Publication date: September 12, 2019
Spinal stroke is a severe pathology caused by an acute disruption of blood flow to the spinal cord. It often becomes a cause of disability, especially if the patient is not provided with medical care in a hospital setting. Recovery after a spinal stroke can be quite lengthy.
Causes of ischemic spinal stroke
The causes of ischemic spinal stroke are divided into three categories:
- Causes associated with damage to the heart and blood vessels (occurs in 20-22% of cases).
- Reasons that cause compression of blood vessels from the outside (occurs in 75% of cases of the disease).
- Causes arising as a result of complications after medical procedures (5-7%).
Cases of damage to the heart and cardiovascular system are explained by the presence of anomalies in their structure, which is often congenital. In addition, lesions can also be acquired (most often, lesions of the vessels themselves).
The cause of the congenital disorder is usually underdevelopment of the spinal vessels, deviations in the normal development of the aorta, all kinds of aneurysms and varicose veins.
Among the most common causes of acquired lesions are:
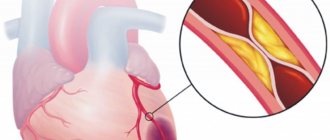
- atherosclerosis of vessel walls;
- blockage of the arterial lumen by blood clots;
- low blood pressure in the vessels that supply the spinal cord;
- heart failure;
- myocardial infarction.
As is known, compression from the outside occurs by squeezing the aorta or nearby vessels. Compression may occur due to a formation in the chest or abdominal cavity. The latter includes pregnancy, an increase in the size of the lymph nodes due to the spread of the tumor (metastasis) or lymphogranulomatosis.
If we talk about compression of the radicular cerebral arteries, then most often this occurs with a vertebral hernia, spinal cord tumor, or even with vertebral fractures.
In addition, ischemic spinal stroke also develops as a consequence of improper technique during surgical intervention in the spine or nearby tissues. Often this incorrect technique is considered to be prolonged squeezing with a surgical clamp, which is used to stop arterial bleeding. The cause of an acute disruption in blood circulation can be, for example, spinal anesthesia or blockade of the spinal nerve roots (usually this happens with radiculitis).
Precursor stage
The first stage, the precursor stage, can last from a few minutes to several months. A short stage is inherent in the case of unexpected and rapid blockage of blood vessels by blood clots or in the case of a pinched artery, which is often observed with spinal injuries.
Speaking about a longer period of this stage, a gradual and slow cessation of blood circulation is assumed (for example, in the case of tumor growth or an increase in the size of an atherosclerotic plaque).
Preceding symptoms of this disease may be:
- occasional lameness;
- pain in the spine area;
- numbness of the limbs;
- feeling of crawling “goosebumps”;
- discomfort in the direction of branching of the spinal roots.
Intermittent claudication in neurology is a condition in which the patient feels a characteristic numbness of the lower extremities, weakness when standing for a long time or walking for a long time. The latter is explained by the resulting oxygen starvation in the spinal region, which is responsible for the mobility of the legs. In addition, the cause of such lameness may be poor blood circulation in the vessels.
Development of stroke
The process of development of ischemic spinal stroke will always depend on the reasons that caused the arrest of blood circulation in the spinal cord. If the latter occurred due to a detached blood clot, then symptoms will develop literally over the next few minutes. In other cases, symptoms will appear completely within a few hours.
Further symptoms of a developing ischemic stroke will depend on which particular vessel has stopped the flow of blood to the spinal cord. If there is a blockage of the spinal artery, then paralysis of the limbs begins, the normal activity of the bladder and intestines is disrupted, the skin becomes not as sensitive as before, especially on the arms and legs.
If the main focus of the stroke is concentrated in the cervical spinal cord, then the patient is characterized by a flaccid type of paralysis in the upper limbs, which is usually accompanied by a decrease in muscle tone. Spastic paralysis may also occur in the lower extremities, which is characterized by increased muscle tone. In case of damage to the thoracic spinal cord, paresis of the legs or flaccid paresis of the legs with fecal retention begins (if the lesion is localized in the lumbosacral region).
Features of hemorrhagic manifestations
Hemorrhage is possible into the substance of the spinal cord (hematomyelia) or under the membranes (hematorachis). Clinical manifestations depend on the size of the hematoma.
Hematomyelia is characterized by:
- acute girdling pain in the torso;
- paralysis of one or all limbs;
- impaired pain and temperature sensitivity in the extremities;
- massive hemorrhage causes changes in the functioning of the pelvic organs.
Tematorahis is a rare pathology in which blood enters the intrathecal space. Most often due to injury or rupture of an aneurysm. Calls:
- sharp shooting pains;
- accompanied by symptoms of brain damage that last for several days.
It is important that there are no manifestations of damage to the brain substance.
With an epidural location of the hematoma, the pain is localized in a certain part of the spine, intensifies as blood accumulates, and is prone to repetition.
Reverse development
The stage of reverse development of symptoms begins a month after the onset of the disease. This stage is characterized by a fragmented restoration of blood supply in the area that was damaged. Recovery occurs due to the flow of blood into the arteries from other large vessels. There is also a restoration of the functions of neurons that remained as intact as possible at the site of the stroke.
As for the reverse development, it is characterized by a slow decrease in sensitivity, the return of some movements inherent in the limbs and the resumption of the work of the pelvic organs. The speed of this process, as well as the extent of restoration of lost function, will depend on the location of the ischemic stroke in the spinal cord.
Major complications
The most common complication of a spinal stroke is motor impairment and limited mobility of the muscle group innervated by the affected area of the spinal cord. The person loses the ability to move independently or suffers from lameness. If a large area of the spinal cord is affected, complete paralysis may develop, in which the patient becomes bedridden. Paralysis is fraught with the development of complications such as bedsores and pneumonia.
If pelvic functions are disrupted, the patient may experience consequences such as urinary dysfunction, fecal incontinence and impotence.
Disability is often a consequence of a spinal stroke
Diagnosis of ischemic spinal stroke
It is usually difficult to diagnose ischemic spinal stroke, since its appearance resembles poliomyelitis, multiple sclerosis, syringomyelia, and abnormalities in the structure of the cerebellum.
It is very important during diagnosis to study in detail the preceding factors and the rate of development of symptomatic signs. All signs will help to establish the cause of the development of circulatory disorders in the spinal cord.
Understanding which segment of the spinal cord is responsible for certain movements or for the sensitivity of parts of the body allows us to determine the localization of the source of the stroke.
To confirm the diagnosis of ischemic spinal stroke, an MRI or CT scan of the spinal cord is performed; myelography, spondylography, or an electrophysiological study may be prescribed.
Through angiography, it is possible to detect which particular lumen of the blood vessel has been narrowed or which one has become blocked. With the help of CT and MRI, you can very accurately determine the level of the stroke that has affected the spinal cord.
Myelography is an excellent diagnostic method that allows you to detect compression of blood vessels by a tumor located in the spinal cord, as well as intervertebral herniation or vertebral fragments (often after injury). Electrophysiological studies such as ENG and EMG are carried out to determine disruptions in muscle innervation.
How is rehabilitation carried out?
Rehabilitation of a patient with a spinal stroke necessarily includes increased physical activity. Gradual exercises, first using passive flexion and extension of the limbs, then connecting devices for dosed loading. It is best to place the patient in a rehabilitation center after inpatient treatment, where he will learn a minimum of independent exercises.
Learning to walk begins with the use of walkers, then moves on to canes.
To overcome muscle weakness, electrical stimulation, massage, acupuncture, underwater shower, and ozokerite applications are prescribed.
Some patients need to be taught self-care. The most suitable period for rehabilitation is the first six months. Then you should take repeat courses twice a year. Positive changes are possible within three years, so any despair must be discarded and the patient must be convinced of rational, consistent treatment.
Treatment of ischemic spinal stroke
The main goal of treatment for ischemic stroke will be to improve blood supply to the spinal cord in the area affected by the stroke. In addition, it is very important to eliminate the factors that cause circulatory disorders and restore spinal functions lost during the course of the disease.
Blood circulation can be improved by increasing blood flow in nearby arteries. For this purpose, doctors usually prescribe vasodilators, which can improve blood flow through the vessels. In addition, decongestants are often prescribed, as well as those that have a venotonic effect. Mandatory in drug therapy will be the use of drugs that can increase the resistance of spinal tissue to oxygen starvation.
Usually, the root causes of circulatory disorders can be eliminated both conservatively and surgically. The choice of treatment will depend on the cause that contributed to the development of this disease.
If the lumen of a blood vessel is blocked by a thrombus, anticoagulants or antiplatelet agents are usually prescribed. If the cause of an ischemic stroke is a compressed artery due to an intervertebral hernia, then to restore normal blood circulation it is recommended to wear an orthopedic corset, perform therapeutic and preventive physical exercise and attend physiotherapy.
If conservative treatment is ineffective, then surgical treatment is performed. Surgical intervention is indicated in case of compression of blood vessels by a vertebral tumor.
At the stage of reverse development, it is still possible to restore lost spinal functions. To do this, they prescribe manual therapy, massage, exercise therapy, various physical procedures and send them to medical sanatoriums.
Forecast and preventive measures
The consequences of a spinal stroke are not as life-threatening as a cerebral stroke. An unfavorable prognosis occurs in extremely severe general somatic conditions, malignant tumors, and secondary infections.
Competent therapy triggers symptomatic regression, but with extensive damage, aggravated by other pathologies, and delayed therapy, recovery cannot be complete, the patient faces complete disability.
The basis of disease prevention is the timely detection, treatment and prevention of any vascular and vertebral pathologies. Giving up bad habits, physical activity, weight and nutrition control minimize the occurrence of predisposition factors to the disease.
If you notice any warning symptoms, call us at the numbers listed on the website. Our specialists will help make an accurate diagnosis and prevent the disease. At the Consulting and Diagnostic Center we use only modern diagnostic and treatment methods. Click the "SIGN UP" button and come see us.