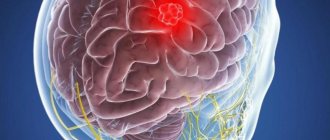
Cavernous hemangioma (cavernoma) is a benign vascular tumor. It consists of deformed venous vessels separated by cavities (cavities). As a rule, these are congenital neoplasms and much less often post-traumatic. They can be located in any area of the brain. They are more common in the hemispheres, but can also form in the trunk (a particularly problematic localization), and in one case out of ten they are multiple. The sizes of caverns range from a few millimeters to several centimeters. Despite their benign nature, hemangiomas, when located in the brain, often lead to serious consequences:
- they can compress and irritate brain structures, manifesting like any volumetric intracranial process with general cerebral and focal symptoms;
- Cavernomas are a source of intracerebral hemorrhages not associated with hypertension in two to four cases out of ten. Moreover, if the patient does not die after the first episode, the risk of a recurrent vascular accident reaches 30%, and a fatal outcome – 70%.
Small cavernous hemangiomas can exist for a long time without symptoms. Most often, the first symptoms appear in middle age. Clinical manifestations depend both on the size of the cavernoma and on its location. It can be:
- headache;
- dizziness;
- double vision;
- nausea;
- vomit;
- noise in the head;
- lack of coordination;
- seizures of a convulsive nature;
- paresis;
- sensitivity disorders;
- speech disorders;
- mental disorders.
Terminology
There are many synonyms for this pathology, including the terms cavernous hemangioma , cerebral cavernous malformation , or simply cavernoma . This pathology does not relate to neoplastic processes, therefore the terms hemangioma and cavernoma should be avoided. Additionally, it is important to note that according to the latest ISSVA nomenclature for classifying vascular anomalies, these changes correspond to low-velocity venous malformations. cavernous in the description or conclusion is useful, since this term is best known to most clinicians.
Symptoms of the disease
Symptoms of liver hemangioma do not appear immediately. Due to the small size of the formation, even in laboratory conditions it is not always possible to notice the presence of new cells. The same applies to clinical manifestations.
When the tumor grows to a size of 10 cm, features uncharacteristic of a healthy state can be detected:
- increase in liver volume;
- nausea, slight vomiting;
- unpleasant, painful sensations under the ribs on the right side.
All these symptoms arise as a result of the fact that the neoplasm puts pressure on neighboring organs and compresses nearby vessels.
In some cases, liver hemangioma may manifest itself after trauma to the abdomen (such as a strong blow) or intense physical exertion of the body. When it ruptures due to strain, it causes internal bleeding and acute pain in the abdominal area.
Are you experiencing symptoms of liver hemangioma?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Morophology
Macroscopically, cavernous venous malformation looks like a mulberry. On histological examination, cavernous venous malformations are thin-walled cavities of irregular shape, the walls of which are formed by endothelium. The cavities may be closely adjacent to each other, or be separated by collagen fibers or fibrous tissue, unlike AVMs, which may have medulla between the loops. In some cases, they are closely associated with developmental venous anomalies (DVA) and in this case it is a mixed vascular malformation.
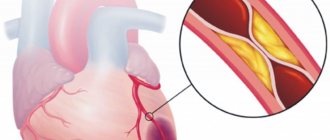
Cavernous angiomas on CT
When using visualization methods, it is useful to separate the cavity into 3 components. These include (1) a peripheral pseudocapsule, consisting of glial tissue impregnated with hemosiderin, (2) an irregularly structured intermediate connective tissue separating the cavities, and (3) a central vascular part, consisting of vascular cavities with slow blood flow.
On CT images without contrast enhancement, a cavernoma appears as a focal formation of an oval or nodular shape, characterized by slightly or moderately increased X-ray density and does not have a volumetric effect on the surrounding parenchyma. Areas of calcification and hemosiderin deposition in the walls of fibrous septa, along with stagnation of blood in the cavities, contribute to increased x-ray density on non-contrast-enhanced images. On CT images, calcifications are detected in approximately 33% of all cavernomas. If the formation is old, then it may contain central non-contrasting areas of reduced density, which corresponds to cysts from resorbed hematomas.
Contrast enhancement can be minimal or maximal, although 70-94% of cavernous malformations are weakly or moderately enhanced after intravenous contrast. In most cases, good contrast is the result of increased blood flow in the vascular component of the mass. The heterogeneous “speckled” enhancement is caused by intravascular fibrous septa, and the low-density rim along the periphery is caused by a pseudocapsule of glial tissue surrounding the formation.
Mass effect is not typical for cavernomas, unless they are associated with recent hemorrhage. On CT images without contrast enhancement, cavernomas may not be detected at all. In hemorrhages and the formation of intracerebral hematoma, cavernomas are visualized as areas of focal signal enhancement in the area adjacent to the hematoma.
Any hemorrhage detected on CT in a relatively young patient should be carefully investigated, and cavernous angioma should always be considered as a possible cause. When evaluating a patient with a seizure disorder, cavernous angioma should also be considered as a likely etiological factor, especially if the patient is between 20 and 40 years of age.
Cavernous malformations identified by CT may also include other rare vascular malformations (thrombosis of arteriovenous malformation, capillary telangiectasia), glioma (poorly differentiated astrocytoma or oligodendroglioma), and metastatic melanoma.
Diagnostics
Cavernous venous malformations of the brain are localized supratentorially in ~80% of cases, but in general can be localized in any part of the brain, including the brainstem. Most often they are single, but at the same time, in one third of patients with sporadic formation, more than one malformation may occur.
Computed tomography Large malformations are visualized by computed tomography as areas of increased density, in the presence of subacute hemorrhage, surrounded by perifocal edema, which do not enhance with contrast. Small malformations are difficult to distinguish.
Magnetic resonance imaging Magnetic resonance imaging is the method of choice. The classic sign is of popcorn or berries, surrounded on the periphery by a ring-shaped zone of signal loss due to the presence of hemosiderin and characterized by increased magnetic susceptibility.
- T1 and T2 MR signal is variable depending on the stage of breakdown of hemoglobin products in the malformation and fluid-liquid levels may sometimes be visualized.
- Gradient echo or T2* sequences are better at detecting malformations than T1 and T2 weighted images. In patients with a hereditary form of multiple cavernous malformations, they are important for counting the number of lesions that may be missed on spin echo sequences.
- Magnetic susceptibility-weighted images (SWI) have a sensitivity comparable to gradient sequences in detecting capillary telangiectasia, and they are also highly sensitive to detecting calcifications compared with T1- and T2-weighted images.
In the presence of recent hemorrhage, moderate perfiocal edema may be detected. Basically, the T1 MR signal intensity does not change after the administration of a contrast agent, but at the same time this is possible.
Selective angiography Kvernous malformations are not visualized during angiography, and arteriovenous shunts are not detected.
Hemangioma in children - symptoms and treatment
Currently, there are various ways to treat infantile hemangiomas. Many of them have already lost their significance, others are successfully used at the present time. The main vector of treatment is active observation or conducting one or another type of therapy from the moment of diagnosis.
When choosing treatment tactics, you should be guided by several factors:
- age of the child (the younger the patient, the higher the risk of further growth of the hemangioma);
- type of hemangioma and its location;
- presence of complications;
- parents’ desire to conduct this or that therapy;
- doctor's experience [24].
To help doctors decide on treatment tactics for infantile hemangioma, Russian surgeons D. A. Safin and D. V. Romanov proposed a special rating scale. With its help, you can assess the need for drug treatment with beta-blockers. This scale takes into account both the age of the child and the location of the hemangioma, as well as its size, quantity and thickness (presence of pathological volume) [28].
Rating scale for determining indications for systemic drug treatment of infantile hemangiomas with beta-blockers
| Criteria | Description | Points |
| Age | 0-4 months | 4 |
| 5-8 months | 3 | |
| 9-12 months | 2 | |
| 1 year and older | 1 | |
| Localization | Orbit, nose, lips, ears | 4 |
| Perineum, buttocks, genitals | 4 | |
| Hemangiomatosis | 4 | |
| Parenchymal organs and glands | 4 | |
| Scalp and other parts of the face | 3 | |
| Neck | 3 | |
| Joint area | 2 | |
| Hands and feet | 2 | |
| Torso | 1 | |
| Limbs | 1 | |
| Size (diameter) | More than 5 cm | 2 |
| 1-5 cm | 1 | |
| Up to 1 cm | 0 | |
| Pathological volume | Eat | 1 |
| No | 0 | |
| Quantity | 5 or more elements | 1 |
| 1-4 elements | 0 | |
| Complications | Eat | 1 |
| No | 0 |
The doctor examines the patient, evaluates the specified criteria and sums up the points. When the score is from 9 to 14, systemic drug treatment is indicated, and when the score is from 4 to 8, drug therapy is not required.
When assessing the location of a hemangioma, it is necessary to take into account not only the cosmetic defect, but also the risk of various complications. These “critical zones” include the ears, nose, lips and eyelids (orbits of the eye). For example, if the cartilage of the ear is destroyed, a permanent deformation of the auricle will occur, the correction of which will require plastic surgery. When infant hemangiomas are located in the perineum and buttocks, ulcerations often appear that are difficult to heal, so this localization is also critical.
The large size of the tumor indicates an active process of proliferation, which is accompanied by the risk of further growth of the hemangioma and a high probability of various complications.
In the treatment tactics of infantile hemangioma, it is also necessary to take into account the presence of a deep (subcutaneous) component of the tumor. It is not amenable to local treatment and laser treatment, which leads to tumor progression in the deep layers of the subcutaneous fat layer. Therefore, in this case, it is recommended to resort to drug therapy.
The greater the number of hemangiomas on the skin, the more difficult it is to carry out local therapy. The presence of more than five vascular tumors significantly increases the risk of hemangiomas in the internal organs (diffuse neonatal hemangiomatosis).
All methods of treating infantile hemangiomas can be divided into two categories:
- Conservative (non-invasive) treatment : oral medication, lotions, watchful waiting (time treatment) and laser treatment.
- Surgical (invasive) treatment : injections (sclerotherapy) or surgery (removal of hemangioma).
Conservative (non-invasive) treatment
Waiting tactics
This treatment was widely practiced before the advent of beta blockers. Now this method can also be used, but it is necessary to take into account: the younger the child, the higher the risk of tumor growth. Watchful waiting requires frequent and systematic follow-up examinations to determine the possible growth of hemangioma.
Drug treatment
Beta blockers. In 2008, French dermatologist C. Leaute-Labreze discovered the effect of propranolol on infant hemangiomas. From this period began the “golden age” of beta-blockers in the treatment of infantile hemangiomas. Given the low risk of side effects and the high effectiveness of treatment, they have become the “first line” of treatment for this disease.
The exact mechanism of action of beta-blockers is still unknown. Presumably, it includes vasoconstriction, suppression of VEGF-A (vascular endothelial growth factor), stimulation of apoptosis (the natural “disassembly” of pathological tissues). Studies have revealed the presence of β2-adrenergic receptors and VEGF-A in the capillaries of expanding infantile hemangioma, which decrease when β2-adrenergic receptors are suppressed.
Beta blockers can be used topically as a lotion or systemically by administering the medication orally. For local treatment, timolol-based eye drops or eye gel are used. For systemic therapy, the drugs Propranolol or Atenolol are used. Each of them has its own characteristics in dosage, frequency of administration and the risk of side effects.
Comparison of the pharmacological activity of the drugs Propranolol and Atenolol.
| Indicators of pharmacological activity | Propranolol | Atenolol |
| Bioavailability | 20-30 % | 40-60 % |
| Half-life of the drug | 3-5 hours | 6-9 hours |
| Lipophilicity (permeability through the cell membrane) | +++ | – |
| Removing the drug from the body | Liver 100% | Kidneys 90%, liver 10% |
Steroid hormones are one of the oldest methods of drug treatment for infantile hemangiomas. This method has been used from 1960 to the present and is a “second line” of therapy. Until 2008, it was the main method of treating hemangiomas, especially with active tumor growth.
The mechanism of the effect of glucocorticosteroids on infantile hemangioma is still not completely clear. However, it is known that steroid hormones influence adipogenesis, inhibit the formation of new vessels and reduce the production of proangiogenic proteins (VEGF-A, etc.).
Steroid hormones in tablets can be used as systemic drug treatment. Given the high risk of side effects of glucocorticosteroids and the emergence of beta-blockers, this method has become much less common. The main indications for its use are complicated hemangiomas and unresponsiveness of the formation to treatment with beta-blockers. The average course of treatment is from 4 to 12 weeks (maximum dose). Sometimes steroid hormone therapy can last up to 9-12 months of the child’s life.
It is also possible to inject glucocorticoids into the tumor. Typically, this treatment uses Triamcinolone injections or a mixture of Triamcinolone and Betamethasone. As a rule, such treatment is prescribed for small volumetric formations.
Cytostatics (Cytoxan, Vinblastine and Avastin), according to foreign authors, help stop the division of tumor cells in metaphase. However, this method has not found application in Russia, since Cytoxan acts on the growth of sensitive, rapidly proliferating cells, thereby inhibiting the erythrocyte lineage of the blood and the development of the egg. There is also an opinion that after using Cytoxan there is a risk of developing a secondary malignant tumor - angiosarcoma.
Vincristine is a cytostatic drug, an alkaloid from the pink periwinkle plant (Vincarosea). It causes apoptosis (the regulated process of cell death) of endothelial cells and reduces the production of their growth factors. As a rule, treatment with Vincristine is carried out for vascular pathology, which is not a true infantile hemangioma, but is associated with kaposiform hemendothelioma or tufted angioma with Kasabach-Merritt syndrome. The medication is given weekly through a central catheter.
This treatment method may be useful if steroid hormone therapy does not respond. Its appointment is carried out with the direct participation of oncologists. Side effects of the drug include skin irritation and rash, neurotoxicity, constipation, cranial nerve palsies, bone pain, alopecia, and muscle weakness. Typically, side effects are short-lived.
Interferons (Interferon-alpha-2a, Interferon-alpha-2b and Imiquimod - 5% Aldara ointment) stimulate the secretion of interferons, which suppress endothelial and fibroblast growth factors, and also promote tumor necrosis. They are used when steroid therapy is ineffective. The effect of these drugs is noticeable only after four months of use.
Since interferons cause a lot of complications (anemia, neutropenia, hypothyroidism, fever, neuroplegia), their use in the treatment of young children is not justified.
Laser correction
To treat vascular pathology, lasers with wavelengths of 532 and 585 nm, less often 1064 nm, are used. These lasers do not damage the skin, therefore they are considered conservative treatment.
The operation of lasers is based on the theory of selective photothermolysis, which was described in 1980. Laser radiation has a constant wavelength, but is absorbed differently by tissues. This is explained by the presence of chromophores (water, melanin and hemoglobin) in the skin. The result of this energy absorption is heating of the tissue. For example, wavelengths of 532 and 585 nm are best absorbed by oxyhemoglobin, due to which isolated heating of the vessel occurs, leading to damage to its endothelium without harm to surrounding tissues. As a result, the vessel closes.
After laser treatment, there are no scars or scars.
Surgical (invasive) treatment
Sclerosis of hemangioma
This method can be used for small surface formations. To glue tumor vessels together, a special drug is injected into them, which damages the endothelium of pathological capillaries and stimulates the formation of a blood clot. As a result, a fibrous subcutaneous scar is formed [4][5][7][16].
This method requires stages - carrying out a course of treatment at certain time intervals, for example, performing sclerotherapy once every 1-1.5 months. This is due to the rapid blood flow in the hemangioma, which reduces the time of exposure of the sclerosant to the endothelium, thereby reducing its effect.
The proposed sclerosants, for example, Aethoxysclerol and Fibro-vein, are intended for sclerosis of the veins of the lower extremities. A prerequisite for their use is the introduction of the drug into the bloodstream. They can cause disruption of microcirculation around the hemangioma up to tumor necrosis, which will lead to gross cicatricial changes. Alcohol should also not be used for sclerosis of vascular formations. Although it has a pronounced sclerosing effect, its use is often accompanied by side effects.
Cryodestruction (removal with liquid nitrogen)
The tumor focus can be destroyed using liquid nitrogen at a temperature of −195.6 °C. It is a colorless and odorless liquid that is sterile, non-toxic, inert to biological tissues and non-flammable. During cauterization of the hemangioma with liquid nitrogen, the tumor focus is clearly demarcated, which is replaced by an organotypic regenerate by 21-30 days after cryotherapy.
It is impossible to stop the growth and completely eliminate extensive and deep hemangiomas that have abundant blood circulation using cryodestruction. Usually it does not bring the desired result, as it leaves cosmetic defects, and in many cases leads to increased growth of hemangioma. Therefore, this method is best used in the treatment of local, non-extensive hemangiomas [5][8][21].
Surgical method of treatment
The radicality of surgical treatment of hemangiomas lies in the complete removal of all tissue affected by the tumor. Previously, it was believed that surgical removal of a tumor was dangerous due to complications: heavy bleeding during surgery and damage to the nerves, lymph nodes, and large arterial and venous trunks involved in the tumor. Now, with the advent of modern research methods, it has become possible to simultaneously remove a vascular tumor within healthy tissues, without affecting important anatomical structures [5][7][8].
Not all hemangiomas are subject to surgical removal: it should be used only in the presence of life-threatening conditions, for example, bleeding or when the airways are blocked, but most often it is resorted to at the final stage of involution, when there is almost no blood flow in the hemangioma - most often in 4- 5 years.
The scope of the operation is determined by the ability to perform it without irreversible cosmetic defects, the formation of a rough scar and the risk of dysfunction of nearby organs. In this regard, surgical treatment has its contraindications [5][7][8][21].
Outdated treatment methods
Radiation therapy (RBRT)
The essence of this method is to irradiate an area of skin with X-rays from a short distance. Such radiation is absorbed predominantly in superficial tissues and is effective only for infantile hemangiomas located exclusively on the surface of the skin.
As a result of X-ray therapy, “scars” form in the hemangioma, and telangiectasias (spider veins) form on the surface of the skin. As a result, to obtain a good cosmetic result in the future, either plastic surgery or laser treatment of the area of close-focus therapy is required [7][10].
Differential diagnosis
Kvernous venous malformations should be differentiated from numerous other pathologies leading to multiple microhemorrhages, including:
- cerebral amyloid angiopathy
- chronic hypertensive encephalopathy
- diffuse axonal injury
- cerebral vasculitis
- radiation damage to the brain
- hemorrhagic metastases
- Parry-Romberg syndrome
Large malformations can simulate:
- hemorrhage into metastases
- hemorrhage into a primary tumor (eg glioblastoma)
Meningioma: what is it?
As a rule, meningioma is benign in nature, however, like any other tumor localized inside the skull, benign meningioma of the brain is considered relatively malignant, accompanied by symptoms associated with compression of the brain matter. Malignant brain tumor (meningioma) is a less common disease characterized by aggressive growth and a high recurrence rate after surgical treatment.
Most often, brain meningioma is localized in the area of the foramen magnum, cerebral hemispheres, pyramid of the temporal bone, wings of the sphenoid bone, tentorial notch, parasagittal sinus and cerebellopontine angle.
In most cases, meningioma is located in a capsule. The tumor is not characterized by the formation of cysts; it can be small, just a few millimeters, or reach large sizes - over 15 centimeters in diameter. If a meningioma grows towards the brain, a node forms, which over time begins to compress the medulla. If a tumor grows towards the bones of the skull, over time it grows between the cells of the bone and causes thickening and deformation of the bone. The tumor can grow simultaneously towards the bone and brain, then nodes and deformation of the skull bones are formed.
Make an appointment
Brain angioma treatment in Germany: radiosurgery
Radiation as a treatment method is used if the tumor is located in hard-to-reach areas or when removing it there is a risk of affecting important areas of the brain. As a rule, the radiosurgical method is used for formations up to 1 centimeter.
A gamma knife is used for radiosurgical treatment. The required effect of treatment may occur in 4-5 months or several years.
The doctor must determine which treatment method is optimal. A qualified neurosurgeon will select a technique based on the situation and health status.
Kinds
There are 11 types of benign meningiomas:
- meningothelial meningiomas – 60%;
- transitional meningiomas – 25%;
- fibrous meningiomas – 12%;
- rare types of meningiomas – 3%.
A brain tumor can be located in different areas of the brain:
- convexital tumor – 40%;
- parasagittal – 30%;
- basal location of the tumor – 30%.
Meningioma of the brain of the frontal lobe
Meningioma of the frontal region forms very often, in most cases it does not bother the patient for a long time. If the meningioma is located in the right frontal lobe, symptoms will appear on the opposite side of the body.
The reasons for the development of meningioma of the frontal region are various: traumatic brain injury, inflammatory disease of the meninges, genetic predisposition, food high in nitrates, neurofibromatosis and other reasons. Radiation exposure is considered a proven cause of tumor development; all other causes are considered risk factors.
Meningioma of the frontal region can cause blurred vision, headache, paresis of the facial nerves, arm muscles, lethargy and other symptoms.
Anaplastic meningioma
Anaplastic meningioma is a grade 3 brain tumor; tumor recurrence occurs in all patients within three years after treatment.
Parasagittal meningioma
Parasagittal meningioma is located in the occipital, parietal or frontal part along the longitudinal midline. Often this tumor is accompanied by a pathological increase in the content of bone matter in the bone tissue. Parasagittal meningiomas, growing in the frontal part of the head, cause:
- increased intracranial pressure;
- development of congestive optic discs in the fundus;
- severe nausea and vomiting, headache;
- epileptic seizures.
Parasagittal meningioma of the parietal region of the head is characterized by sensory disturbances and epileptic seizures. Meningioma of the occipital region is characterized by increased intracranial pressure and hallucinations.
Atypical meningioma
Atypical brain meningioma is a grade 2 tumor; tumor recurrence occurs in 30% of patients within 10 years after treatment.
Meningioma falx
A tumor growing from the greater falciform process of the brain is called falx meningioma. Over time, the tumor grows into the sagittal venous sinus, resulting in impaired venous circulation and intracranial hypertension. The growth of the tumor causes the following negative symptoms: epileptic seizures, impaired sensitivity and motor activity of the legs, pelvic disorders.