Risk factors
There are also numerous risk factors for the development of cerebral ischemia in newborns, among which neurologists and obstetrician gynecologists note:
- first pregnancy over 35 years of age or under 18;
- long-term infertility therapy;
- insufficient body weight of the newborn (less than 1.5-1.7 kg);
- premature birth (before the 37th week of pregnancy) or post-term pregnancy (more than 42 weeks);
- spontaneous rupture of membranes;
- too long or rapid labor;
- incorrect presentation of the fetus;
- umbilical cord vasa previa (vasa previa), most often observed during in vitro fertilization;
- injuries to the baby’s skull during childbirth (as a result of obstetric errors);
- emergency caesarean section;
- heavy bleeding during childbirth;
- the presence of cardiovascular or autoimmune diseases in the pregnant woman, anemia, diabetes mellitus, functional disorders of the thyroid gland, blood clotting disorders (thrombophilia), antiphospholipid syndrome, infectious and inflammatory diseases of the pelvic organs;
- severe arterial hypotension during pregnancy and late gestosis.
Risk factors for cerebral ischemia in infants are also recognized as congenital blood pathologies associated with mutations in the prothrombin genes, platelet coagulation factors V and VIII, plasma homocysteine, as well as disseminated intravascular coagulation syndrome and polycythemia.
[23], [24], [25], [26], [27], [28], [29]
How complications are treated
Encephalopathic manifestations of severe and moderate forms often result in persistent brain symptoms. It may manifest itself mildly or the baby may become disabled. With any prognosis of encephalopathic changes, there are restrictions on the use of medications:
- Antiepileptic drugs for seizures.
- Muscle relaxants for severe cerebral palsy.
In order for a baby with ischemic complications to develop correctly, you need to regularly work with him:
- If a child has cerebral palsy, then he needs a special massage technique, which should be performed by a specialist at least in the early stages.
- Older children require exercise therapy.
- Special mechanisms are needed to adjust the correct posture. With spastic changes due to incorrect position, they intensify, which will lead to an unfavorable outcome. With the help of strollers, splints, bolsters, and special chairs, the most acceptable, physiological position of the body is ensured.
- The speech therapist will correct the baby’s speech, teach him to be attentive and assiduous.
Complications and consequences
The development of cerebral ischemia in newborns causes oxygen deficiency-induced damage to its cells and causes very serious, often irreversible neurological consequences and complications that are correlated with the topography of the lesions.
Studies have shown that cerebral ischemia in newborns is more susceptible to pyramidal cells of the hippocampus, Purkinje cells in the cerebellum, reticular neurons of the perirolandic region of the cerebral cortex and the ventrolateral part of the thalamus, cells of the basal ganglia, nerve fibers of the corticospinal tract, midbrain nuclei, as well as neurons of the neocortex and brainstem brain
In full-term newborns, the cerebral cortex and deep nuclei are primarily affected; in premature newborns, diffuse destruction of the white matter cells of the hemispheres is noted, which causes chronic disability in surviving children.
And with global ischemia of brain stem cells (in which the centers for regulating respiration and heart function are concentrated), their total death and almost inevitable death occurs.
Negative consequences and complications of perinatal and neonatal cerebral ischemia of 2-3 degrees in young children are manifested by epilepsy, unilateral vision loss, delayed psychomotor development, motor and cognitive disorders, including cerebral palsy. In many cases, their severity can be fully assessed by the child’s age of three.
- Cerebral ischemia grade 1 in a newborn - causes, symptoms and treatment
[45], [46]
Hypoxic-ischemic encephalopathy in children
A neurological examination of a newborn child should begin with the standardization of examination conditions, since inadequate room temperature and the nature of lighting affect the resulting reflexes, reactions, etc. The examination is carried out at the optimal room temperature of about 24-26 ° C after 1-2 minutes of adaptation of the child in the unfolded position. form under a radiant heat source. At low temperatures, it is more likely to get a reaction of increased muscle tone and tremor, at high temperatures - muscle hypotension. Lighting should be symmetrical in relation to the newborn, since light incident on one side causes a narrowing of the pupil and palpebral fissure on the side of illumination. During examination, it is necessary that the child’s head is in the sagittal plane, since due to the asymmetric cervical-tonic reflex, a decrease in muscle tone is noted on the side of the head rotation, and an increase on the opposite side.
It is also necessary to take into account the time that has passed since the last feeding, since after saturation the baby is relaxed, he may have reduced muscle tone and a number of reflexes and reactions, and before feeding the newborn may be in a state of relative hypoglycemia, leading to restlessness, tremors and increased muscle soreness. tone.
Next, it is advisable to determine the state in which the newborn is, since the same indicators of reflexes and reactions can be physiological for one state of the child and pathological for another.
The sociability of a newborn as the main indicator of general activity is assessed by the reaction of displeasure in the presence of discomfort (forced awakening, hunger, wet diapers, etc.) and the speed of calming when eliminating irritating factors, as well as by the response to positive stimuli (response to affectionate speech, stroking, picking up).
The interaction between the child and the doctor is essential in determining the communication skills and behavior of a newborn, and therefore the role of not only the newborn’s reactions is important, but also the doctor’s persistence in receiving them, his positivity towards the child during examination. To assess a child’s sociability, the difference in auditory and visual reactions to animate (the doctor’s face and voice) and inanimate (artificial and natural light sources, rattle, bell, clap) stimuli is important. The presence of search, palm-oral, grasping reflexes and the Babinsky reflex indicates the presence of tactile sensitivity. Pricking a child with a needle causes frowning of the eyebrows, clenching of the eyes, wrinkling of the nasolabial furrow, opening of the mouth, pouting of the lips, stretching of the mouth, tension of the tongue, trembling of the chin, screaming, as well as a motor reaction: flexion with adduction of the limbs. A painful reaction occurs a few seconds after the application of irritation, which is due to slow conduction through the nerves of the newborn due to insufficient myelination.
A decrease in the listed reactions may be either a sign of depression of the central nervous system as a result of a number of somatic and neurological diseases, or damage to the corresponding analyzer. Thus, lack of response to pain may be a consequence of hereditary sensory polyneuropathy.
Among the signs of the child’s general activity, spontaneous motor activity should be noted. Its assessment is quite subjective and depends on the doctor’s experience, but objectification is possible only by analyzing a video recording of activity for 1 hour. Typically, spontaneous movements consist of periodic flexion and extension of the legs, their crossing, pushing away from the support; movements of the hands at chest level in the elbow and wrist joints with clenching of fists. The presence of a choreoathetoid component in movements, which is physiological for newborns, indicates the predominance of extrapyramidal (striatal) motility and consists in restlessness of the tongue, spreading and independent movements of the fingers.
The facial expressions of a newborn are quite rich and, as a rule, symmetrical and consist of squeezing the eyes, frowning the forehead, deepening the nasolabial folds, tense the tongue, and open the mouth. Facial asymmetry is possible on the first day due to the peculiarities of the passage of the baby’s head through the birth canal. On the other hand, facial asymmetry may be due to damage to the cranial innervation.
The doctor studies the child’s pupils, the movement of the eyeball, the state of the palpebral fissure, etc., the symmetry of mouth opening when yawning and screaming, swallowing, screaming, and the muscles of the tongue.
It should be noted that tremor as a periodic oscillation around a fixed axis of a certain amplitude and frequency occurs in almost half of newborns. Low-amplitude, high-frequency tremor when a newborn is crying or excited, as well as in some stages of sleep, is a physiological phenomenon. In terms of prevalence, tremor can affect the chin, tongue, and limbs.
Muscle tone is the most important characteristic of the motor activity of a newborn. We can talk about the child’s active muscle tone (posture) and passive, the value of which is determined by checking mobility in the joints. A healthy full-term baby has a so-called fetal position due to a flexor increase in tone (arms are bent in all joints, brought to the body and pressed to the chest, hands are clenched into fists, the thumbs of the hands lie under the other four; legs are bent at the joints and abducted in hips, dorsiflexion predominates in the feet). In some cases, a predominant physiological increase in muscle tone in the arms compared to the legs and neck extension are noted. The active muscle tone of the newborn can also be judged by holding the baby in the air face down, with the baby's head in line with the body, the baby's arms slightly bent and legs extended. “Sinking” of the child’s head when he is pulled up by the shoulder girdle (symptom of “flaccid shoulders”) in full-term newborns occurs both with hypoxic parasagittal lesions of the brain and with injury to the cervical spinal cord.
The assessment of reflex activity is carried out on the basis of at least three tests of this reflex. If the reflex amplitude is maintained in all three tests or the amplitude decreases slightly in the third, the reflex is considered normal; if the initial amplitude value is low, persists in three tests or progressively decreases with repeated testing of the reflex, and also if repeated stimulation is necessary to obtain the reflex, it is considered reduced.
Testing of abdominal and cremasteric reflexes is of limited value in neonatology due to their variability in detection and severity.
Of particular importance is checking the reflexes of newborns (“primary”, “unconditioned” reflexes). Most of the reflexes of newborns reflect the evolutionary maturity of the child, his functional state, and only some of them have a specific topical significance. Due to their large number, it is necessary to focus on the most informative ones. When stroking the baby's skin in the area of the corner of the mouth, the head turns towards the stimulus (search reflex), when a finger lightly touches the newborn's lips, the lips stretch (proboscis reflex), and when a pacifier is placed in the mouth, sucking movements occur (sucking reflex). When pressing on the thenar area, the child opens his mouth, tilts his head, bends his shoulders and forearms (Babkin's palmar-oral reflex), when placing fingers in the newborn's hand, the researcher's fingers are grasped (upper grasp reflex), and if the child can be lifted, the Robinson reflex occurs. When the skin of the back along the spine is irritated, the newborn bends the torso in an arc open towards the irritation (Galant reflex). A child raised under the armpits bends his legs in all joints, and when placed on a support, he stands on half-bent legs (support reflex); when bending forward, the child makes stepping movements (stepping reflex), while crossing his legs in the lower third of the lower leg is possible. In the position of the child on his stomach, when the researcher’s palms are applied to his feet, a reflex repulsion and crawling occurs (Bauer reflex). When pressing on the ball of the foot in the area of the II-III toe, plantar flexion occurs (inferior grasping reflex of Verkom), and when the sole is irritated by strokes, its extension and fan-shaped divergence of the toes occurs (Babinsky reflex).
It should be noted that a dynamic study of the state of the nervous system of healthy newborns indicates the presence of transient physiological changes in the neurological status of the child in almost half of the children. Therefore, to classify a particular deviation in the neurological status of a newborn as physiological or pathological, it is necessary to evaluate it in connection with other phenomena, dynamic observation, and in some cases the use of adequate additional research methods.
The neurological status of the newborn can be normal or deviant, and among the options for the latter, one of the following neurological syndromes is noted: increased excitability, muscle hypertension or hypotension, apathy, hemisyndrome; or their combinations. In Russia, the most common classification of lesions of the nervous system in newborns and young children is Yu. A. Yakunin et al. Within the framework of this classification, hypoxic encephalopathy is considered as a particular manifestation of the pathology of the nervous system of this period. In the classification of Yu. A. Yakunin et al. consider the periods of action of the harmful factor: prenatal (embryonic, early fetal) and perinatal (antenatal or late fetal, intranatal and neonatal). The dominant factors, in addition to hypoxia, include trauma, infection, intoxication, inborn errors of metabolism, chromosomal aberrations, unspecified and unclassified conditions. According to the severity, encephalopathy can be mild, moderate, or severe. Among the levels of damage are the meninges, cerebral cortex, subcortical structures, trunk, spinal cord, peripheral nerves, combined forms.
-th degree
In this case, there is an implicit appearance of neurological disorders. With grade 1 cerebral ischemia, patients note the appearance of:
- Headaches.
- General weakness, which gradually develops into severe fatigue.
- Decreased concentration.
- Frequent insomnia.
- Memory impairment.
- Emotional instability.
However, these symptoms are not specific. Because of this, it is very difficult to timely diagnose the appearance of grade 1 cerebral ischemia. Many people associate all these symptoms with overwork, so they rarely seek medical help. However, you need to understand that this stage of pathology is amenable to the fastest and most effective treatment.
Cerebral ischemia in newborns
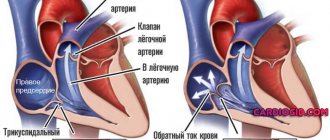
CEREBRAL ISCHEMIA is a diagnosis that doctors can make to newborn babies in the maternity hospital. It occurs due to insufficient oxygen supply to brain cells. The reason contributing to this deficiency can appear both during the mother’s pregnancy and during the birth of the child.
One of the first tests that doctors use immediately after the birth of a baby is the well-known Apgar score. The number of points determines the condition of the baby. The lower the score, the more severe the child’s condition, the greater the likelihood of this diagnosis. Doctors use the diagnosis of cerebral ischemia of newborns in the first month of a child’s life and divide the pathology into three degrees according to severity. The child's treatment depends on the severity.
The mildest is grade 1; as a rule, there are mild neurological symptoms, for example, in the form of increased excitability of the child, and the baby does not require hospital treatment. But in the case of the second, especially third degree, the issue of hospitalization of the baby in a specialized department of the hospital is decided. The first month is an acute condition. From the second month of life until the age of 1 year, there is a period of recovery of the nervous system affected by ischemia, and the neurologist, in diagnosing hypoxic-ischemic damage to the central nervous system, identifies the leading syndromes and selects treatment in accordance with this. One of the severe consequences of cerebral ischemia is cerebral palsy, which makes the child disabled from childhood.
During this second period of time, parental involvement in the restorative treatment process will be very important. Observation by a neurologist is necessary, and additional ultrasound examinations of the brain are required. Based on the results of the examination and research, the neurologist may refer you and your child to an appointment with an osteopath, and may also prescribe a course of medications. Most often, these drugs are from the group of vascular, nootropic drugs, as well as from the group of vitamins or diuretics. In some difficult cases, children need to be readmitted to the hospital to receive anticonvulsant therapy, intramuscular injections and drips.
What is required from parents?
Firstly, it is an attentive attitude towards your baby. Monitoring the child during the day, his sleep and wakefulness, his mental and motor development, his reaction to environmental influences. Do not neglect your doctor's orders. When making a scheduled visit to a neurologist, tell us about your observations of your child, this will help adjust the prescriptions.
An osteopath may also need such information. After an initial consultation with an osteopath, where time is allocated to collect all available data and direct osteopathic diagnosis, the tactics for managing the child are determined. More often than not, one procedure for correcting the found dysfunctions is not enough, and then the osteopath will prescribe a second appointment, which may be after 1-3 weeks.
What changes do parents observe in their child after treatment with an osteopath? Most often this is improved sleep, a decrease in unmotivated crying, regurgitation, positive changes in pre-speech and motor development. The neurologist observes positive dynamics during a neurological examination, and he has the opportunity to reduce the drug load on the child.