Atherosclerosis. Episode I: The Hidden Menace of Plaques
“O pessimum periculum quod opertum latet. The most terrible danger is the hidden danger.” Publilius Syrus
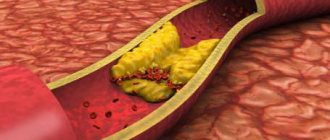
Atherosclerosis is a chronic vascular pathology that is the cause of most ischemic damage to the cardiovascular system. The term “atherosclerosis” was introduced in 1904 by Marchand and substantiated by the experimental studies of N. N. Anichkov, therefore it is also called Marchant-Anichkov disease. The “victims” are mainly arteries of the elastic and muscular-elastic type. The evolution of the pathological cascade includes the formation of endothelial dysfunction, massive deposition of lipids in the intima, exacerbation of innate and adaptive immune responses, proliferation of smooth myocytes of the vascular wall and remodeling of the extracellular matrix. These processes lead to the formation of atherosclerotic plaque (ASP), the morphological substrate of atherosclerosis (Fig. 1) [1]. .
Figure 1 | Scheme of etiopathogenesis of atherosclerosis
Exposure to cardiovascular disease risk factors (CVD risk factors) causes endothelial dysfunction and increases the permeability of the vascular wall, allowing the invasion of atherogenic lipid fractions (low density lipoproteins (LDL) and very low density lipoproteins (VLDL)). Endotheliopathy also promotes monocyte recruitment, migration, and adhesion. Once in the intima, monocytes differentiate into macrophages and absorb modified lipids, turning into foam cells. Simultaneously, in this first stage of the disease, smooth muscle cells (SMCs) migrate into the intima, where they synthesize elements of the extracellular matrix (ECM) and contribute to the formation of the fibrous capsule. As atherosclerotic plaque (ASP) grows, the number of SMCs decreases and the foam cells undergo apoptosis, releasing active metalloproteinases that destroy the fibrous membrane, increasing the susceptibility of the plaque to rupture. There is a change from a stable ASB subtype to an unstable one. The immune system (innate and acquired immunity) is actively involved in this process and plays a key role in plaque vulnerability [1].
It contains a lipid, or, to be more precise, atheromatous (Greek athḗra, “gruel”) core, built from modified lipids, proteins, their breakdown products, cholesterol crystals, fragments of macrophages and smooth muscle cells with connective tissue growing around it ( sklḗrōsis, “hardening”) - fibrous cap [2].
During the atherosclerotic process, stages are revealed, with characteristic pathomorphological manifestations (Table 1) [2].
Table 1 | Pathomorphological classification of atherosclerotic lesions. Comparison of macro- and microscopic stages of the process [2]
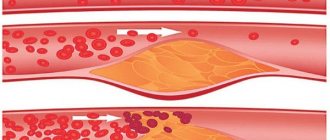
The morphological features of the plaque determine the degree of its “danger” to the body. Violation of the integrity of the ASP leads to thrombogenic damage. In order to predict and determine the correct treatment strategy, formed ASPs are divided into stable and unstable (Fig. 2, 3). The main characteristics for classification are the structure of the fibrous cap and the size of the lipid core [3]. .
Figure 2 | Sections of a coronary artery with damaged, unstable and stable atherosclerotic plaques
Left: rupture of the fibrous cap of the plaque (red arrow) with superimposition of atheromatous masses and thrombus formation (Tp). In the center: atherosclerotic plaque (ASP) with a thin fibrous cap - an unstable subtype. Inside the plaque there is a large atheromatous core (AN) with hemorrhages (hemorrhages). White arrows indicate the thinnest part of the fibrous cap. Right: stable ASP, the tegmentum is mainly composed of fibrous tissue with partial calcification (black arrows) [3].
Figure 3 | Microphotographs of the lumen of a coronary artery with varying degrees of stenosis severity
A-C: atherosclerotic plaque (ASP) with cap rupture in mild, moderate and severe stenosis, respectively (the severity of stenosis was calculated by the diameter of the lumen (luminal stenosis)). A: non-occlusive thrombus. B and C: occlusive thrombus. D–F: unstable ASP with mild, moderate and severe stenosis, respectively. The atheromatous core (AN) is covered with a thin fibrous cap; blood clots are not detected in the lumen. GI: stable ASP with mild, moderate and severe stenosis, respectively. The AG is absent or small in size, and calcification (Ca++) is often observed [3].
Stable plaques have a well-defined dense fibrous cap without thinning throughout, as well as a small atheromatous core. Some plaques, instead of an atheromatous core, have deposits of calcium salts (petrificates) at their base. The thickened fibrous cover of the plaque indicates a good reparative function of the intimal smooth muscle elements. The cover of stable plaques is mainly represented by dense connective tissue with compactly located collagen fibers, with a meager amount of lipids and cellular elements [4].
Activated macrophages located in the ASP secrete destructive metalloproteinases that break down the collagen and elastin of the fibrous cap of the plaque. The predominance of this function aggravates the destructive processes in the plaque core. This is how a vulnerable unstable plaque (vulnerable unstable plaque) is formed (Fig. 4) [5]. In such a plaque there is a high probability of the formation of a thrombogenic site. Criteria for an unstable vulnerable plaque: the presence of a thin fibrous cap (less than 65 µm) with pronounced infiltration by inflammatory cells (T-lymphocytes and macrophages), a large lipid core occupying more than 30% of the total area of the plaque, massive neovascularization, with the occurrence of hemorrhages from pathologically formed neovessels, abundant infiltration of foam cells. It has also been suggested that the presence of multiple areas of microcalcification (as opposed to large homogeneous foci of calcification) in the fibrous cap may increase the risk of rupture. .
Figure 4 | "Virtual histology" - data from optical coherence tomography
A: Thin capsular fibroatheroma (yellow arrows) is an atherosclerotic plaque with a fibrous cap <65 µm overlying a prominent lipid core. B: Damaged plaque - with rupture of the fibrous cap (red arrows) and formation of a cavity (red asterisk) within the plaque. C: Microchannels (white arrows). D: Clusters of macrophages appear as bright spots with high signal dispersion (yellow arrows). E: Cholesterol crystals are thin linear areas of high signal intensity within the plaque (red arrows). F: Thrombus is an unformed mass protruding into the lumen of the vessel, size ≥ 250 µm (white arrows) [5].
Vulnerable unstable plaques vary in their “weak link.” There are fibroatheroma with a thin fibrous cap (lipid type), plaques with a high proteoglycan content and a pronounced inflammatory reaction, which leads to erosion and thrombosis (inflammatory-erosive type) and plaques with necrosis/calcinosis (dystrophic-necrotic type) [6].
Timely visual examination of the structure of ASP allows us to move away from the concept of “symptomatic” and “asymptomatic” plaques, forming an idea of the potential of a particular plaque before the development of a critical situation. It is most important to find out the state of the fibrous cap and the level of activity of necrotic processes in the core of the plaque. Predictors of the highest risk of ischemic complications are the presence of hemorrhages, ulcerations and thinning of the ASP cap, blood clots and other embologenic material (sometimes these can be fragments of calcifications) on the lumenal (facing the lumen of the vessel) surface of the plaque.
Sources:
- Badimon L., Vilahur G. Thrombosis formation on atherosclerotic lesions and plaque rupture. J Intern Med. 2014;276(6):618-32.
- Simionescu M., Sima AV Morphology of Atherosclerotic Lesions. In: Wick G, Grundtman C (eds) Inflammation and Atherosclerosis. Springer, Vienna.2012:19-37.
- Tian J. Distinct morphological features of ruptured culprit plaque for acute coronary events compared to those with silent rupture and thin-cap fibroatheroma: a combined optical coherence tomography and intravascular ultrasound study. J Am Coll Cardiol. 2014;63(21):2209-16.
- Rognoni A. et al. Pathophysiology of Atherosclerotic Plaque Development. Cardiovasc Hematol Agents Med Chem. 2015;13(1):10-3.
- Narula J. et al. Histopathologic characteristics of atherosclerotic coronary disease and implications of the findings for the invasive and noninvasive detection of vulnerable plaques. J Am Coll Cardiol. 2013;61(10):1041–1051.
- Lee KY, Chang K. Understanding Vulnerable Plaques: Current Status and Future Directions. Korean Circ J 2019;49(12):1115-1122.
Removal of cholesterol plaques in the carotid artery
Removal of cholesterol plaques on the carotid artery at the second stage (fibrosis) and at the third stage (calcionosis) can occur in several ways:
- increasing blood (arterial) pressure - but this path is fraught with the formation of new damage to blood vessels and, as a consequence, the formation of new atherosclerotic deposits;
- dilatation of blood vessels, however, this method is ineffective on the carotid artery and is used more often for varicose veins of the extremities;
- increased tone of blood vessels;
- cleansing the blood of cholesterol - however, this method does not so much destroy existing plaques as prevent the formation of new ones.
The cost of removing cholesterol plaques on the carotid artery using medications is entirely determined by the cost of the drugs used. The cost of surgical treatment (carotid endarterectomy, angioplasty, stenting) is even higher if it is not done according to the insurance policy. Surgical treatment is resorted to when conservative methods fail.
Conservative methods of removing cholesterol plaques include taking specialized medications, increasing the proportion of foods in the diet that cleanse blood vessels of cholesterol, performing (daily) therapeutic exercises for atherosclerosis, and taking statins or other medications for high cholesterol.
How to remove cholesterol plaques from the carotid artery safely? Surgery has some risks, and drug treatment has contraindications and side effects. Drug treatment can be aimed at reducing the level of cholesterol synthesis by the liver, increasing energy metabolism in cells - this is how it is possible to remove excess cholesterol from the blood and carotid arteries. An alternative is infusions and herbs for cholesterol plaques, but their effectiveness remains unproven.
Surgery to remove cholesterol plaques in the neck
Surgical intervention (operation) to remove cholesterol plaques in the vessels of the neck is prescribed when drug treatment methods have not brought (or cannot bring) any effect, or if the underlying disease has led to complications. Surgery to remove cholesterol plaques in the neck does not lead to a complete recovery, because... It is not the cause of the disease that is eliminated, but its consequence.
Surgery to remove cholesterol plaques on the carotid artery is called a carotid artery bypass. The purpose of the procedure, as well as the determination of possible risks to the health and life of the patient, is carried out by a surgeon, cardiac surgeon and vascular surgeon. As a result of the operation, the patency of blood vessels is restored, i.e. revascularization is performed.
An alternative to surgery to remove cholesterol plaque in the carotid artery is stenting a blood vessel - this is a low-traumatic procedure in which a stent is installed in the artery, expanding the lumen of the vessel, and special membrane filters. The membranes filter blood from microthrombi, but do not interfere with blood circulation in the brain.