Classification of internal bleeding
All internal bleeding can be divided into several groups according to various criteria:
- by reason of their occurrence, they are divided into mechanical (arise due to damage to blood vessels during trauma), arrosive (caused by damage to the vascular walls due to necrosis, as well as germination or disintegration of tumors) and diapedetic (their occurrence is associated with an increase in the permeability of the walls of small vessels caused by scurvy, sepsis and a number of other reasons);
- by the nature of the damaged vessel - depending on which vessel the blood is pouring from, internal bleeding can be arterial, venous, capillary or mixed;
- According to the volume of blood loss, experts distinguish light bleeding (loss of up to 10-15% of the circulating blood volume or up to 500 ml), moderate (from 16 to 20% of the bcc, from 500 to 1000 ml), severe (from 21 to 30% of the bcc, from 1000 to 1500 ml), massive (more than 30% bcc, from 1500 ml). Bleeding with a volume of more than 2500-3000 ml, that is, from 50-60% of the bcc, is fatal.
Also, internal bleeding can be classified according to location, location of accumulation of escaping blood, the presence or absence of obvious signs of bleeding, and time of occurrence.
Knowing exactly what type of bleeding is makes it much easier to treat.
About the disease
Gastrointestinal bleeding is an extremely dangerous sign. We are talking about the leakage of blood that comes out of damaged vessels and enters the organs of the gastrointestinal tract. Bleeding is considered a complication of inflammatory and chronic diseases. It is often caused by alcohol and drug intoxication of the body.
The sources of hemorrhage are the stomach, intestines, and esophagus. The disease is as common as appendicitis. Often this phenomenon occurs as a complication of duodenal ulcers, chronic gastritis, and the appearance of neoplasms.
We recommend diagnosing gastrointestinal bleeding at the medical institution “KDS Clinic”. All examinations are carried out using modern technical equipment and innovative techniques. The disease will be diagnosed even at an early stage.
Sigmoidoscopy (rectoscopy)
If necessary, an examination of the rectum is performed. Sigmoidoscopy (rectoscopy) is a method of endoscopic examination of the rectum and distal sigmoid colon by examining their internal surface using a sigmoidoscope inserted through the anus.
Sigmoidoscopy is the most accurate and reliable examination of the rectum and lower sigmoid colon. In the practice of a coloproctologist, sigmoidoscopy is an obligatory component of every proctological examination. The examination allows you to visually assess the internal surface of the rectum and distal third of the sigmoid colon to a level of 20-35 cm from the anus.
Symptoms of internal bleeding of the gastrointestinal tract
With internal bleeding of the gastrointestinal tract, the patient is disturbed by painful sensations. The following are signs of intestinal bleeding:
- nausea and vomiting;
Regardless of food intake, the patient feels a lump in the throat and is bothered by nausea. Brown vomit is observed. Sometimes blood is found in the vomit. This is due to the fact that the blood interacts with hydrochloric acid. If blood clots appear, you should immediately consult a doctor.
- bowel dysfunction;
Diarrhea or constipation occurs, accompanied by flatulence. There is bloating and colicky pain in the intestines after eating. With hemorrhage, the stool is tarry. Looks like melena.
- general weakness;
Throughout the day the patient feels weak in the body. The temperature drops to 35.0.
- disorders of the cardiovascular system;
Tachycardia appears and blood pressure rises. Associated symptoms are dizziness, pale face, and migraine.
- fainting;
In critical cases, the patient loses consciousness due to lack of oxygen. Cold sweat and tachycardia appear.
Stomach bleeding also causes other symptoms. These include tinnitus, ascites, belching, and dysphagia.
Physical examination
Physical examination
The gastroenterologist begins the examination from the head - carefully examining the nose, mouth and throat, since sometimes the cause of bleeding can be localized.
Next, they are identified with
symptoms of anemia and hypovolemia. The patient's heart rate and blood pressure are determined. A bad symptom is an acceleration of heart rate and a drop in blood pressure (>10 mmHg). Orthostatic hypotension involves rapid or severe blood loss.
Other signs that may indicate significant blood loss include:
- cool skin;
- oliguria;
- disturbances of consciousness.
Patients with anemia feel weak, dizzy, see spots before their eyes, have chest pain, and may faint. The severity of these symptoms depends on the amount of blood lost and the rate of bleeding.
It is also important to carefully examine the patient's body for symptoms of chronic liver disease. A number of specific symptoms indicate a pathological condition of the liver:
- presence of spider veins on the skin of the breast
- gynecomastia;
- loss of axillary and pubic hair;
- yellowing of the skin;
- palmar erythema;
- enlarged spleen;
- ascites;
- swelling of the legs;
- hand tremors
Causes of stomach bleeding
Gastric bleeding is a complication of various chronic and inflammatory diseases.
Hemorrhage, or in other words hemorrhage, is often caused by a duodenal ulcer. If left untreated, the inflammatory process of the gastric mucosa leads to bleeding. The cause of gastric bleeding is the appearance of benign or malignant neoplasms. Increased pressure in the intestines leads to gastrointestinal disorders, including bleeding of internal organs.
Hiatal hernias, like tumors, are accompanied by hemorrhage and lead to death if undiagnosed. The pathology can be caused by ulcerative colitis, hemorrhoids, or anal fissures. Occurs against the background of liver cirrhosis, dysbacteriosis, pancreatitis. Diseases such as hepatitis B, C, vein thrombosis, and hypertension also lead to bleeding.
Bleeding occurs when veins are pressed by tumors and scars. The cause of gastric bleeding can be damage to blood vessels, varicose veins of the stomach and intestines, lupus erythematosus, vitamin deficiency and reduced immunity. This pathology often occurs due to circulatory disorders. For example, hemophilia, acute and chronic leukemia, hypoprothrombinemia. Bleeding is also caused by excessive intake of aspirin, alcohol or drug intoxication, overdose of drugs and chemicals. Depression and constant emotional stress can affect such symptoms.
Gastric bleeding is caused by vascular abnormalities. We are talking about erosion, thrombosis and rupture of capillaries. The cause is called a change in the hemostatic system when blood clotting is impaired.
Symptoms of neoplasms
Advanced neoplastic diseases are indicated by:
- underweight;
- enlarged, hard liver with a lumpy structure;
- palpable tumor in the abdominal cavity;
- enlarged and hard lymph nodes.
Other symptoms:
- Subcutaneous emphysema in a patient with persistent vomiting indicates Boerhaave syndrome (esophageal perforation). A prompt consultation with a surgeon is necessary.
- Telangiectasia on the mucous membranes may indicate Randu-Osler-Weber disease.
Treatment of stomach bleeding
Treatment of gastric bleeding depends on the patient’s condition and the severity of the problem. The patient is urgently hospitalized in the hospital. Next, the medical professional finds out where the hemorrhage is located, the cause and intensity of the bleeding.
The patient is given infusion and blood transfusion therapy, which stops the bleeding and normalizes the condition. Drug treatment is effective only if we are talking about hemorrhage, which develops due to problems with hemostasis.
If varicose veins of the stomach are observed, then alloying of the damaged vessels is carried out. Gastroduodenal bleeding is stopped using an endoscope. In cases of cancer and heart failure, urgent surgical intervention is required.
If a duodenal ulcer has led to the development of bleeding, then surgical intervention will be required. The bleeding wound is stitched, then gastric resection is performed. For ulcerative colitis, a subtotal resection of the colon is performed.
After the operation, the patient is prescribed medication, physiotherapeutic procedures, and bed rest. The prognosis after treatment depends on the patient’s condition and his age. In most cases, the condition returns to normal within a few days if medical care was provided on time.
Peroxidase test to confirm the presence of guaiacol
This is the most commonly used stool blood test. The test available is called Hemoccult. In this study, a stool sample is distributed into a guaiacol-impregnated cardboard box, which, if the stool contains heme, turns blue (heme causes a reaction similar to peroxidase). The more blood in the stool, the higher the likelihood of a positive result.
The Hemoccult test gives a positive result in 50% of cases when 10 ml of blood enters the gastrointestinal tract during the day. Under physiological conditions, 0.5-1.5 ml of blood is normally extravasated into the lumen of the gastrointestinal tract during the day.
The sensitivity of the first test is estimated to be approximately 30%. Performing 3 tests (which is the standard) increases the confidence to 92%. False negative results are especially common in people taking medications or foods high in vitamin C.
Relatively often, the test gives false positive results when consuming large amounts of red meat and foods high in peroxidase (radish, radish, horseradish). Taking iron supplements does not give false positive results in the study.
How do blood vessels bleed?
Bleeding can be mild, moderate or severe. His character may be:
- arterial - strong, jet;
- venous - blood loss occurs gradually;
- capillary - minor discharge due to damage to small vessels.
The problem itself can be stable/unstable, recurrent. Vessels of the mucosa, submucosal and intermuscular plexus, as well as those located outside the gastrointestinal tract, can bleed.
The expiration can last for several hours or days. In medicine there are:
- profuse blood loss - the patient loses more than 1 liter of blood in 1-3 hours and needs urgent medical attention;
- acute - less than 1 liter expires in 1-2 days, the patient’s vital signs are relatively stable;
- chronic - develops slowly, often over several weeks or even months, the intensity of symptoms gradually increases.
About the types of hemorrhagic conditions
In medicine, the internal type of hemorrhage is not classified in detail. Based on the cause of internal bleeding, there are the following types:
- Mechanical type. This condition occurs in the event of trauma to the vascular tissues through which blood flows. Occurs due to injury (often occurs in men) or due to surgery.
- The arrosive type of hemorrhage is considered to be a consequence of necrosis affecting vascular tissue or if newly formed structures grow and disintegrate.
- Diapedetic type. In this condition, the vascular tissue is not destroyed, but due to various pathological processes (hemorrhagic vasculitic changes, phosphorus poisoning and many other processes), the capillary network becomes highly permeable.
According to the type of vascular tissue there are:
- Arterial type, where destruction of the arterial vessel is diagnosed.
- Venous type, in which the veins are damaged.
- Capillary type. The blood medium spreads evenly from the capillary vessels. If blood pours out from different organs, then this is a parenchymal type of hemorrhage.
- Mixed type. Occurs with destructive changes in venous, arterial and capillary vessels.
If we take into account localization, then there are:
- Gastric and intestinal types of hemorrhages. Possible due to ulcerative processes in the stomach and duodenum, gastritis changes, inflammation of the intestines, also if the mucous membrane is cracked and there are newly formed structures. If esophageal hemorrhages are observed, the cause is liver dysfunction. In case of intestinal hemorrhages or intraperitoneal bleeding, the cause is hemorrhoidal changes or rectal fissures.
- Hemorrhages localized in the cavity spaces of the pleura due to torn vascular tissues between the ribs (hemothorax). This condition occurs when there is a closed injury to the chest.
- Hemorrhages that flow into the pericardium (pericardial sac), which compresses the heart muscle (hemipericardium). If this condition is ignored, it can manifest itself as heart failure followed by death. Such hemorrhage can occur with a mechanically damaged chest in the front, or surgical intervention on the heart muscle.
- Intra-articular hemorrhages (hemarthrosis). This type of bleeding often occurs when joint tissues are damaged (usually the knee joints).
According to the location where blood accumulates, there are:
- Hemorrhages in cavities. They are divided into bleeding of the abdominal cavity (if the abdominal area, chest and various organs are injured), pleural membrane (if the ribs are broken), and the skull.
- Hemorrhages within tissue structures, where blood accumulates in deep tissues that disintegrate, causing hematomas.
According to the amount of blood loss there are:
- Mild hemorrhages, where total blood loss is no more than 15% of the total blood circulation.
- Moderately severe hemorrhagic conditions, where blood is lost 20% of the total blood circulation.
- Severe bleeding, where the patient has lost approximately 1.5 liters of blood
- Massively manifested hemorrhagic condition. The total volume of blood circulation is reduced by more than 30%.
- Fatal blood loss occurs when the total circulating blood volume decreases above 60%.
Hemorrhages can occur:
- Obviously. After a certain time, the blood comes out into the external environment through the patient’s natural type of orifices.
- Is hidden. There are no main symptomatic manifestations; perhaps they are mild.
Given the time period, there are:
- Primary identified blood loss. They signal themselves after the vascular wall is ruptured.
- Secondary detected hemorrhages. They are observed a certain time after the traumatic factor that provoked them. This type of hemorrhage is divided into early, where manifestations occur after a period of 1 to 3 days due to the fact that an embolus has come out of damaged vascular tissue or the suture has been incorrectly applied. Late, secondarily detected hemorrhages appear three days after the vessel is damaged as a result of infection joining the wound.
General rules of first aid for bleeding
If the victim has lost a significant amount of blood, try to lay him down and elevate his legs.
Do not touch the wound with your hands or remove glass shards from it.
If sand and rust get into the wound, do not wash the damage, as this will increase the bleeding.
If the wound becomes dirty, you need to carefully remove the dirt in the direction from the wound, then treat the cleaned edges with an antiseptic.
When treating the edges of a wound with an iodine solution, do not allow the antiseptic to get inside the wound.
Depending on the type of blood loss, try to stop the bleeding using a tourniquet, twisting, or squeezing the damaged vessel.
First aid for capillary bleeding
Bleeding from the capillaries is not accompanied by large blood loss and stops relatively quickly. A sign of capillary damage is the appearance of a gentle stream of blood on the wound.
First aid for this bleeding includes treating the edges of the wound with an alcohol antiseptic (iodine), on which an aseptic gauze bandage is applied. Please note that the bandage is not tight. Usually, with capillary bleeding, there is no need to go to the hospital, with the exception of situations where the damage is extensive.
1 First aid for bleeding
2 First aid for bleeding
3 First aid for bleeding
First aid for venous bleeding
A sign of venous bleeding is rapidly flowing dark blood. Its flow is uniform, without gushing or pulsating.
With venous bleeding, blood clots may appear; they cannot be removed, since in this case blood loss may increase.
To stop bleeding, apply a pressure aseptic bandage to the wound. If blood loss continues, it is necessary to apply a tourniquet below the damaged area. To reduce injury to soft tissues and skin, a soft pad is placed on them (under the tourniquet). It is necessary to make a note indicating the time of application of the tourniquet. The maximum time for wearing a tourniquet is 2 hours in warm weather and 1 hour at sub-zero temperatures. The tourniquet cannot be held longer than this time, otherwise the bloodless tissue will begin to die. If you don’t have a tourniquet, you can make twists from available materials: a bandage, a belt, a towel, a piece of fabric using a handle and a short stick. The time frame for the spins is the same. Try not to use any hemostatic drugs without a doctor's prescription.
First aid for arterial bleeding
Arterial bleeding is one of the most dangerous. The main sign of arterial damage is bright scarlet blood flowing out in a pulsating stream at high speed. If large arteries are damaged, the blood begins to flow intermittently, like a fountain.
First aid for this bleeding is to apply a hemostatic tourniquet above the level of the wound. You can also use a twist. Time restrictions are the same.
If there is no tourniquet or twist, you can stop the bleeding by pressing the artery above the damaged area with your finger, i.e. at the pulsation point.
In case of bleeding from the brachial, ulnar, femoral or popliteal artery, you can fix the arm or leg as bent as possible in an elevated position.
Acute bleeding from the digestive tract
At the first signs of bleeding from the digestive tract, the patient should be urgently hospitalized in a surgical clinic; all therapeutic measures begin as early as possible and are carried out simultaneously with diagnostic ones. The efficiency, clarity, and coherence of the actions of the medical staff at all stages of medical care (calling a doctor, transporting to the hospital, processing medical documentation, delivery to the surgical department, determining blood type and Rh compatibility, other laboratory, diagnostic and therapeutic measures) largely depends on the fate of the patient. In no case should you expect that the bleeding can stop and not happen again - this is a gross medical error.
Arriving at the patient, the doctor quickly collects anamnesis and analyzes the main complaints (according to the patient or relatives), quickly conducts a general examination, examines the pulse, determines the heart rate and breathing rate, organizes transportation of the patient (through the ambulance service, and if this is not possible, for example due to the distance from the city center, then using available means - cars, horse-drawn vehicles, etc.). Along the way, while performing all these steps, you should find out whether the patient has any medical documents - extracts from the medical history, results of previous studies, data on blood type (certificate or stamp in the passport), etc., which may be useful for establishing a diagnosis and further treatment. A small amount of vomit (for hematemesis) and/or stool (not for chalk) should be sent to the hospital to be tested for blood content.
Situations that a doctor may encounter, assuming a patient has bleeding from the digestive tract, can be extremely varied (when calling a patient at home, in transport, at the workplace, on the street, in a distant village, etc.), so give clear specific recommendations for each case are hardly possible. However, in all cases, the doctor must try to confirm the assumption of bleeding, at least approximately determine its severity and refer the patient to a medical institution where there are conditions for carrying out the necessary diagnostic and therapeutic measures.
If acute bleeding from the digestive tract is suspected, the doctor must decide at different stages - from the moment of visiting the patient to hospitalization and in the process of emergency examination and the beginning of the first treatment measures - the following urgent issues (and the sooner the better).
- Confirm that there was indeed bleeding from the digestive tract. This is necessary due to the fact that some symptoms may be misinterpreted by patients and others. For example, vomiting of the “coffee grounds” type, characteristic of gastric bleeding, may actually be vomiting after drinking coffee or coffee drinks, and black stools resembling melena may be after eating beets, ingesting carbolene, drugs containing bismuth salts (vicalin , vi-kairo, de-nol), iron (ferrolex, ferrogradumet), etc. If the presence of bleeding is confirmed, the patient must be urgently hospitalized in the surgical department of the hospital to carry out the necessary diagnostic examination and treatment.
- When bleeding into the abdominal cavity (due to perforation of a gastric or duodenal ulcer, the wall of the gallbladder with purulent or gangrenous cholecystitis, etc.), an outpouring of gastric juice and bile occurs into the peritoneal cavity with signs of its irritation and the rapid development of peritonitis with the corresponding clinical picture.
- Determine the location of bleeding (esophagus, stomach, duodenum, etc.). Often, on the basis of characteristic clinical symptoms, it can be roughly determined (vomiting of scarlet blood - bleeding from the esophagus, "coffee grounds" type - from the stomach, stools like "melena" (in el en os - dark, black) - bleeding from the stomach and thin intestines, proximal parts of the colon; release of pure blood - in case of bleeding from its distal parts). Urgent further examination of the patient allows in many cases to establish the site of bleeding with greater confidence.
- Determine the cause of bleeding (underlying disease).
- Determine (at least approximately) the degree of blood loss.
It is believed that acute blood loss (over several minutes or hours) of at least 500 ml of blood is accompanied by clinical symptoms. Loss of 700-800 ml of blood may manifest as hematemesis and/or melena. In many cases, it occurs in patients with a pre-established diagnosis (peptic ulcer, portal cirrhosis of the liver with esophagocardial varicose veins), usually with increasing symptoms of exacerbation of the disease, after various violations of the diet and nature of the diet (taking spicy irritating foods, large doses of strong alcoholic drinks ) or physical activity (lifting heavy weights, etc.).
The clinical picture of acute bleeding into the lumen of the stomach or intestines is often quite characteristic. The most common are two types of symptoms:
- discharge of blood (fresh or altered) with vomiting or bowel movements;
- vascular collapse.
Often, it is the discharge of blood through vomit or stool that frightens the patient, causing him to think about bleeding from the stomach or intestines (especially if he has had similar symptoms before or has heard about them) and consult a doctor.
In acute venous esophageal-gastric bleeding (for example, from varicose veins), the secreted blood is dark cherry in color. During gastric bleeding in patients with preserved secretion of gastric juice, the color of the blood in the vomit changes: due to the interaction of hemoglobin heme with hydrochloric (hydrochloric) acid, hydrochloric acid hematin is formed, which has a brown color; The vomit takes on the appearance of coffee grounds. In case of acute gastroduodenal bleeding that occurs against the background of achlorhydria from an arterial vessel of the mucous membrane of the stomach or duodenum, the vomit contains fresh scarlet unchanged blood.
Bleeding from the duodenum (for example, from a peptic ulcer), as well as from other parts of the small intestine, is manifested by black stool - melena or tarry stool. This occurs due to the gradual formation of black iron sulfide from hemoglobin (under the influence of digestive enzymes as the blood moves through the intestines). It should be borne in mind that melena can also occur with bleeding from the esophagus and stomach in the absence of vomiting or due to the fact that not all the blood was excreted along with the vomit, but some of it entered the intestines. It should also be remembered that with very heavy profuse bleeding from the upper intestine, blood, quickly moving through it (when large quantities of blood enter the intestine, its peristalsis sharply increases), can be excreted with feces and unchanged. Therefore, the appearance of melena is very important for diagnosing internal bleeding. It must also be remembered that hematemesis and melena occur only some time after the start of bleeding: the first symptom may be vascular collapse.
It should be borne in mind that esophageal-gastric bleeding is sometimes mistaken for pulmonary bleeding (in which part of the coughed up blood can be swallowed and then vomited in a modified form like “coffee grounds”) and for intestinal bleeding in women from the uterus. Differential diagnosis should also be carried out with acute bleeding into the abdominal cavity (with rupture of the liver, spleen, ectopic pregnancy, etc.), when the leading clinical picture is a suddenly developing collapse in a patient with a pathology of the digestive tract (peptic ulcer, diverticulum, tumor, etc.) .d.). It must be remembered that when bleeding from the gastrointestinal tract, some time usually passes, although relatively short, before the blood is released into the external environment.
The second manifestation of acute massive bleeding is vascular collapse (drop in blood pressure, general weakness, thready pulse, tachycardia, pale skin, etc.).
With acute bleeding, patients experience sudden weakness, dizziness, dry mouth, dry eyes, tinnitus, palpitations, nausea, and drowsiness. At first they are somewhat excited, then fainting or a collaptoid state sets in.” The patient’s face is characterized by a sharp, in some cases “deadly” pallor, his skin is covered with cold, sticky sweat. Tachycardia and tachypnea are detected; the wings of the nose are involved in the act of inhalation.
The general condition of the patient is determined not only by the degree of blood loss, but also by its speed. Thus, rapidly developing bleeding (hours, days) with a loss of 1/3-1/4 of the total blood volume can threaten the patient’s death; relatively slow (weeks, months) bleeding, even with a loss of total blood volume, provided it stops, can end safely.
Sometimes even a quick examination allows you to suspect an underlying disease that could be the source of bleeding. Thus, icteric staining of the skin and mucous membranes, skin scratching, the well-known “liver stigmata” make it possible to suspect cirrhosis of the liver and bleeding from varicose veins of the esophagus (it should be borne in mind that with cirrhosis of the liver, so-called hepatogenic gastroduoes occur in 10-25% of cases -denal ulcers, which can also be a source of bleeding). If the patient is exhausted and his skin has an earthy-gray color, the presence of a malignant neoplasm of the digestive tract can be assumed. At any tumor location, bleeding may occur due to tumor invasion of a large vessel. It has been noted that with tumors of the cecum and ascending small intestine, bleeding and anemia occur more often than with lesions of other parts of the small intestine by a malignant tumor.
To identify the source of acute bleeding from the esophagus, stomach and duodenum (usually upon admission of the patient to the hospital), urgent X-ray and endoscopic examinations are performed. If acute bleeding from the colon is suspected, sigmoidoscopy and colonoscopy are used (one should not forget about examining the anal area and digital examination of the rectum, since the source of quite severe bleeding can be, for example, hemorrhoids or a bleeding tumor of the rectum). Diagnostic endoscopy in such patients should be performed early rather than waiting for bleeding to stop. The tragedy for these patients may be that endoscopy is postponed, and conservative therapy without accurately identifying the source of bleeding is ineffective. In addition, bleeding that is minor at first can later become profuse and endanger the patient’s life.
Currently, endoscopic examination carried out at the height of bleeding can pursue not only diagnostic, but also therapeutic purposes - injections of sclerosing substances into varicose veins of the esophagus, direct application of hemostatic and coagulating substances to the bleeding area of the mucous membrane, ulcers, etc., electrocoagulation, cauterization laser radiation. In case of multiple lesions, endoscopy can determine the true sources of bleeding.
In some diagnostically difficult cases, the arteriography method allows identifying the true source of profuse bleeding from the digestive tract in the presence of several potential sources of hemorrhage.
However, despite the use of the most advanced diagnostic methods, in a number of patients the cause of bleeding from the gastrointestinal tract remains unclear. The cause of gastroduodenal bleeding during X-ray and even endoscopic examination, according to various authors, cannot be determined in 10-15% of cases (these figures are much better than 15-20 years ago).
According to some authors, in patients with potential sources of bleeding, in 10-25% of cases, other causes were actually identified.
Diagnostic laparotomy does not always allow one to determine the source of bleeding. In some cases, the source of bleeding is not detected even at autopsy. Bleeding of unknown etiology is observed in 6.5-13% and, according to some data, in 25% of cases.
Acute bleeding can occur in different ways. In this regard, the following are highlighted:
- acute bleeding, single, short-term (minutes, hours);
- prolonged (from 1 to 3 days); 3) long-term (3-7 days);
- recurrent (1-7 days), externally manifested by two or more acute episodes of blood loss. Particularly severe acute bleeding, accompanied by massive blood loss, is designated as profuse.
There are many classifications of the severity of acute blood loss. A fairly common classification is that there are 4 degrees of bleeding severity.
In the first degree of severity, the bleeding is not profuse, accompanied only by minor hemodynamic changes (blood pressure is within normal limits, the pulse is slightly increased), the general condition of the patient is satisfactory, but a short-term loss of consciousness may be observed. The hemoglobin content is not lower than 100 g/l, the hematocrit (hematocrit number) is above 30, the deficit in circulating blood volume (CBV) is no more than 5%.
In the second degree of severity of bleeding, the general condition of patients is of moderate severity, pallor of the skin and visible mucous membranes is noted, blood pressure drops to 90 mm Hg. Art., hemoglobin content is up to 85 g/l, hematocrit is up to 30, the deficit of circulating blood volume (CBV) reaches 15%.
With the third degree of severity of bleeding, the patient's condition is serious, pronounced hemodynamic changes are observed: the skin is pale, covered with cold sweat, the patient yawns, feels thirsty, fainting occurs, the pulse is thready, blood pressure drops to 60 mm Hg. Art., hemoglobin - up to 50 g/l, hematocrit - below 30, BCC deficiency - 30%.
With the fourth degree of severity, the patient’s condition is extremely serious; a picture of collapse is observed, the pulse is not detected, the hemoglobin content is below 50 g/l, the BCC deficiency exceeds 30%.
It should be noted that different authors, when assessing the severity of blood loss, focus on different symptoms (the degree of hemoglobin reduction, the content of red blood cells per unit volume of blood, hematocrit, bcc, some clinical criteria). In addition, taking into account and comparing a number of indicators, which do not always change strictly in parallel, makes it difficult to clearly assess the degree of blood loss - this most important indicator of the patient’s condition, which determines the nature and priority of emergency treatment measures and prognosis. In addition, the indicators of red blood per unit volume in the first hours and days usually do not change (blood is lost - oligemia occurs), therefore one cannot focus on the content of hemoglobin, erythrocytes and hematocrit in the blood precisely during the most critical period - during blood loss and in the next few hours after it. To assess the degree of blood loss, determining the total volume of blood volume, for example, using a solution of polyvinyl alcohol or polyglucin, as well as plasma and erythrocyte mass using erythrocytes, can be of great importance during this period. Determining the BCC is important while simultaneously taking into account the loss of globular mass, or “globular volume” (GO, i.e., the total volume of red blood cell loss), since the BCC is restored relatively quickly due to the entry of tissue fluid into the blood, and the loss of red blood cells is restored much more slowly; therefore, in the first hours after bleeding, the deficit of blood volume also does not very accurately reflect the general condition of the patient.
In practice, when determining the degree of blood loss, they usually use a fairly simple Algover method, which allows one to determine the ratio of pulse rate and systolic pressure (“shock index”). With a shock index of 0.5, blood loss is 15%, with an index of about 1 - 30%, with an index of 2 - up to 70%. In this case, the clinical picture and general condition of the patient must be taken into account.
In practice, it is more expedient, more convenient and easier to distinguish 3 degrees of severity of acute bleeding:
- I - with blood loss up to 1-1.5 liters of blood and corresponding clinical and laboratory changes, BCC deficiency up to 20%;
- II - with blood loss from 1.5 to 2.5 liters of blood and a deficit of blood volume up to 20-40%;
- III - with blood loss of 2.5-3 liters or more and a deficit of blood volume up to 40-70%.
Very tentatively, we can assume that the I degree of blood loss does not threaten the patient’s life (provided the bleeding stops), with the II degree the threat to the patient’s life is very significant, adequate therapeutic measures are necessary (see below), with the III degree of severity of blood loss without treatment there is a threat to life is very high, and even with timely complex treatment, mortality can be 20-30% or more.
This classification allows the doctor to quickly understand the degree of blood loss and take the necessary measures accordingly. It should be remembered that the severity of the patient’s condition is determined by:
- degree of blood loss;
- its sharpness;
- the initial condition of the patient, depending on the severity and nature of the disease that caused blood loss, as well as on concomitant diseases (chronic diseases of the heart or lungs, complicated by circulatory failure, renal failure, etc.) and the general physical development and reactivity of the patient’s body.
There are three stages of pathological and compensatory changes that occur during bleeding and immediately after it:
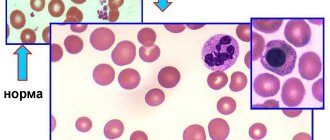
- oligemia, accompanied by reflex vascular spasm and the release of blood into the bloodstream from the depot. During this period (12-24 hours), the amount of hemoglobin and red blood cells per unit volume of blood does not change, therefore, these indicators cannot be significant in diagnosing bleeding and assessing its severity (however, already in the first hours the process of intercellular - tissue flow begins and gradually intensifies - fluids into the bloodstream);
- hydremia (hemodilution), which occurs on the 2-3rd day due to the influx of tissue fluid into the vascular bed; the content of hemoglobin and red blood cells per unit volume of blood decreases proportionally (the color index remains within the normal range - 0.8-1);
- period of sharp activation of erythropoiesis (starting from the 3-4th day): reticulocytes appear in the peripheral blood; If iron reserves in the body are depleted, anemia becomes hypochromic.
In case of acute bleeding from the digestive tract, the prognosis is always serious, since from the first manifestations of bleeding to identifying the source and taking radical (surgical) measures to stop it, it often takes quite a lot of time. In addition, there is always no complete confidence that the bleeding has stopped and will not happen again. It is believed, for example, that with severe gastroduodenal ulcer bleeding, approximately 1/2-1/3 of patients die (due to sudden blood loss, it is not possible to urgently hospitalize the patient, quickly find out the causes of the bleeding and stop it, etc.). It should be remembered that with many diseases of the digestive system, relapses of acute bleeding are possible.
A patient with acute bleeding from the digestive tract or suspected of such must be urgently hospitalized in a surgical hospital.
It is better to transport the patient in a horizontal position so that cerebral circulation does not suffer due to oligemia; to prevent aspiration of vomit, it is necessary to turn the patient's head to the side; It is necessary to ensure that the tongue does not sink in, and periodically clean the oral cavity with gauze swabs or rinse with cold water. Cold applied to the abdominal area is usually recommended (a regular rubber heating pad, a strong plastic bag or bottle filled with pieces of ice, snow or cold water). The patient must be taken to the car on a stretcher, and from the car to the hospital on a gurney. The patient should not be allowed to walk on his own, as physical stress may increase bleeding; in addition, due to severe blood loss in a patient in an upright position, cerebral ischemia may worsen and a faint or even coma may occur and, finally, due to severe weakness, the patient may fall and be injured.
Treatment measures are determined by the degree and rate of blood loss, the ability to identify the source of bleeding, and the presence and nature of concomitant diseases. In almost all cases, treatment measures usually pursue the following main goals:
- stopping bleeding;
- combating oligemia through replacement therapy (reimbursement, first of all, of the volume of blood loss, in more severe cases, replacement of red blood cell mass);
- fight against D VS syndrome;
- fight against shock and collapse;
- for bleeding from the upper digestive tract, both initially caused by the high proteolytic activity of gastric juice (gastroduodenal and esophageal ulcers, erosive gastritis, duodenitis), and maintained and aggravated by this factor, drugs are used that sharply suppress gastric secretion.
Stopping bleeding from the digestive tract is possible only after identifying its source using modern endoscopic methods by local impact on the bleeding area or by surgery. Some general measures carried out for hemostatic purposes often begin earlier, from the moment the ambulance arrives and/or during the subsequent transportation of the patient. Usually they start with the use of agents that increase the coagulation properties of blood. Traditionally, 10-15 ml of a 10% solution of kalysch chloride is immediately administered intravenously slowly; 1 ml of 1% solution of Vikasol intramuscularly; 100-200 ml of a 5% solution of aminocaproic acid in an isotonic solution of sodium chloride intravenously, by drip, if necessary, the administration is repeated after 4 hours until a daily dose of 10-15 g of the drug or 5-10 ml of a 1% solution of para-(Aminomethyl)-benzoic acid is reached (synonym - amben or pamba); intravenously or intramuscularly, followed by intravenous drip administration of 2-3 g of fibrinogen (available in ampoules with a capacity of 250-500 ml, dissolved in heated water for injection). It should be noted that these remedies are in most cases ineffective; Thus, calcium supplements help only in cases of severe deficiency of this ion in the blood, which rarely occurs even with massive bleeding. Vikasol is a synthetic water-soluble analogue of vitamin K, which takes part in the formation of prothrombin and promotes normal blood clotting. However, its effect is manifested only when the content of prothrombin in the blood decreases (below 30-35%), which is observed in severe liver diseases (prothrombin is formed in the liver), with obstructive jaundice (absorption of vitamin K occurs with the participation of bile), with an overdose of anticoagulants or with severe intestinal malabsorption syndrome (with enterocolitis, nonspecific ulcerative colitis, etc.). Vitamin K is found in significant quantities in many foods of plant origin (spinach, cauliflower, some fruits and root vegetables), in liver (especially pork), less of it in milk, chicken eggs and some other products; Quite a large amount of vitamin K is synthesized by intestinal microflora. It is believed that the effect of Vikasol appears only after 12-18 hours (with slow intravenous administration - earlier).
Aminocaproic acid and Ambien are effective only for bleeding caused by increased fibrinolysis; Some effect of the drugs can be expected in case of severe liver diseases (for example, with bleeding from varicose veins of the esophagus and cardia of the stomach, which developed against the background of cirrhosis of the liver). It is also advisable to administer aminocaproic acid during massive transfusions of canned blood (when secondary hypofibrinogenemia may occur). Fibrinogen is effective for bleeding caused by hypofibrinogenemia, for example, with cirrhosis of the liver with a clinical picture of its functional failure (fibrinogen is formed in the liver). Therefore, the effectiveness of these measures is very conditional and they help only in rare specific cases, in particular, with liver failure, with bleeding caused by surgery, with hereditary hypofibrinogenemia.
Relatively recently, in case of blood loss of the first degree, transfusion of plasma and blood substitutes (polyglucin, rheopolyglucin, gelatin-zero, etc.) was recommended to compensate for blood loss. However, the infusion of so-called blood substitutes to replenish the volume of blood loss has only a very short-term effect. It should also be borne in mind that hemodez lowers blood pressure, which is undesirable in case of large blood losses and arterial hypotension. In case of blood loss of II severity, transfusion of blood and blood substitute fluids in a ratio of 1:1 was recommended; for grade III blood loss - in a ratio of 3:1. Direct transfusion of same-type blood from a donor is very effective (in terms of stopping bleeding and blood replacement), but this is difficult to implement in general medical practice. Therefore, in recent years, the first thing recommended is the infusion of fresh frozen plasma (500-1000 ml intravenously in a stream or fairly quickly by drip - about 100 drops per minute). In this case, three main goals are pursued: combating DIC, replenishing the loss of blood volume (plasma), stopping bleeding (since fresh frozen plasma best preserves blood clotting factors, so it has hemostatic properties). If clinical signs of anemia persist (pallor of the conjunctiva and mucous membranes, shortness of breath), additional red blood cells are transfused. In whole (canned) blood, the factors of blood coagulation and fibrinolysis are largely inactivated (inactivation of the latter can contribute to the intensification of DIC syndrome and the deterioration of the patient’s condition); therefore, transfusion of canned blood is possible only in cases of massive blood loss, when there is no fresh frozen plasma and red blood cells. Transfusion of platelet mass, recommended by some authors, is, firstly, difficult to obtain, and, secondly, the number of platelets in a person is normally 5-10 times higher than the amount below which (50-109 per 1 l) and bleeding is possible due to lack of platelets.
To maintain cardiac activity, caffeine and cordiamine are administered. Pressor amine preparations (mesaton, norepinephrine) are contraindicated until blood volume is completely restored, as they increase spasm of small vessels and contribute to the development of disseminated intravascular coagulation syndrome.
Signs of the effectiveness of blood replacement therapy are normalization of blood pressure (systolic and especially diastolic), warming and pinking of the skin, and decreased sweating.
Poor prognostic signs are, in addition to ongoing blood loss and general deterioration of the patient’s condition, a change from metabolic acidosis (2nd day) to alkalosis, and the appearance of signs of disseminated intravascular coagulation syndrome. In severe and protracted cases, when signs of DIC syndrome appear (developing as a result of capillary stasis, an increase in the content of procoagulants in the blood and an increase in the adhesive ability of platelets, as well as after the administration of large quantities of so-called hemostatic agents), heparin is administered (up to 20,000-500 000 units/day) and fibrinolysin (intravenous drip of 20,000-400,000 units/day). Early surgical intervention should be resorted to only if bleeding persists despite ongoing therapy.
Recently, for moderate esophageal and gastroduodenal bleeding caused by the “aggressive” effect of active gastric juice on the mucous membrane of these organs, H2 receptor blockers have been successfully used, sharply suppressing gastric secretion: 2 ml of a 10% solution of cimetidine (synonyms: belomet, cinamet, histadil, neutronorm, simetidine, primamet, tagamet, etc.) intravenously slowly or intramuscularly; 2 ml of a 25% solution of ranitidine hydrochloride (synonyms: ranisan, acylok-E, zantac, zoran, peltoran, ulcodin, ulkoran, etc.) intravenously slowly, as well as famotidine (synonyms: lecidil, gastrosidine, ulfamide, famosan, etc.). In the absence of ampoule forms, Hg blockers can be prescribed orally in tablets (cimetidine 200 mg, ranitidine 150 mg, famotidine 40 mg) if there is no severe vomiting. By suppressing gastric secretion, they thereby suppress the proteolytic effect of gastric juice, which is especially important for peptic ulcers, erosive gastroduodenitis, varicose veins of the esophagus and cardia of the stomach (it goes without saying that these remedies are useless for gastric achylia). A blocker of the H+K+ATPase enzyme, omeprazole (omeprol), which is prescribed orally, 1 capsule (20 mg) per day, has a strong inhibitory effect on gastric secretion. Gastric secretion is also suppressed by pirenzipene hydrochloride (gastrocepin), which is administered intravenously in 2 ml (10 mg) or per os in 25 mg tablets. Somatostatin (stylamine), which inhibits gastric secretion, reduces mesenteric blood flow and pressure in the portal vein system and increases platelet aggregation, is highly effective for gastroduodenal ulcer bleeding, as well as for bleeding from varicose veins of the esophagus and cardia. It is used as a continuous intravenous drip (6 mg/day). First, 250 mcg of the drug is administered intravenously once in a solvent specially attached to each ampoule, then after 3-5 minutes - intravenously in a continuous drip at the rate of 250 mcg/hour; after bleeding stops, administration continues for another 48-72 hours.
To prevent erosive and ulcerative bleeding caused by non-steroidal anti-inflammatory drugs (drug-induced erosive and ulcerative lesions of the stomach and duodenum), and at the first signs of moderate bleeding, in recent years a synthetic analogue of natural prostaglandin E, misoprostol, has been used. Cytotec sharply suppresses gastric secretion and pepsin production, helping to stop bleeding, increases gastric secretion, and causes rapid cessation of erosive and ulcerative bleeding.
In the absence of strong modern inhibitors of gastric secretion, large doses of antacids (Almagel, Maalox, Gelusillac, Gastrolugel, etc.) that bind hydrochloric (hydrochloric) acid are prescribed orally; 25-30 ml or 2 tablets (finely crushed) every 1.5-2 hours. Antacids are prescribed orally or administered through a gastric tube.
For bleeding from small vessels (for example, with erosive gastritis), vasopressin is administered; in its absence, pituitrin (the main active ingredients are oxytocin and vasopressin) is administered subcutaneously or intramuscularly, 0.2-0.25 ml (1 -1.2 units) 4-6 times a day or intravenously, 1 ml (5 units) in 500 ml of 5% glucose solution. Pituitrin is often recommended for bleeding from esophageal varices. When bleeding from varicose veins of the esophagus, a probe with an inflatable balloon (such as a Blackmore balloon) is used to compress them.
Patients with cirrhosis of the liver are prescribed broad-spectrum antibiotics orally or parenterally to suppress the putrefactive decomposition of blood entering the intestines, to prevent the adverse effects of its breakdown products on the liver and hepatic coma; Lactulose (Normaza) is also prescribed internally.
As our clinical observations have shown (more than 160 patients over the past 10 years), this tactic in most cases allows us to stop bleeding and gain time to organize the transfer of patients to a surgical clinic.
For gastric bleeding, gastric lavage with ice water is recommended (special devices have even been created for this purpose, but recently there has been some disappointment in this method), selective intra-arterial infusion of vasoconstrictors, electrocoagulation or laser coagulation of the bleeding area through an endoscope (due to the complexity and due to the unsafety of endoscopic methods, they are used only in large endoscopic centers).
It should be emphasized once again that all these measures are temporary and are carried out during the period of transfer of the patient to the surgical clinic and during preparation for surgery or for endoscopic laser coagulation or electrocoagulation of the bleeding area of the mucous membrane of the stomach and duodenum. And only when bleeding has stopped, justified by objective indicators, treatment is then carried out conservatively. These measures should be carried out in the presence of contraindications to surgical treatment (decompensated heart disease with circulatory failure PA - stage III, chronic pneumonia with severe insufficiency of external respiration function, old age of patients suffering from serious diseases at the same time, etc.).
With conservative management of patients, fasting is recommended in the first 1-2 days (liquid is administered subcutaneously or into the rectum in the form of an isotonic sodium chloride solution, 5% glucose solution). Then liquid food is prescribed, possibly with pieces of ice (diet 1, Meulengracht diet). In a more distant period (when the bleeding has stopped and the patient has recovered from a serious condition), the underlying disease is treated (if it is not eliminated surgically in the acute period) and parenteral iron supplements are prescribed (to eliminate iron deficiency anemia that occurs after severe bleeding).