Introduction
Microvascular angina (MVA) is a disease of the cardiovascular system, accompanied by chest pain typical of angina and electrocardiographic changes characteristic of myocardial ischemia, without damage to the epicardial coronary arteries, according to angiography [1]. SWS is characterized by prolonged pain in the heart area not only during and after physical activity [2], but also at rest, often accompanied by a decrease in the pain threshold and a change in the emotional status of patients. Despite the fact that the prognosis for MVA is usually favorable, angina pectoris significantly worsens the quality of life of patients and poses a significant burden on the healthcare system. Diagnosis of MBC in real clinical practice is often based on history and clinical data, which leads to false-positive or false-negative results. With coronary angiography, only the epicardial arteries can be seen, and it is not possible to assess the state of the microvasculature [3]. Considering the widespread prevalence of MHS among patients with heart pain, an in-depth study of this pathology, its diagnosis and treatment is necessary.
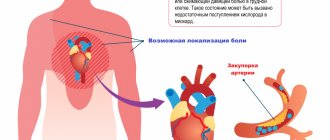
Symptoms of angina pectoris
Patients experience pain of varying intensity: from mild discomfort behind the sternum to severe pain in the heart muscle. The duration of a typical attack is 3-5 minutes, there are pronounced onset and end phases. The intensity of symptoms decreases when the provoking factor is eliminated. The pain of angina pectoris is radiating and can affect the jaw, shoulder blade, arm or neck.
During an attack, the patient feels weak, shortness of breath appears, and tachycardia and arrhythmia develop. Representatives of the older age group may experience a sharp increase or decrease in blood pressure. In rare cases, an atypical attack develops, accompanied by abdominal pain, nausea and vomiting.
The frequency of manifestations of angina pectoris varies. Patients may experience up to five attacks per day or experience a sharp increase in symptoms every few months. If left untreated, angina at rest may develop against the background of exertional angina.
Are you experiencing symptoms of angina pectoris?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Place of MVS in the structure of IHD
Cardiovascular diseases (CVD) still maintain a leading position in the structure of mortality around the world [4, 5]. Thus, according to Rosstat data for 2021, mortality from CVD was 633 cases per 100 thousand population. A year earlier, this figure was 622.1 cases per 100 thousand population. The annual mortality rate from coronary heart disease (CHD) among the Russian population is 27%. However, only 40–50% of patients with coronary artery disease know about their disease and receive comprehensive treatment. In more than half of hospitalized patients diagnosed with acute coronary syndrome, coronary angiography reveals unchanged coronary arteries, which indicates a different origin of anginal pain, not excluding AVS [6]. It is now widely accepted that obstructive disease of the epicardial arteries is not the only cause of myocardial ischemia [7, 8]. In a retrospective analysis of the NCDR Cath registry, only 37.6% of patients were diagnosed with obstructive epicardial artery disease, while 69% of patients were confirmed to have transient myocardial ischemia using noninvasive diagnostic tests [9]. It should be noted that chest pain with intact coronary arteries is not always a consequence of MVA, therefore, diagnostics require the use of high-resolution optical systems.
Pathophysiology of coronary microvascular dysfunction (CMD)
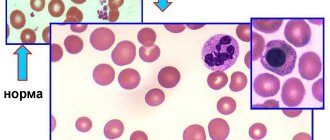
The myocardium is an aerobic muscle tissue that requires a continuous supply of oxygenated blood to produce the energy needed to maintain the pumping function of the heart. Under basic cardiac conditions, 60–70% of the required oxygen can be obtained from arterial blood, so the increased myocardial oxygen demand can only be met by increasing coronary blood flow. The proximal coronary bed consists of epicardial arteries with a diameter of 5 to 0.5 mm and gives rise to intramural vessels. The distal coronary bed is represented by prearterioles, arterioles with a diameter of 40 to 400 μm and capillaries with a diameter of less than 10 μm, which constitute the main coronary circulatory system [10]. At rest, the tone of the coronary microvasculature is high, but arteriolar diameter can change rapidly, responding to increased myocardial oxygen demand and increasing coronary blood flow [11]. Capillaries and venules are an important component of the coronary microcirculation, therefore, structural and functional disorders at this level (for example, a drop in blood pressure in the capillary network or microembolization) can cause the development of myocardial ischemia. Depending on the clinical picture, different pathogenetic mechanisms of microvascular dysfunction are distinguished (Table 1) [12].
According to A. Faccini et al., inflammation is another potentially important cause of the development of CMD [13]. Coronary microvascular spasm, originally described in [14], can, like epicardial spasm, cause myocardial ischemia in the absence of increased myocardial oxygen demand and initiate resting angina. Today, there is no doubt that MWS is a heterogeneous syndrome, the development of which may be based on various pathogenetic mechanisms. Proposed mechanisms of CMD include altered regulation of coronary microcirculation by the autonomic nervous system and generalized vascular disorders. Thus, in one of the large studies by P. Ong et al. [15, 16] during testing of patients for acetylcholine, every fourth patient experienced microvascular spasm, characterized by ischemic changes on the ECG without visible changes in the diameter of the epicardial coronary arteries. AL Arrebola-Moreno et al. [17] reported that coronary microvascular spasm induced by intracoronary acetylcholine leads to disturbances in myocardial perfusion and contractility. In the VR study, Taqueti et al. [18] found a direct connection between CMD and the development of heart failure in patients with preserved ejection fraction. However, in most cases, MWS develops as a result of isolated CMD [19], which is the only (or predominant) mechanism responsible for the development of an attack of angina or asymptomatic myocardial ischemia [20].
Treatment
Therapy begins with the elimination of all provoking factors that can affect the condition of a person suffering from the pathology. The attacks are controlled by taking nitroglycerin. After making a diagnosis, the cardiologist can prescribe the patient long-acting nitrates, antiplatelet agents, calcium channel blockers and beta-blockers.
The persistence of symptoms during conservative treatment becomes a reason to refer a child or adult for surgery. During the intervention, surgeons perform stenting of the coronary arteries and perform endovascular angioplasty. Clinical recommendations provide for the possibility of coronary artery bypass grafting against the background of exertional angina. The effectiveness of surgical treatment is 90-95%.
Clinical picture and diagnosis of MWS
MWS is characterized by a triad of symptoms: 1) typical angina caused by physical activity, in combination or in the absence of rest angina and shortness of breath; 2) the presence of signs of myocardial ischemia according to electrocardiography (ECG), Holter monitoring (HM), stress tests in the absence of other diseases of the cardiovascular system; 3) unchanged or slightly changed coronary arteries (arterial stenosis less than 50%) [21]. Angina attacks can occur quite often, up to several times a week, but remain stable. Pain occurs both during physical activity, emotional stress, and at rest and is poorly relieved by nitrates. Thus, MVA is a form of chronic angina and, according to ICD-10, belongs to code I20.8 “Other forms of angina.”
There are 4 clinical criteria to suspect MWS [22]:
clinic of myocardial ischemia: anginal attacks or equivalent symptoms (for example, shortness of breath) during exercise or at rest;
absence of obstruction of the coronary arteries: narrowing of the artery lumen by 50% or less or fractional blood flow reserve of more than 0.8, according to computed tomography or invasive coronary angiography;
objective confirmation of myocardial ischemia (ischemic changes on the ECG at the time of the attack); anginal pain, ischemic changes on the ECG and/or echocardiographic study (EchoCG), decreased myocardial perfusion during stress tests;
confirmation of microvascular disorders: coronary blood flow reserve less than 2.0–2.5 (depending on the measurement technique); microvascular spasm during an acetylcholine test (ischemic changes on the ECG in the absence of epicardial spasm); increase in microvascular resistance indicators; slowing of coronary blood flow with a TIMI score of 25 or more.
If all 4 criteria are present, the diagnosis of MWS is most convincing. The presence of criteria 1 and 2 indicates the possibility of MVS, but MVS can be diagnosed only by obtaining objective evidence of myocardial ischemia (criterion 3) or impaired coronary microvascular function (criterion 4).
Myocardial ischemia is usually diagnosed by performing stress tests (the most commonly used are bicycle ergometry (VEM), treadmill test and 24-hour HM) by identifying horizontal depression of the ST segment more than 1 mm from the J point on the ECG [23]. It is very important to understand that the diagnosis of MBC in patients with chest pain should not be made solely by exclusion based on the results of coronary angiography. An integrated approach is required, taking into account all non-invasive and invasive research methods to verify myocardial ischemia [24]. Clinical guidelines suggest the following algorithm for confirming myocardial ischemia. The diagnosis is made on the basis of a combination of complaints, medical history (cardiovascular risk factors), and detected hidden coronary insufficiency. If angina is suspected, it is recommended to calculate the pre-test probability of coronary artery disease based on the nature of chest pain, age and gender of the patient [25]. However, a number of large studies in recent years have shown that this approach leads to a significant overestimation of the risk of coronary artery disease and is accompanied by the prescription of unnecessary additional diagnostic tests.
All patients with suspected coronary heart disease undergo an ECG as a first step [26]. In uncomplicated ischemic heart disease, specific signs of ischemia without exercise are most often absent. The only fairly specific sign is the appearance of a Q wave after a myocardial infarction. Isolated changes in the T wave are not very specific and are most often not taken into account. When performing an ECG with exercise, a specific sign of myocardial ischemia is horizontal or oblique depression of the ST segment with a depth of at least 0.1 MV, duration of at least 0.06–0.08 s from the J point in one or more ECG leads. Signs of vasospasm include transient elevation of the ST segment by at least 0.1 MV in two or more leads [27]. However, the sensitivity of the method decreases in patients with cicatricial changes on the ECG, with intraventricular blockades and left ventricular (LV) hypertrophy. I would like to note that a stress ECG test on a bicycle ergometer or treadmill is not informative in cases of complete blockade of the left bundle branch, the presence of a pacemaker and WPW syndrome, in which changes in the ST segment cannot be interpreted. In addition, false-positive results are often found in patients with resting ECG changes due to LV hypertrophy, electrolyte imbalance, rhythm and conduction disturbances [28].
All patients with coronary heart disease or suspicion of it are recommended to undergo echocardiography, which allows assessing the systolic and diastolic functions of the left ventricle, identifying valvular pathology, excluding hypertrophic cardiomyopathy, aneurysm of the ascending aorta, and congenital heart pathology [22, 26]. However, with MWS, local zones of hypokinesis are not recorded on echocardiography at rest due to the large number of small affected areas, but one of the early signs of IHD, namely microvascular dysfunction, may be impaired LV diastolic function [29]. Other disadvantages of echocardiography are the low quality of visualization of the basal segments of the LV and false-positive results for pathological changes in the apical region [30]. The presence of tachycardia/arrhythmia in a patient significantly complicates the interpretation of echocardiography results. It should be noted that the disadvantage of all ultrasound methods for studying myocardial blood flow is the dependence of the interpretation on the qualifications and experience of the specialist performing the study. The sensitivity of echocardiography at rest in detecting myocardial ischemia, according to various authors, is 7.5–26.7%. The absence of such a sign as impaired regional and global contractility in patients with MWS can be explained by the peculiarities of the spread of ischemia, when it is limited to individual small areas of the myocardium [31].
According to modern European and Russian recommendations, CM is recommended for patients with chest pain and suspected arrhythmia. 12-lead CM may be useful if vasospastic angina is suspected. The diagnostic value of this method for routine examination of a patient with suspected myocardial ischemia is low. ST segment depression on the resting ECG can be interpreted as a sign of transient ischemia. However, ST segment depression is not associated with a poor prognosis, does not provide additional information compared with stress testing, and is often not even confirmed as a sign of transient ischemia by imaging stress testing. It should be noted that ST segment depression on the resting ECG may be due to LV hypertrophy. In this regard, CM cannot be used for a reliable diagnosis of myocardial ischemia, since the results of the study do not exclude or confirm IHD, including MVS [5, 22].
Stress tests are very important for verifying latent forms of myocardial ischemia by provoking ischemia with pharmacological or physical stress. The options for stress testing are varied. During their implementation, the myocardial oxygen demand increases (treadmill test, VEM, dobutamine test) or oxygen delivery to the myocardium decreases (tests with dipyridamole and adenosine) [22, 29].
The treadmill test is a more physiological method and has advantages over VEM due to the ability to dose-increase the load using the standard Bruce protocol to values greater than with VEM. A reliable sign of myocardial ischemia when performing VEM is horizontal or oblique ST segment depression of 1 mm or more [5]. The probability of diagnosing coronary artery disease is close to 90% if, during exercise, depression of the ST segment of the ischemic type reaches 2 mm or more and is accompanied by a typical attack of angina. VEM is indicated only for patients who are able to perform adequate physical activity on an exercise bike. Therefore, VEM is not possible if the patient has joint diseases or significant stenosis of the arteries of the lower extremities. Due to the relatively low sensitivity of VEM for ischemic heart disease, its negative result also does not exclude this diagnosis. The rate of false-positive results reaches 15% [24, 25]. Numerous studies have reported lower sensitivity of VEM and higher false-positive rates in women compared with men. The sensitivity and specificity of the treadmill test and VEM are approximately the same. False-negative tests lead to underestimation of angina symptoms.
Compared to stress ECG tests, stress echocardiography is more preferable. This is one of the most informative and cheapest methods for non-invasive diagnosis of myocardial ischemia, which has proven its high diagnostic value [32]. This method can be applied using all stress agents and has high sensitivity (80–85%) and specificity (84–86%) in the diagnosis of stenoses exceeding 50%. The capabilities of radioisotope methods in detecting MVS are being widely studied, but so far they have not become routine due to their complexity and high cost [21].
An important place in the diagnosis of cardiac arrest is occupied by positron emission tomography (PET) of the heart with stress testing [33]. According to most experts, PET of the heart at rest is not very informative. Disruption of myocardial blood flow can only be detected under conditions of functional load, which makes it possible to detect a decrease in blood flow in areas of the myocardium caused by endothelial dysfunction or vasospasm of the microvascular bed [34]. The distribution of the radiopharmaceutical against the background of stress allows us to identify even small areas of the LV in which myocardial hypoperfusion is noted. There are different types of stress tests: exercise test on a bicycle ergometer or treadmill, pharmacological test with vasodilators, transesophageal pacing and cold test. In clinical practice, during PET perfusion studies with 13N-ammonium, a pharmacological test with adenosine is most often used. According to the literature, PET using pharmacological stress tests has high specificity (78–100%) and sensitivity (87–97%) in the diagnosis of myocardial ischemia [33, 34]. The PET method, like single-photon emission computed tomography (SPECT), provides information about the presence or absence of myocardial ischemia, its location and severity, and scar changes. At the same time, PET, unlike SPECT, is characterized by higher image quality, has unique capabilities for calculating blood flow (in ml/min/g), which allows non-invasive assessment of blood flow reserve and provides a lower radiation dose. However, PET is generally less used due to its low availability and high cost. To date, studies are being conducted combining the PET method with intravenous pharmacological load. The radiopharmaceutical adenosine triphosphate, available on the pharmacological market, is used as a load; it has proven itself as a vasodilator, has a short decay period, and rarely causes side effects. The use of dobutamine seems inappropriate for MWS, since the expected effects of decreased myocardial contractility due to the ischemia it causes are extremely rare, as is the case with the use of stress echocardiography [21, 23]. The diagnosis of vasospastic angina is made on the basis of transient ischemic changes in the ST segment during an attack of angina (characteristic rises in the ST segment during an attack). To exclude vasospastic angina, it is possible to provoke coronary spasm during coronary angiography [35] by administering acetylcholine chloride [23]. The test for vasospasm is considered positive if: a) an anginal attack occurs; b) ischemic changes on the ECG; c) pronounced vasoconstriction of the epicardial arteries [36]. If a test with acetylcholine is accompanied by pain and ischemic changes on the ECG, but there is no spasm of the epicardial arteries, then we can talk about vasoconstriction at the level of the microvasculature.
Treatment of MVS
Treatment of MWS includes standard therapy for coronary artery disease: β-blockers, nitrates, calcium antagonists, statins, antiplatelet agents, second-line drugs (angiotensin-converting enzyme (ACE) inhibitors, nicorandil, ivabradine, ranolazine, trimetazidine), non-drug treatments (spinal cord stimulation, psychotherapy) [37].
Traditional antianginal drugs are prescribed in the first stages of treatment. Short-acting nitrates are recommended to relieve anginal attacks, but they often have no effect. Thus, only less than 50% of patients noted an improvement in their condition when using sublingual nitroglycerin. Conversely, nicorandil, which opens potassium ATP channels and has nitrate-like effects, has been reported to have a beneficial effect in MWS [38].
In patients with dominant symptoms of angina pectoris, therapy with β-blockers, which have been proven to eliminate the symptoms of angina pectoris, seems rational. These are the drugs of first choice, especially in patients with obvious signs of increased adrenergic activity (high heart rate at rest or during exercise) [39]. However, patients with microvascular or epicardial spasm should use caution when using β-blockers (especially those lacking vasodilatory properties) because these drugs may increase coronary vasoconstriction by masking α-adrenergic receptors in the coronary vessels [37].
Another drug that reduces myocardial oxygen demand due to its rate-lowering effects is ivabradine [40]. Calcium antagonists as first-line drugs are indicated in case of variability in the threshold of angina pectoris, especially in the angiospastic genesis of myocardial ischemia. Patients with clinical signs of MWS and lipid metabolism disorders are shown statins, which are known to have a positive effect on endothelial function. ACE inhibitors improve exercise tolerance and relieve angina symptoms [41]. The positive effect of ranolazine on endothelial function is known. In the work of E. Rayner-Hartley et al. [42] assessed the effect of ranolazine on the quality of life of patients with severe refractory angina caused by MVA. Patients received ranolazine at a dose of 1000 mg/day together with sulodexide for 4 weeks. The use of ranolazine improved the quality of life and reduced the number of visits to medical care. To correct endothelial dysfunction, trimetazidine is also used, which improves the metabolism of cardiomyocytes during myocardial ischemia. In the study by S.A. Boldueva et al. [43] showed the effectiveness of using trimetazidine in patients with MWS, in addition to standard antianginal therapy, with improvement in the clinical picture, quality of life, myocardial perfusion and endothelial function.
Unfortunately, traditional therapy for MWS is not always effective; the quality of life remains low due to pain, and patients are often hospitalized. Therefore, all patients with MWS require active correction of traditional risk factors, such as hypertension, diabetes mellitus, smoking, obesity, sedentary lifestyle, and hyperlipidemia.
Treatment of Prinzmetal's angina
A course of medication that affects both the symptoms of the disease and its causes can help cope with attacks and reduce their regularity. Clinical recommendations for Prinzmetal angina include:
- taking drugs from the category of calcium antagonists in combination with long-term nitrates;
- anti-alpha adrenergic drugs that prevent coronary artery spasm;
- a course of antioxidant vitamins C and E;
- other medications that promote the natural elasticity of blood vessels and maintain their conductive capacity.
If a conservative course turns out to be ineffective, doctors resort to surgical intervention. More often this is coronary angioplasty with stenting, less often cardiac denervation with plexectomy simultaneously with coronary bypass surgery. A decision may be made to implant an automatic defibrillator or pacemaker.