Strokes
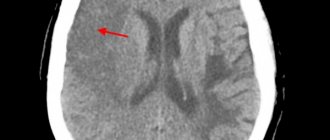
This term refers to rupture of an artery followed by hemorrhage. This is a very dangerous condition in which the cerebral cortex is damaged by a growing hematoma with subsequent loss of function. According to ICD 10, there are three codes corresponding to stroke:
- I 60 - indicates hemorrhage into the space that is located between the membranes of the brain, called subarachnoid. According to further gradation, it includes five varieties (0-4) depending on the vessel whose rupture caused the stroke. The next digit is written after the period;
- I 61 – damage to parenchymal tissue. This means that the vessel has ruptured inside the hemispheres or brain stem, damaging the white or gray matter. Further classification also includes five types depending on the location of the lesion;
- I 62 – stroke, the localization of which could not be identified. The doctor is sure that the patient has a hemorrhage, but it is impossible to determine the location and area of the lesion for a number of reasons. Includes three subclasses.
The consequences of stroke of the hemorrhagic type are described in the headings of ICD 10 - these are residual effects after hemorrhage, which often lead to disability. These are very dangerous conditions, during which there is a high mortality rate; about a third of patients die in the first 5 years of life.
Help without delay. Beware, spinal stroke!
Numbness of the skin, impaired movement in the leg... One of the diseases in which such manifestations occur is stroke. The connection is firmly established in the mind: if there is a stroke, it means the brain.
However, it can also be spinal, affecting the “main cable” of the body - the spinal cord. We are talking with Irina Vladimirovna Vlasova, a neurologist at the Expert Voronezh Clinic, about this pathology. Spinal stroke is the topic of our interview.
— Irina Vladimirovna, now in many cities of Russia there is a campaign aimed at informing people about the first signs of a stroke. But in addition to cerebral stroke, there is an equally dangerous disease - spinal stroke. Tell me what it is?
This is an acute disorder of spinal circulation, which can develop due to compression, blockage or rupture of the spinal artery. In this case, two scenarios are possible: ischemia or hemorrhage. Based on this, spinal stroke is divided into ischemic and hemorrhagic. The first form is more common.
Read material on the topic: Ischemic and hemorrhagic stroke: what is the difference?
— Is spinal stroke reflected in ICD-10?
Yes, its code is G95.1
— How often does this pathology occur among Russians and who is at risk?
It is relatively rare: in the structure of neurological diseases it accounts for 1-1.5%. The risk of occurrence in women and men is generally the same. Most often, this diagnosis is made in the age range of 30-70 years.
IN THE STRUCTURE OF NEUROLOGICAL DISEASES, SPINAL STROKE IS 1-1.5%
What are the causes of spinal stroke? There are several groups, including:
- pathological changes in the vessels supplying blood to the spinal cord (can be congenital - for example, aneurysms, malformations, underdevelopment, and acquired - for example, atherosclerosis);
Read the material on the topic: Will traditional methods of treatment help in the treatment of atherosclerosis?
- processes leading to compression of blood vessels supplying the spinal cord from the outside (tumors, other space-occupying formations in the chest or abdominal cavity, enlarged lymph nodes, vertebral fragments due to injuries);
- complications that arise during operations on the spine or nearby vessels (in particular, on the aorta).
WHEN SYMPTOMS OF A SPINAL STROKE APPEAR, A PERSON NEEDS URGENT MEDICAL CARE AND EMERGENCY HOSPITALIZATION TO A VASCULAR CENTER. CALL AN AMBULANCE
Most often, this pathology develops due to a combination of several factors.
— What are the symptoms of a spinal stroke?
Signs appear quite quickly (from several minutes to several hours, less often - days). They are quite diverse, which is explained by the location of the lesion and its prevalence.
At the level and below the site of the lesion, disturbances in movement (paresis), sensitivity and functions of the pelvic organs are noted.
Ischemic stroke develops more often against the background of “precursors”. These can be various short-term sensitivity disorders (numbness, tingling, mainly in the lower extremities), transient motor disturbances in the form of paresis.
With a hemorrhagic spinal stroke, severe pain in the spine is noted, with radicular symptoms, as well as the motor and other disorders listed above.
— What should be done if there are signs of a spinal stroke? What is first aid?
If a person experiences any of the above symptoms, he needs urgent medical care and emergency hospitalization at a vascular center. Call an ambulance.
— In order to help a patient with a cerebral stroke, doctors have only four hours. How quickly should a patient with suspected spinal stroke be admitted to hospital?
We are talking about the so-called “therapeutic window”. It is up to 4-6 hours (the sooner the better). The sooner help is provided, the smaller the area and severity of the lesion will be.
After this time, the chances of reversing the changes that occur decrease.
— What is included in the “gold standard” for diagnosing spinal stroke?
A collection of complaints and medical history and a neurological examination are required.
Computed and magnetic resonance imaging, spinal angiography, lumbar puncture and electroneuromyography are used.
You can sign up for an MRI of the spine here
A general and biochemical blood test, coagulogram (study of the characteristics of the blood coagulation system), glucose and lipid levels are performed. Consultations with other specialists are carried out.
— What diseases are differentiated between spinal strokes?
The range of pathologies for differential diagnosis includes acute inflammation of the spinal cord, its tumors and space-occupying formations, epidural abscesses, and syringomyelia.
— How is spinal stroke treated? What are its principles?
Regardless of its type, nonspecific therapy is carried out aimed at reducing edema, maintaining metabolic processes in nerve cells, and preventing complications.
For ischemic spinal stroke, neuroprotective therapy is carried out, anticoagulants and antiplatelet agents are prescribed.
If this is a hemorrhagic spinal stroke, drugs are used to stop the bleeding, and, if indicated, surgery is performed to eliminate its source.
— Irina Vladimirovna, what is the prognosis for patients with spinal stroke? Has modern medicine learned to successfully treat this disease and rehabilitate such patients?
This pathology has a mostly favorable outcome, but sometimes it can result in disability or death. This can be, in particular, in case of malignant tumors, a severe general somatic background (for example, the presence of diabetes), or the addition of an infection (for example, the development of pneumonia).
The outcome is also influenced by factors such as the cause that led to the development of the stroke, the anatomical and physiological characteristics of the “bypass” blood circulation. Early treatment improves the prognosis of the disease.
SPINAL STROKE MOSTLY HAS A FAVORABLE OUTCOME. EARLY TREATMENT IMPROVES THE DISEASE PROGNOSIS
Recovery after a spinal stroke is ensured by rehabilitation measures. Early rehabilitation includes the use of physical therapy, kinesiotherapy and physiotherapy, massage, and ergotherapy.
The success of rehabilitation also depends on the extent of damage to the spinal cord tissue and the timeliness of seeking help (within the “therapeutic window”).
— Our material will be incomplete if we do not talk about disease prevention. How to avoid spinal stroke?
Its prevention lies in timely diagnosis and treatment of vascular pathologies; detection and elimination of malformations, aneurysms; treatment of intervertebral hernias; prevention of spinal column injuries.
Read material on the topic: What are hernias and protrusions of the spine?
It is important to lead an active lifestyle, normalize weight, eat rationally, and get rid of bad habits.
Other materials on topics:
Let's pull and pull! Who can benefit from spinal traction?
What will an MRI of the spinal column show?
For reference:
Vlasova Irina Vladimirovna
Graduate of the Faculty of General Medicine of the Voronezh State Medical Academy in 2007.
From 2007 to 2009 she completed clinical residency in the specialty “Neurology”.
Currently holds the position of neurologist at Clinic Expert Voronezh. Receives at the address: st. Pushkinskaya, 11.
Heart attacks
This is an acute condition characterized by blockage of the lumen of the artery or its sharp spasm, followed by impaired circulation and the appearance of an area of tissue necrosis (scientifically called necrosis).
Code 63 corresponds to the ICD 10 code for stroke of ischemic type, the gradation is as follows:
- thrombosis of arteries in the neck and base of the skull - corresponds to the number 0, embolism - 1, unspecified rupture - 2;
- thrombosis of cranial arteries - coded 3, embolism - 4, unspecified etiology - 5;
- vein rupture – 6;
- unknown and other heart attacks are marked with numbers 8 and 9.
All of the listed sub-clauses of the classification are placed after the dot; if, for example, the veins are damaged, the code will look like this: I 63.6. Heart attacks are very dangerous; according to statistics, about 80% of all strokes are ischemic. Such patients are hospitalized in the intensive care unit and are under the supervision of a doctor.
Blockages and spasms of blood vessels without heart attack
In clinical practice, there are often cases where disruption of blood flow does not cause necrotic changes. According to ICD 10, such conditions are included in two large groups:
- I 65 – includes damage to the carotid, vertebral and basilar arteries emerging from it;
- I 66 – this code indicates spasm or embolism of the cerebral and cerebellar arteries.
Nerve cells are very sensitive and quickly die due to oxygen starvation and lack of nutrients. But the brain is structured in a unique way; it contains the so-called “Circle of Willis” - these are “spare” connections between arteries, thanks to which blood can flow through bypass vessels. That is why sometimes obstruction does not lead to cerebral infarction.
Let us note the main reasons that can create an obstruction in the artery:
- Spasm is a narrowing of a vessel due to contraction of its muscles, resulting in a decrease in its capacity. Usually the cause is neurogenic;
- Narrowing - differs from the previous version by violating the anatomical integrity of the vascular wall in a certain area. Such changes are irreversible;
- Thrombosis is the formation of a blood clot on the artery wall, which gradually increases in size and creates an obstruction;
- Embolus - circulates along with the blood, enters a vessel of a smaller caliber and causes its blockage. Usually this is a detached blood clot or atherosclerotic plaque.
The listed reasons often lead to cerebral infarctions or the development of severe conditions after stroke, having a certain code according to ICD 10.
From 01/01/22, the official version of the International Classification of Diseases of the World Health Organization becomes its 11th revision (ICD-11), which received more than 10 thousand changes compared to ICD-10. Currently, ICD-11 is considered a preliminary version and is for informational purposes only, with the possibility of editing the classification as a result of ongoing discussion. At the same time, the remaining period of time until the beginning of 2022 is necessary to translate the classification into different languages and prepare national health systems for its practical application. A service platform has been created for developers and translators with the ability to visualize the classification structure. ICD-11 is a fully electronic version and can be integrated with electronic health and information systems applications [1].
The structure of ICD-11 is represented by 26 chapters with codes for diseases, health-related conditions, and external causes of disease or death. Chapter numbers in ICD-11 will now be in Arabic numerals instead of ICD-10 Roman numerals. The codes for the first 9 chapters begin with a number corresponding to the chapter number (1-9), the codes for the next 17 chapters begin with a Latin letter in alphabetical order (AS). Diseases of the nervous system make up Chapter 08 (08 Diseases of the nervous system), and the section on cerebrovascular diseases has been returned to this chapter in ICD-11 (Table 1) .
Table 1. Section 8B0-8B2 Cerebrovascular diseases, chapter 08 “Diseases of the nervous system” ICD-11
Compared to ICD-10, this section has undergone certain changes (Table 2) . Subarachnoid, intracerebral and other non-traumatic intracranial hemorrhage are now combined under the rubric “Intracranial hemorrhage”. Instead of the “Cerebral Infarction” heading, the “Cerebral Ischemia” block was introduced, which includes transient ischemic attacks, cerebral ischemic strokes and other definite and undetermined cases of cerebral ischemia. For the first time in ICD-11, a new heading “Cerebrovascular disease without acute cerebral symptom” has appeared, including “silent” cerebral infarctions, microhemorrhages and other definite and undetermined cerebrovascular diseases without acute cerebral symptoms. The heading “Hypoxic-ischemic encephalopathy” was created as a separate heading, corresponding to code G93.1 “Anoxic brain damage, not classified in other headings” ICD-10.
Table 2. Comparison of codes for cerebrovascular diseases in ICD-10 and ICD-11
Note. * - left in Chapter 11 Diseases of the circulatory system.
The entire block “Intracranial hemorrhage” of non-traumatic etiology in ICD-11 is presented as follows:
8B00 Intracerebral haemorrhage - I61 in ICD-10;
8B00.0 Deep hemispheric hemorrhage - I61.0 in ICD-10;
8B00.1 Lobar (hemispheric lobar) hemorrhage (Lobar haemorrhage) - I61.1 in ICD-10;
8B00.2 Hemorrhage in the brainstem (Brainstem haemorrhage) - I61.3 in ICD-10;
8B00.3 Hemorrhage into the cerebellum (Cerebellar haemorrhage) - I61.4 in ICD-10;
8B00.4 Intraventricular hemorrhage without parenchymal hemorrhage - I61.5 in ICD-10;
8B00.5 Hemorrhage of multiple sites - I61.6 in ICD-10;
8B00.Z Intracerebral haemorrhage, site unspecified - I61.9 in ICD-10;
8B01 Subarachnoid hemorrhage - I60 in ICD-10;
8B01.0 Aneurysmal subarachnoid hemorrhage (Aneurysmal subarachnoid haemorrhage) - I60.0-I60.8 in ICD-10;
8B01.1 Non-aneurysmal subarachnoid hemorrhage - no direct equivalent in ICD-10;
8B01.2 Subarachnoid hemorrhage not known if aneurysmal or non-aneurysmal - I60.9 in ICD-10;
8B02 Nontraumatic subdural hemorrhage - I62.0 in ICD-10;
8B03 Nontraumatic epidural hemorrhage - I62.1 in ICD-10;
8B0Z Intracranial hemorrhage, unspecified - I62.9 in ICD-10.
Clinical conditions coded in the Cerebral Ischemia block include transient ischemic attacks, cerebral ischemic strokes, and other definite (8B1Y) and undetermined (8B1Z) cases of cerebral ischemia. The actual transient ischemic attack has code 8B10, which includes the following subheadings:
- 8B10.0 Transient blindness (Amaurosis fugax) - G45.3 in ICD-10;
— 8B10.Y Other specified transient ischemic attack;
- 8B10.Z Transient ischemic attack, unspecified - G45.9 in ICD-10.
At the same time, code 8B10.Y combines various clinical syndromes of transient cerebrovascular accidents in the carotid and vertebrobasilar systems, as well as transient ischemic attacks associated with subarachnoid hemorrhage, in contrast to ICD-10, in which carotid and vertebrobasilar arterial syndromes have separate codes (G45.1 and G45.0, respectively), as are transient global amnesia (G45.4) and multiple and bilateral precerebral artery syndromes (G45.2).
Subsection 8B11 “Cerebral ischemic stroke” corresponds to block I63 of ICD-10 and includes the following conditions in the form of 6 headings, 3 of which have subheadings:
8B11.0 Cerebral ischemic stroke due to extracranial large artery atherosclerosis - I63.0 in ICD-10;
8B11.1 Cerebral ischemic stroke due to intracranial large artery atherosclerosis - I63.3 in ICD-10;
8B11.2 Cerebral ischemic stroke due to embolic occlusion - I63.1 and I63.4 in ICD-10:
8B11.20 Cerebral ischemic stroke due to cardiac embolism;
8B11.21 Cerebral ischemic stroke due to aortic arch embolism;
8B11.22 Cerebral ischemic stroke due to paradoxical embolism;
8B11.2Y Cerebral ischemic stroke due to other specified embolic occlusion.
8B11.3 Cerebral ischemic stroke due to small artery occlusion - no equivalent in ICD-10;
8B11.4 Cerebral ischemic stroke due to other known cause - I63.8 in ICD-10:
8B11.40 Cerebral ischemic stroke due to global hypoperfusion with watershed infarct;
8B11.41 Cerebral ischemic stroke due to other non-atherosclerotic arteriopathy;
8B11.42 Cerebral ischemic stroke due to hypercoagulable state;
8B11.43 Cerebral ischemic stroke in association with subarachnoid hemorrhage;
8B11.44 Cerebral ischemic stroke from dissection.
8B11.5 Cerebral ischemic stroke of unknown cause:
8B11.50 Cerebral ischemic stroke due to unspecified occlusion or stenosis of extracranial large artery - I63.2 in ICD-10;
8B11.51 Cerebral ischemic stroke due to unspecified occlusion or stenosis of intracranial large artery - I63.5 in ICD-10;
8B11.5Z Cerebral ischemic stroke, unspecified - I63.9 in ICD-10.
Intracranial large arteries are represented by the siphon of the internal carotid artery, the anterior, middle and posterior cerebral, vertebral and basilar arteries. Rubric 8B11.3 “Cerebral ischemic stroke due to occlusion of a small artery” actually does not have an exact analogue in ICD-10 and includes such definitions as lacunar infarction and lacunar stroke. However, to code a specific lacunar syndrome, you can use additional codes from a separate block 8B26 “Cerebral vascular syndromes in cerebrovascular diseases” in the heading 8B26.5 “Lacunary syndromes” with appropriate detail in the form of an additional code after the 5th digit:
— 8B26.50 Pure motor lacunar syndrome — G46.5* in ICD-10;
— 8B26.51 Pure sensory lacunar syndrome — G46.6* in ICD-10;
— 8B26.5Y Other specified lacunar syndromes;
— 8B26.5Z Lacunar syndromes, unspecified.
In the heading 8B11.4 “Cerebral ischemic stroke due to other known causes”, stroke due to global hypoperfusion with infarction of the watershed zone (zone of adjacent blood supply) and stroke due to hypercoagulation are distinguished, corresponding in essence to the terms “hemodynamic stroke” and “stroke by type of hemorheological microocclusion” in the Russian Federation classification of the Research Institute of Neurology of the Russian Academy of Medical Sciences [2].
On average, about 30% of all cases of cerebral infarction (cryptogenic stroke), including stroke due to multiple potential causes, fall into the heading 8B11.5 “Cerebral ischemic stroke due to multiple potential causes”.
This division of cerebral ischemic stroke in ICD-11 corresponds to the TOAST classification of stroke subtypes [3], which is the most widely used among various etiological classifications of cerebral stroke. The TOAST classification system defines criteria for ischemic strokes due to atherosclerosis of large extra- or intracranial vessels, cardioembolic causes from high- or intermediate-risk sources, small vessel disease, and other established causes. When a cause cannot be identified due to incomplete workup or when there are multiple competing causes, the condition is classified as stroke of unknown etiology (accounting for about 30% of all cases), despite the possibility of cases with a clearly defined etiology within this cohort with several different potential causes of stroke [4, 5]. ].
In this case, the etiology of stroke is established based on the results of a neurological examination of the patient with an assessment of the main risk factors, determination of hematocrit, prothrombin time, platelet count, erythrocytes and leukocytes, brain imaging (CT/MRI), 24-hour electrocardiography, echocardiography and ultrasound examination of extra- and intracranial arteries. Extended diagnostic evaluation may include a comprehensive echocardiographic examination with transesophageal echocardiography, chest CT, and a complete assessment of the hemostatic system [5].
At the same time, attempts continue to develop more reliable classification systems for the causes of ischemic stroke with clearer criteria for determining their subtypes, including at the national level [6, 7]. It is also proposed to create a single combined (“causal” and phenotypic) classification system [ 8]. Thus, the CCS classification identifies patients with multiple causes of stroke in accordance with the most likely etiology of the cerebrovascular event [9]. The ESUS classification suggests that the most common stroke of unknown etiology is embolic, even if a thorough search for the cause does not reveal its underlying cause, which may be due to the presence of sources with a low risk of embolism. At the same time, the sources of embolism can be multiple. Embolic stroke of unknown source (ESUS) is a diagnostic subgroup of cryptogenic stroke [4, 10, 11]. In this vein, ICD-11 separately, along with cardiogenic embolism, distinguishes arterial and paradoxical (venous) embolism.
The SPARKLE classification proposes to distinguish large vessel disease taking into account the presence of atherosclerotic plaques, which reduces the proportion of strokes of unknown etiology and demonstrates the advantages of this system compared to the CCS and TOAST classifications. A very high so-called plaque load in the absence of hemodynamically significant stenosis of the internal carotid arteries (which is explained by their compensatory dilatation) correlates with a high 5-year risk of stroke, death or myocardial infarction and should be included in the diagnostic criteria for large vessel diseases [8]. The presence of non-stenotic atherosclerotic lesions of the carotid and vertebral arteries can cause arterial embolism, especially in the case of an irregularly shaped plaque or its ulceration [12,13]. Plaque load is calculated as the total cross-sectional area (sum of areas) of all plaques measured longitudinally in the common, internal or external carotid arteries on both sides [14].
The ASCO Phenotypic Classification of Stroke (later ASCOD) proposes a ranked assessment of the most likely causes of stroke (A - atherosclerotic large vessel disease, S - small vessel disease, C - cardiac causes, O - other causes, D - cerebral vessel dissection). At the same time, the ASCOD system records and evaluates all major diseases present in patients with ischemic stroke [15–18]. Application of the CCS and ASCO classifications to patients with transient ischemic attacks and minor strokes, as well as to young patients, reduces the number of cases with an undetermined etiology of a vascular event in these cohorts compared with the use of the “causal” TOAST classification [19–21].
If the patient's condition meets the criteria for a stroke and it is not possible to clarify the type of stroke using neuroimaging or other examination methods, code 8B20 “Stroke not known if ischemic or haemorrhagic”, corresponding to ICD-10 code I64, is used.
The new ICD-11 block 8B21 “Cerebrovascular disease without acute cerebral symptom” includes conditions that do not cause acute brain dysfunction and are detected by neuroimaging or autopsy. At the same time, they have strong links with the development of cognitive impairment, dementia and non-focal neurological symptoms such as gait, balance and voiding disorders, indicating their important clinical significance in terms of preventive measures. These conditions are based on cerebral microangiopathy and are represented by the following codes:
8B21.0 “Silent cerebral infarct”;
8B21.1 Silent cerebral microbleed;
8B21.Y Other specified cerebrovascular disease with no acute cerebral symptom;
8B21.Z Cerebrovascular disease with no acute cerebral symptom, unspecified.
In this case, code 8B21.Y includes changes in the white matter of the cerebral hemispheres of ischemic origin (leukoaraiosis), manifested by its hyperintensity on MRI. In ICD-10 it corresponds to code I67.3 “Progressive vascular leukoencephalopathy (Binswanger disease).”
In fact, rubric 8B11.3 “Cerebral ischemic stroke due to small artery occlusion” and block 8B21 “Cerebrovascular disease without acute cerebral symptom” combine most of the cerebral microangiopathies (cerebral small vessel disease).
Block I67 “Other cerebrovascular diseases” of ICD-10 has received significant revision, which has been transformed into block 8B22 “Some specified cerebrovascular diseases” of ICD-11, which includes other specific lesions of extra- and intracranial arteries and veins that can cause an acute cerebral episode or be asymptomatic, without acute focal brain dysfunction:
8B22.0 Dissection of cerebral arteries - I67.0 in ICD-10;
8B22.1 Cerebral venous thrombosis - I67.6 in ICD-10;
8B22.2 Cerebral vasoconstriction syndromes - no direct analogue in ICD-10;
8B22.3 Isolated cerebral amyloid angiopathy - no direct equivalent in ICD-10;
8B22.4 Intracranial vascular malformation - no direct equivalent in ICD-10;
8B22.5 Cerebral aneurysm, nonruptured - I67.1 in ICD-10;
8B22.6 Familial cerebral saccular aneurysm - no direct equivalent in ICD-10;
8B22.7 Cerebral arteritis, not elsewhere classified - I67.7 in ICD-10;
8B22.8 Hypertensive encephalopathy - I67.4 in ICD-10;
8B22.9 Migraine-induced stroke - no direct analogue in ICD-10;
8B22.A Subclavian steal syndrome - no direct analogue in ICD-10;
8B22.B Moyamoya syndrome - I67.5 in ICD-10;
8B22.C Hereditary cerebrovascular diseases - no direct analogue in ICD-10;
8B22.Y Other specified cerebrovascular disease - I67.8 in ICD-10.
In this case, code 8B22.7 includes primary cerebral arteritis/angiitis (8B22.70) and other specified (granulomatous arteritis of the nervous system, cerebral arteritis in infectious or parasitic diseases - 8B22.7Y) and unspecified (8B22.7Z) - cerebral arteritis, not classified elsewhere.
Code 8B22.C “Hereditary cerebrovascular diseases” unites various arteriopathies associated with different genetic defects - syndromes 8B22.C0 CADASIL (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy syndrome), 8B22.C1 CARASIL (cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy syndrome) and other specified (8B22.CY - associated with mutations of the COL4A1, TREX 1 and other genes) and unspecified (8B22.CZ) hereditary cerebrovascular diseases.
Code 8B22.Y, in addition to acute cerebrovascular insufficiency, also includes the syndrome of posterior reversible encephalopathy (not always combined with vasoconstriction) and cerebral necrosis - conditions that have no analogues in ICD-10.
Block 8B23 “Cerebrovascular disorders” (corresponding to block I68 of ICD-10) includes syndromes of brain damage in diseases that, in addition to the intracranial and extracranial arteries or the nervous system as a whole, also involve other parts of the vascular system or other body systems. These include cerebrovascular disorders in systemic and chronic diseases, cerebral stenosis or occlusion of cerebral arteries in infectious diseases, and secondary cerebral arteritis. Items in this section should be coded together with the primary classification code for the specific disease, including other diagnostic codes from the cerebrovascular disease block.
Codes from block 8B25 “Sequelae of cerebrovascular disease” (corresponding to block I69 of ICD-10) are applied 1 month or later after the onset of cerebrovascular disease:
8B25.0 Late effects of cerebral ischemic stroke - I69.3 in ICD-10;
8B25.1 Late effects of intracerebral haemorrhage - I69.1 in ICD-10;
8B25.2 Late effects of subarachnoid haemorrhage - I69.0 in ICD-10;
8B25.3 Late effects of other nontraumatic intracranial hemorrhage - I69.2 in ICD-10;
8B25.4 Late effects of stroke not known if ischemic or haemorrhagic - I69.4 in ICD-10;
8B25.Y Late effects of other specified cerebrovascular disease - I69.8 in ICD-10;
8B25.Z Late effects of cerebrovascular disease, unspecified—I69.8 in ICD-10.
Block 8B26 “Cerebral Vascular Syndromes in Cerebrovascular Diseases” provides additional codes added to the main diagnostic code to indicate the anatomical location of the brain lesion (corresponds to ICD-10 block G46*):
8B26.0 Brainstem stroke syndrome;
8B26.1 Cerebellar stroke syndrome;
8B26.2 Middle cerebral artery syndrome;
8B26.3 Anterior cerebral artery syndrome;
8B26.4 Posterior cerebral artery syndrome;
8B26.5 Lacunar syndromes;
8B26.Y Other specified vascular syndromes of brain in cerebrovascular diseases;
8B26.Z Vascular syndromes of brain in cerebrovascular diseases, unspecified.
Thus, in ICD-11, which officially comes into force on January 1, 2022, section 8B0-8B2 “Cerebrovascular diseases” is located in chapter 08 “Diseases of the nervous system”. The division of cerebral ischemic stroke in ICD-11 corresponds to the TOAST etiological classification of stroke subtypes. In order to develop more clear criteria for determining the subtypes of ischemic stroke and their causes, various authors have proposed other classification systems. It seems necessary to develop a new revision of the domestic classification of cerebrovascular pathology, consistent with ICD-11 codes.
The author declares no conflict of interest.
Remaining classification
We have listed the main gradation of cerebrovascular disorders, which are often encountered in clinical practice. Let us note the remaining pathologies, concomitant diseases and conditions after stroke, which correspond to their code according to ICD 10:
- I 64 – set when it is not possible to distinguish hemorrhage from ischemia;
- I 67 – cerebrovascular pathologies not related to strokes and heart attacks;
- I 68 – cerebrovascular accident in other diseases;
- I 69 – complications of stroke.