardia in children may include physiological changes, medications, and any other form of arrhythmia. Sometimes an underlying heart condition can also cause a child's heart rate to increase.
There are three known types of tachycardia:
- Sinus tachycardia is a natural increase in a child's heart rate. The sinus node, which is also known as the heart's pacemaker, is responsible for sending electrical impulses throughout the body that cause the heart muscles to expand and contract, thereby creating a steady heartbeat rhythm. The sinus node sends faster impulses when metabolic activity is high and slows down when the body is at rest (sleep). Thus, in most cases, sinus tachycardia is a natural phenomenon caused by changes in activity levels, and this abnormality leads to sinus arrhythmia in children.
- Supraventricular tachycardia is one of the most common types of tachycardia in children. It does not cause life-threatening problems in most children and adolescents. However, if the tachycardia is frequent, your doctor may prescribe medications to control the condition.
- Ventricular tachycardia is a condition where a child's rapid heartbeat is caused by the lower chambers or ventricles of the heart. Although this type of tachycardia is rare, it can be serious and sometimes life-threatening in children.
Wolff-Parkinson-White syndrome is the presence of an extra pathway in the heart's electrical system that causes rapid heartbeat, dizziness, and shortness of breath. A doctor can treat this heartbeat abnormality with medications.
- Bradycardia
Bradycardia is the opposite of tachycardia. When the heart rate is too low, say less than 60 to 50 beats per minute, the baby is more likely to have bradycardia. However, before diagnosing this condition, the doctor will take into account age, activity level.
Other heart rhythm problems in children include complete heart block and sick sinus syndrome.
Who is at risk for developing arrhythmia?
Arrhythmia is more common in children with congenital heart defects, narrow heart valves, a family history of arrhythmia, and other heart conditions. In adolescence, arrhythmia can be caused by drinking alcohol and smoking.
Diseases such as obesity, diabetes, sepsis, sleep apnea, etc. may also increase the risk of developing arrhythmias.
Additionally, irregular heart rhythms in children may be caused by heart surgery, medications, or an imbalance of certain chemicals, such as potassium, in the body.
When should you see a doctor?
Often, an arrhythmia, or abnormal heart rhythm, is the result of changes in physical activity, making it common in children. However, if the pulse is too fast or slow, regardless of physical activity, and if it occurs frequently, a medical examination is necessary.
Treatment of arrhythmia in children
As a treatment, the child may be prescribed:
- Cardiac catheterization using radiofrequency energy
- Use of implantable devices such as pacemakers and implantable cardioverter defibrillator
- Cardioversion, which involves sending an electrical shock or impulses to the heart to convert erratic heartbeats into a regular rhythm
- Surgery to treat atrial fibrillation
References:
- Pulse; Medline Plus; US National Library of Medicine
- Dianne Pickering; How to measure the pulse; Community Eye Health Journal
- Fast Heart Rate; C. S. Mott Children's Hospital
- Arrhythmia; Medline Plus; US National Library of Medicine
- Types of Arrhythmia in Children; American Heart Association
- Ventricular Tachycardia; C. S. Mott Children's Hospital
- Ajay Dharod, et al.; Association of Asymptomatic Bradycardia With Incident Cardiovascular Disease and Mortality; Jama Internal Medicine
- Sick sinus syndrome; C. S. Mott Children's Hospital
- Arrhythmia; National Heart, Lung, and Blood Institute
Heart rate norms
In the fetus
You can notice fluctuations in the baby’s heart at the beginning of the first trimester; the rhythm is rapid and changes with the development of the fetus. Pulse at 6–8 weeks is 110–130 beats, from 8 to 11 it reaches 190, from 11 weeks – 140–160, varies several times a day.
In newborns
- The heart rate of a baby (the first 4 weeks after birth) with anxiety increases to 160–200 beats.
- 120–140 beats is normal.
- Children born prematurely have a higher heart rate than a child born at full term.
In infants
A baby is considered a child from 30 days to 1 year. By the age of one year, the baby’s normal heart rate is 132 beats. Normally, the heart rate in children increases to 162.
In young years
In a child under 7 years of age, the nervous system is at a stage of intensive development, which is the reason for the increase in heart rate in children. For a 2-year-old child, the normal heart rate is 124 beats; physical activity or stress leads to a frequency of 94 to 154 beats.
In preschoolers
The age of preschoolers is conventionally divided into three periods:
- junior preschool age - from 3 to 4 years;
- average preschool age - from 4 to 5 years;
- senior preschool age - from 6 to 7 years.
The normal pulse rate for 6-year-old children, as can be seen from the table, is 106 beats.
The heart rate of school-age children is 80–120 beats.
In children 9–10 years old, the normal heart rate is considered to be 108 beats per minute.
- Fetal heart rate at different stages of pregnancy, table of indicators