Main causes of stomach bleeding
Stomach bleeding is a deadly condition
Among the reasons that lead to the development of bleeding in the stomach are pathologies of ulcerative nature:
- Diseases in the esophagus.
- Manifestations of esophagotomy in a chronic form.
- The result of gastroesophageal reflux disease.
- The presence of a peptic ulcer in the stomach or duodenum.
- Acute ulcerative process in the digestive tract.
- Medicinal reasons include taking medications from the group of glucocorticoids, salicylates, non-steroidal anti-inflammatory drugs, reserpine and others.
- Stressful effects caused by mechanical stress, massive burn processes, myocardial infarction, septic disorders, as well as the consequences of traumatic brain injuries and other pathologies.
- Endocrine disorders developing like Zollinger-Ellison syndrome, as well as decreased functioning of the thyroid glands.
- Bleeding that is the result of pathology in the internal organs. These include disorders in the liver cells or pancreas.
- The presence of ulcers in the stomach that occurs as a result of surgery.
- Manifestations of gastritis in erosive form.
Stomach bleeding can cause esophageal varices
Non-ulcerative lesions include:
- Manifestation of varicose veins in the esophagus.
- The result of tumor processes of benign and malignant nature.
- Pathologies of the blood and blood vessels in the form of blood clotting disorders, pathological fragility of blood vessels, etc.
Types of gastrointestinal bleeding All gastrointestinal bleeding is divided into several subgroups, depending on the type:
- Acute type of bleeding. This condition develops spontaneously and, as a rule, leads to a sharp deterioration in health. It occurs for the first time against the background of existing pathology. Such bleeding can be profuse or small.
- Chronic type of bleeding. In such a case, bleeding can be detected only on the basis of an anemic condition, which is protracted or has periodic manifestations during periods of exacerbation of the underlying disease.
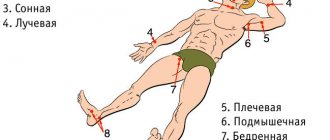
Bleeding also varies depending on the location where it occurs. Among them are bleeding:
- from the upper floor of the gastrointestinal tract. These include any lesions of the esophagus, stomach and duodenum;
- from the lower level of the gastrointestinal tract. This section includes the small, large and rectum.
In order to accurately determine the location in complex cases, it is necessary to determine the ligament of Treitz, which is involved in supporting the duodenum.
Acute gastrointestinal bleeding (clinic, diagnosis, therapy)
Gastrointestinal bleeding syndrome complicates the course of many diseases of the digestive tract and can cause death. All bleeding is divided primarily into bleeding from the upper, lower parts of the gastrointestinal tract (GIT) and bleeding of unknown etiology. Most often, this syndrome complicates diseases of the upper gastrointestinal tract (above the ligament of Treitz). Thus, in the USA, the annual number of hospitalizations for bleeding from the specified section of the gastrointestinal tract ranges from 36 to 102 patients per 100 thousand population. The gastrointestinal tract is detected twice as often in men [1, 2]. Bleeding from the lower gastrointestinal tract in general is much less common. It should be noted that due to the widespread introduction of endoscopic research methods, the proportion of bleeding of unknown etiology has decreased from 20–25% to 1–3% [3], and according to other authors, to 5–10% [4]. Among the causes of bleeding from the upper gastrointestinal tract, erosive and ulcerative lesions of the stomach and duodenum (duodenum) are in first place, and destructive processes in the duodenum are twice as likely to lead to hemorrhagic complications [5]. The mortality rate from upper GI bleeding ranges from 3.5-7% in the USA [6,7] to 14% in the UK [8], and the mortality rate from lower GI bleeding is 3.6% [6] .
There are hidden, usually chronic, gastrointestinal bleeding and obvious (massive) hemorrhages.
In acute bleeding, the degree of blood loss may vary.
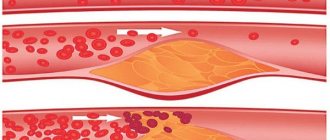
In the case of massive blood loss, the volume of circulating blood decreases, there is a discrepancy between its vascular bed, a decrease in blood pressure, an increase in heart rate, a decrease in the minute volume of blood circulation, which causes an increase in total peripheral vascular resistance due to compensatory, generalized vascular spasm. This compensatory mechanism is short-term, and with continued blood loss, irreversible hypoxic phenomena may occur in the body. First of all, liver function suffers, in which foci of necrosis may occur [3].
In the development of any bleeding, two periods are distinguished: latent, from the moment blood enters the digestive tract, and generalized, manifested by such obvious signs of blood loss as tinnitus, dizziness, weakness, cold sweat, palpitations, drop in blood pressure, and fainting. The duration of the first period depends on the rate and volume of bleeding and ranges from several minutes to a day.
Upper gastrointestinal bleeding
The main causes of bleeding from the upper gastrointestinal tract are presented in Table 1.
Table 1. Causes of bleeding from the upper gastrointestinal tract.
| Cause of bleeding (diagnosis) | Percent |
| Duodenal ulcer | 22,3 |
| Erosive duodenitis | 5,0 |
| Esophagitis | 5,3 |
| Gastritis, including hemorrhagic and erosive | 20,4 |
| Gastric ulcer | 21,3 |
| Varicose veins (esophagus and stomach) with portal hypertension | 10,3 |
| Mallory-Weiss syndrome | 5,2 |
| Malignant tumors of the esophagus and stomach | 2,9 |
Rare causes, including:
| Total 7.3 |
It has been found that 44% of all hospitalizations for upper gastrointestinal bleeding occur in patients over 60 years of age [1], and mortality rates are also significantly higher in older people. However, it should be noted that approximately 80% of upper gastrointestinal bleeding episodes resolve spontaneously or require non-massive therapy [9].
An analysis of the causes of deaths from bleeding from the upper gastrointestinal tract shows that higher mortality rates (from 50 to 70%) are associated with cases of recurrent bleeding from varicose veins of the esophagus and stomach [10]. In general, it is recurrent bleeding that is most dangerous prognostically. Risk factors for rebleeding include endoscopically detectable signs of a threat of rebleeding (streaming ongoing bleeding, blood leakage, a thrombosed vessel and a visible non-bleeding vessel). These visual signs most often accompany erosive and ulcerative lesions of the gastrointestinal tract. It is believed that these signs of bleeding are more important for a gastric ulcer than for a duodenal ulcer.
Among other signs that may cause or influence the outcome of bleeding, factors such as the size of the ulcer (giant ulcers), concomitant pathology (renal failure, cirrhosis of the liver, acute coronary insufficiency, chronic circulatory failure, tumor, endocrine, systemic diseases) should be noted. .
In general, the first place for causes of bleeding (see Table 1) is erosive and ulcerative lesions of the stomach and duodenum. And this despite the undoubted successes in the treatment of peptic ulcers achieved in recent years. Apparently, there are several reasons, and the main ones are the asymptomatic course of the ulcer and uncontrolled use of nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin, alcohol, and a combination of these factors. Thus, it is the use of NSAIDs in patients with peptic ulcers that can give a blurred picture of the disease, on the one hand, and fatal bleeding, on the other. Of no small importance in the etiology of gastrointestinal bleeding and its recurrence in patients with peptic ulcer disease is infection of patients with Helicobacter pylori (HP), especially in cases of incomplete eradication of HP, as well as the acid-peptic factor.
An overt period of upper GI bleeding typically begins with vomiting of blood (bright red blood, dark clots, or coffee-ground vomit) or the appearance of melena (black, tarry, spotty stool with a peculiar, foul odor), but it should be noted that with massive bleeding from the upper gastrointestinal tract, copious scarlet blood may also appear in the stool.
At the same time, the patient experiences anxiety or lethargy, pallor, decreased blood pressure, tachycardia, and in some cases, in patients with serious blood loss, bradycardia associated with vagal influence may be recorded. A critical hemodynamic situation occurs when blood loss reaches 40% of the total circulating blood volume. During this period, the presence of bleeding as a syndrome is beyond doubt, but it is much more difficult to determine its specific source.
The main method for diagnosing bleeding from the upper gastrointestinal tract is endoscopic visualization of the bleeding site during endoscopy; other methods (nasogastric tube, level of residual blood nitrogen) are auxiliary. As a rule, endoscopic diagnosis of ulcerative bleeding, especially of gastric localization, is not difficult. The situation is different with gastropathy, as a source of hemorrhagic complications. Endoscopically, gastropathy is determined by the presence of a large number of submucosal hemorrhages, erythema and erosions. Erosion is a defect in the mucous membrane that does not extend to its muscular plate. In fact, most endoscopists define erosion as an area of hemorrhage or shallow defects in the mucosa with a core of necrosis no more than 3–5 mm in diameter. Gastropathy is often induced by taking NSAIDs, alcohol, and occurs as a result of stress.
Bleeding from dilated veins of the esophagus and stomach is more often observed from large nodes or common varicose veins. When assessing the situation, endoscopists often focus on the color of the nodes. Red and blue color of one node is considered a risk factor for bleeding. A white spot on a varicose node can be a fibrin plug and is considered a diagnostic factor for previous bleeding, but does not indicate the possibility of recurrent bleeding [11]. Isolated gastric varices in the fundus may be the result of splenic vein thrombosis, detected by angiography. Varicose veins in the duodenum rarely bleed.
In Mallory-Weiss syndrome, the source of bleeding is a rupture of the mucosa near the gastroesophageal junction, caused by intense vomiting that accompanies prolapse of the stomach lining. In patients with this syndrome, there is an association with chronic alcohol consumption and portal hypertension.
Management of patients with bleeding from the upper gastrointestinal tract, most often associated with erosive and ulcerative lesions of the stomach and duodenum, is carried out in three stages [12].
- Urgent measures aimed at identifying the source of bleeding, stopping it and correcting hemodynamic and metabolic disorders.
- Treatment aimed at restoring the integrity of the affected organ, taking into account the etiology and pathogenesis of the underlying disease.
- Prevention of recurrent bleeding, including rational therapy of the underlying disease.
At the first stage, the set of necessary measures includes: ensuring airway patency (side position, insertion of a nasogastric tube), as well as intravenous access, determining blood type, Rh factor and biological compatibility. In addition, a blood test is taken from the patient for hemoglobin and hematocrit, the number of formed elements, the state of the blood coagulation system, the levels of urea, electrolytes, and glucose are determined; perform liver function tests; monitor arterial blood gases. In case of significant blood loss, it is necessary to restore the volume of blood volume (transfusion of saline solution, and if there are signs of sodium retention in the body, a 5% dextrose solution). If signs of a drop in blood volume appear, a transfusion should be performed within an hour: 500 ml - 1 liter of colloidal solution, followed by blood transfusion of red blood cells or whole blood (if the volume of blood loss is large, the second is preferable). During infusion therapy, care should be taken to ensure urine output is greater than 30 ml/h and to avoid volume overload. At the same time, measures should be taken to stop bleeding. If endoscopy is impossible for some reason, you can try to stop the bleeding using therapeutic methods: gastric lavage with ice water and administration of antisecretory agents, which, in addition to affecting secretion, have the ability to reduce blood flow in the mucous membrane. The use of acid production blockers for erosive and ulcerative bleeding is especially indicated. According to recent data, the use of H2-histamine receptor blockers and proton pump inhibitors (PPIs) can reduce the likelihood of surgical intervention and death by 20 and 30%, respectively [13, 14]. Modern PPIs, characterized by rapid action, are especially effective. Typically, patients are given 40 mg of omeprazole (Losec) or 50 mg of ranitidine (Zantac, etc.) intravenously. The use of famotidine (quamatel at a dose of 20 mg from two to four times a day, depending on the degree of blood loss and the severity of endoscopic changes [15] also has a good effect. Simultaneously with blockers of acid production, it is advisable to prescribe cytoprotective agents: sucralfate (Venter), preferably in in the form of an emulsion of 2.0 g every 4 hours, bismuth preparations (de-nol, ventrisol, etc.).
Diagnostic and therapeutic endoscopy (argon plasma coagulation, electrocoagulation, laser photocoagulation, diathermocoagulation, clipping, chemical coagulation with dehydration, etc.) significantly improves the results of treatment of bleeding from the upper gastrointestinal tract [12]. According to available data, for bleeding caused by erosions, intraarterial infusion of vasopressin during angiography and catheterization has a good effect (80-90%), the effect is less pronounced after intravenous infusions of vasopressin [16]. In ulcerative bleeding, the effect of vasopressin is subtle, possibly due to the larger caliber of bleeding vessels [17]. Otherwise, the treatment of bleeding in gastropathy does not differ from that described above.
As for bleeding from dilated veins of the esophagus and stomach, the drug of choice is a synthetic analogue of somatostatin (octreotide), which has now replaced vasopressin. Octreotide (Sandostatin) is administered at a dose of 25-50 mcg/hour as a continuous infusion over five days. The combined use of metoclopramide and intravenous infusions of nitroglycerin is also effective [18]. The main forms of treatment for this type of bleeding are urgent sclerotherapy or ligation [19].
Bleeding from duodenitis almost always stops spontaneously, and therefore therapeutic endoscopy is rarely required, and angiodysplasia is treated mainly with laser endoscopic coagulation therapy [20, 21].
It should be noted that for the full treatment of a patient with bleeding from the upper gastrointestinal tract, it is not enough to stop the bleeding and stabilize the patient’s condition; it is necessary to prescribe rational treatment for the underlying disease that caused the blood loss. Thus, for the treatment of erosive and ulcerative processes associated with HP, the need to prescribe full-fledged eradication therapy, taking into account not only the resistance of HP to metronidazole, but also multiresistance to other antibacterial agents, is absolutely obvious. According to the results of our studies, we can talk about a weekly triple therapy with colloidal bismuth subcitrate (240 mg twice a day), tetracycline (750 mg twice a day) and furazolidone (200 mg twice a day). A weekly or, if resistant to metronidazole, 14-day quadruple therapy is possible: omeprazole (20 mg twice a day), colloidal bismuth subcitrate (240 mg twice a day), tetracycline (500 mg four times a day) and metronidazole (500 mg twice daily). Eradication of HP with this treatment reaches 85.7–92% [22, 23].
To prevent bleeding caused by taking NSAIDs in association with HP, patients who continue to take anti-inflammatory drugs according to indications should undergo similar eradication therapy with the mandatory inclusion of a PPI (Losec, Pariet) 20 mg twice a day in the regimen, with subsequent transfer to maintenance course of PPI at half the daily dose. You can take misoprostol (200 mcg four times a day). Misoprostol is also effective in preventing stress erosions, although it causes diarrhea in some patients.
Bleeding from the lower gastrointestinal tract
The most common causes of bleeding from the lower gastrointestinal tract according to A. A. Sheptulin (2000) are:
- angiodysplasia of the small and large intestine;
- intestinal diverticulosis (including Meckel's diverticulum);
- tumors and polyps of the colon;
- tumors of the small intestine;
- chronic inflammatory bowel diseases;
- infectious colitis;
- intestinal tuberculosis;
- hemorrhoids and anal fissures;
- foreign bodies and intestinal injuries;
- aortointestinal fistulas;
- helminthiases.
The average age of patients with lower GI bleeding is higher than that of patients with upper GI bleeding. In the last few decades, mortality rates from acute bleeding from the lower gastrointestinal tract have decreased slightly, which is associated, first of all, with the improvement in the diagnosis of bleeding, thanks to the use of colonoscopy and angiography, which make it possible to select the optimal algorithm for surgical or angiographic treatment.
As with upper gastrointestinal bleeding, 80% of all episodes of lower gastrointestinal bleeding stop spontaneously, and 25% of patients with stopped bleeding experience recurrence. Unlike upper GI bleeding, most lower GI bleeding is subtle or minor, intermittent, and does not require hospitalization.
Of all the above causes of bleeding from the lower sections of the gastrointestinal tract, the most common (30%) are hemorrhages from cavernous hemangiomas and angiodysplasias of the mucous membrane of the small and large intestine (arteriovenous malformations of types I, II and III). In second place is diverticulosis (17%), and in 5-10% of cases in patients with bleeding from the lower gastrointestinal tract, the cause of the bleeding cannot be determined [4].
In diverticulosis, bleeding diverticulum is more often found in the left parts of the colon [24]. More often, bleeding occurs with concomitant diverticulitis and trauma to blood vessels. The amount of blood loss can be dangerous for older people.
Tumor processes rarely cause acute bleeding; they mainly cause chronic, hidden blood loss and iron deficiency. Hidden bleeding also often accompanies ulcerative colitis and Crohn's disease, since with this pathology large vessels, as a rule, are not damaged.
Bleeding from hemorrhoids is often not profuse, but in some cases massive blood loss may occur, requiring urgent surgical measures.
Diverticular bleeding often presents as acute, painless, and manifests itself as bright red unchanged blood (hematochezia) in the stool, although melena may occur if the source of the bleeding is located in the small intestine. Moreover, the lighter the blood, the more distal the bleeding site is located. A similar picture is often observed with angiodysplasia. Differential diagnosis in these cases is usually based on colonoscopy or angiography. In neoplastic processes, the clinical picture of bleeding is usually represented by weak, intermittent bleeding and stool with a positive reaction to occult blood. With internal hemorrhoids, pain is most often absent, and bleeding can be in the form of a stream of scarlet blood or manifested by the presence of blood on toilet paper or around the stool, but not mixed with stool, which retains its normal color. In general, when, in the presence of signs of bleeding, the intestinal contents retain their normal color, this indicates a low location of the source of bleeding (in the rectosigmoid sector). Bleeding from hemorrhoids is often observed when straining or when passing hard stool. A similar picture is also typical for patients with bleeding from anal fissures, but in this case it is often accompanied by severe pain. In addition, the same symptoms may accompany rectal polyps and rectal carcinoma. In this regard, patients with these symptoms must undergo anoscopy and sigmoidoscopy.
Bleeding, the source of which is Meckel's diverticulum, is more often observed in childhood. This is painless bleeding that may present as melena or bright scarlet blood, classically described as "currant jelly" stool. Here, too, everything depends on the level of location of the diverticulum. The diagnosis is made on the basis of radioisotope studies, which, however, often give both false-negative and false-positive results [25].
Inflammatory bowel disease is characterized by pain, which usually precedes bleeding. In these patients, blood usually mixes with the stool, which changes its color, since the source of bleeding is often located above the rectosigmoid colon. At the same time, other signs of the disease were detected, such as diarrhea, tenesmus, etc. Infectious colitis caused by pathogenic intestinal flora can also often be represented by bloody diarrhea, but in this case significant blood loss is rarely observed. The diagnosis in this case is made on the basis of sigmoidoscopy with biopsy and stool culture.
If the intestinal damage is ischemic in nature, colicky pain is observed in the abdominal cavity, often on the left, accompanied later (within 24 hours) by bloody diarrhea. This type of bleeding is characterized by minimal blood loss; massive bleeding is less common. Diagnosis is usually made by x-ray and colonoscopy with biopsy.
Of great importance in the diagnosis of bleeding from the lower gastrointestinal tract are the information obtained from collecting anamnesis and objective examination of the patient. A significant role is played by burdened heredity, previous and existing chronic pathology (oncological diseases in the patient and relatives, including familial polyposis of the colon, hepatitis, cirrhosis of the liver, urogenital pathology), as well as living and working conditions, contact with animals, etc.
Examination of the patient often allows one to draw a number of conclusions, for example, the presence of multiple telangiectasias on the skin and mucous membranes suggests that they are also present in the intestinal wall. In addition, it is important to consider symptoms of existing posthemorrhagic iron deficiency anemia, abdominal pain, diarrhea, anorexia, weight loss, or the presence of palpable abdominal masses. Colonoscopy is invaluable in the diagnosis of bleeding from the lower gastrointestinal tract, and in cases of progressive blood loss, angiography is indicated for patients.
However, despite the fact that currently there is a rich arsenal of technical means, we should not forget about simple but quite informative research methods available in any conditions - digital rectal examination, which can answer many questions, especially in pathology rectum. It is no coincidence that this procedure is in first place on the list of diagnostic measures for bleeding from the lower gastrointestinal tract. In addition to the above measures (anoscopy, sigmoidoscopy, colonoscopy with biopsy, angiography), one should not forget about the need to examine stool for occult blood with benzidine (after careful preparation of the patient). In some cases, radioisotope studies, computed tomography and NMR diagnostics help in making the correct diagnosis.
In 80% of cases, acute bleeding from the lower gastrointestinal tract stops on its own or during therapeutic measures aimed at treating the underlying disease. The most effective therapy for diverticular and angiodysplastic bleeding is: selective catheterization with intra-arterial administration of vasopressin; transcatheter embolization of intestinal arteries; endoscopic electro- and laser coagulation; sclerotherapy. For hemorrhoids, methods such as local (in suppositories) vasoconstrictor therapy can be used; A 10% solution of calcium chloride is prescribed orally (one tablespoon four to five times a day). In case of massive bleeding, rectal tamponade can be used. For repeated bleeding, surgical treatment is indicated. For internal hemorrhoids, in some cases sclerosing therapy with varicocid, ethaxiscleron and other agents is prescribed. Great importance in the prevention of hemorrhoidal recurrent bleeding is attached to the treatment of chronic obstipation syndrome in these patients.
Considering the fact that bleeding from the lower gastrointestinal tract is much more often hidden and accompanied by chronic iron deficiency anemia, it is necessary in each case to diagnose occult blood loss and their timely therapeutic correction. The presence in most patients with chronic blood loss of combined pathology of the gastrointestinal tract (chronic atrophic gastritis, intestinal dysbiosis), malnutrition with vitamin deficiencies, and in some cases alcohol abuse, creates the need to prescribe complex therapy, which is preferably carried out using combination medications. In this case, the drug of choice is the drug Ferro-Folgamma (which contains 100 mg of anhydrous iron sulfate or 37 mg of iron, folic acid (5 mg), cyanocobalamin (10 mcg) and ascorbic acid (100 mg). A successful combination of the above ingredients in one dosage form creates conditions for the most effective absorption of iron and correction of pathological processes.In addition, the presence of rapeseed oil in the preparation, as a carrier, protects the gastric mucosa from the irritating effect of iron, which is of great importance in case of its concomitant damage.
Doses and duration of treatment are selected individually based on laboratory and clinical parameters. Usually the drug is prescribed 1 capsule two to three times a day.
In any case, therapy for patients with gastrointestinal bleeding should be comprehensive and take into account the individual characteristics of patients and concomitant pathology.
For questions about literature, please contact the editor
I. V. Mayev , Doctor of Medical Sciences, Professor A. A. Samsonov , Doctor of Medical Sciences G. A. Busarova , Candidate of Medical Sciences N. R. Agapova MGMSU, Moscow
Symptoms
The symptoms of gastric bleeding do not differ fundamentally depending on the age of the patient. It is characterized by a small number of manifestations, the assessment of which does not cause any particular difficulties.
Bleeding in adults
For older people, diagnosing gastric bleeding is much easier due to the possibility of verbal contact, since the doctor can find out all the detailed information. In addition, in this case, the doctor can monitor his condition, regularly checking for complaints and dynamics.
Types and their classification
The division of glucocorticoids is carried out based on several criteria.
Depending on the reasons that caused the bleeding, 2 groups of pathologies are distinguished:
- Ulcerative bleeding;
- Bleeding not associated with an ulcer.
Most often, hemorrhages occur due to the first cause, as well as other pathologies of an erosive nature in the stomach.
The next division is based on the characteristics of the exacerbation process.
- Acute hemorrhage – intense blood loss;
- Chronic blood loss - blood flows out slowly over a long period of time.
Hemorrhage into the gastrointestinal tract most often occurs in men over 50 years of age.
Signs of hemorrhage may be obvious or occur with hidden symptoms.
Such conditions occur in a single phase or have a recurrent type.
The localization of the complication that occurs is of no small importance for diagnosis and treatment. In this regard, there are 2 more types of hemorrhages:
- Hemorrhage from the upper gastrointestinal tract;
- Irrigation of blood from the lower gastrointestinal tract.
More than 30% of hemorrhage occurs in the duodenum.
Diagnosis of gastric bleeding
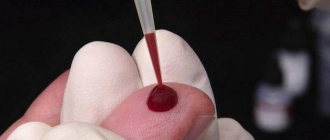
The level of hemoglobin in the blood will determine the severity of blood loss
The diagnosis of gastric bleeding is given great importance, since timely diagnosis can not only reduce the risk of developing severe complications, but also reduce the severity of the postoperative period.
Among the main diagnostic methods are:
- Finding out medical history data that relate to the presence of complaints, chronic pathologies, and great importance should also be given to clarifying the use of medications, etc.
- The patient's complaints, the time of their appearance, the conditions of occurrence and the dynamics of the process are determined. The patient’s condition and the possible dynamics of the process are assessed simultaneously.
- The condition of the stool, as well as possible vomit, is assessed. Great importance is given to the color of the content, whether it is bright red or dark, which determines the level of its occurrence, as well as its possible stop or termination.
Laboratory methods include not only stool analysis, but also a general clinical blood test. The hemoglobin level is assessed, which determines the severity of blood loss.
Determination of blood clotting using the coagulogram method. Not only the platelet component is being assessed, but also the duration of bleeding is being determined, as well as the effectiveness of the therapy used.
Of the instrumental methods, radiography of the abdominal organs is primarily used. To obtain an accurate result, it is necessary to apply contrast, which can reveal the presence of filling defects, bleeding, etc.
How to determine gastrointestinal tract?
Since gastrointestinal tract disease is not a separate disease, but is a consequence of a number of other pathologies, its manifestations are nonspecific and vary widely.
Potential symptoms of gastrointestinal tract:
- The appearance of nausea and vomiting with blood clots, the color of coffee grounds,
- General weakness of the body, from mild malaise to dizziness, fainting and even coma,
- Sudden changes in heart rate, most often from weak to rapid,
- General intoxication, including cold sweat, pallor of the skin, lips, limbs,
- A decrease in blood pressure, progressing in direct proportion to the current blood loss,
- Abnormal stools containing blood, most often with a tarry consistency.
In addition to these manifestations, the patient also suffers from symptoms of the underlying disease that caused gastrointestinal bleeding.
First aid for stomach bleeding
Initially, if the patient develops symptoms reminiscent of gastrointestinal bleeding, it is necessary to seek help from specialists by calling an ambulance. In such situations, the time will be significantly reduced and the favorable prognosis will increase.
At the same time, a simple algorithm of measures aimed at stabilizing the condition and reducing the severity of blood loss should be performed.
Before the ambulance arrives, the patient must be laid down, legs elevated and cold applied to the stomach.
These include:
- Ensuring complete rest for the patient. To do this, he needs to be given a horizontal position lying on his back, and it is recommended to raise the leg end by placing a cushion.
- Until an accurate diagnosis is made, the patient is prohibited from consuming any type of liquid or food. This may reduce the informativeness of the diagnosis.
- If there is an assumption about the possible localization of the outbreak, ice or any object that gives off cold is applied to the suspected area. This helps to narrow the vascular link and prevents the development of inflammation or swelling. This procedure should last no more than 20 minutes, between which there is a break of 3 minutes. If necessary, the procedure can be repeated, no earlier than 40 minutes from the initial setting.
- It is forbidden to perform gastric lavage or self-administration of enemas. If the patient is not in critical condition with bleeding from the upper sections, it is permissible to use Dicinon.
- In case of loss of consciousness or its disturbances, the patient is recommended to take a position with his head turned to one side. This will prevent the tongue from retracting or vomit from entering the respiratory tract. In addition, the patient is recommended to use ammonia to restore consciousness.
- During transportation, the patient is placed in a supine position and, if necessary, secured.
Specifics of urgent actions
Gastric bleeding requires immediate medical attention. It will not be possible to stop the blood loss on your own, and any delay may cost the patient’s life.
Therefore, first aid should begin with calling an ambulance or immediately transporting the victim to the nearest medical facility.
Before examining the patient by doctors, the following algorithm of actions must be followed:
- Provide the patient with a comfortable lying position;
- Eliminate its mobility;
- The person must be positioned on a flat surface so that the head is slightly lower than the rest of the body;
- If there is vomiting, turn your head to the side so that the patient does not choke on it;
- A heating pad filled with ice or any very cold object, which is wrapped several times in any material, is applied to the abdominal area;
- Ensure maximum psychological peace of the patient.
Treatment in hospital
If there is a large loss of blood, the patient is given plasma and red blood cells.
Outpatient treatment is carried out on the basis of gastroenterological or surgical hospitals.
If there is a large loss of blood, the doctor prescribes the injection of plasma and red blood cells.
There are two main directions for treating gastric bleeding. These are conservative methods that include the use of hemostatic agents, as well as iron preparations aimed at restoring reserves and improving well-being.