Carotid endarterectomy is surgery to remove plaque in the carotid artery and is used to reduce the risk of stroke. Treatment of atherosclerotic plaque on the walls of the vessels of the carotid arteries is impossible with the help of medications, since it is a dense rocky formation and is not able to dissolve.
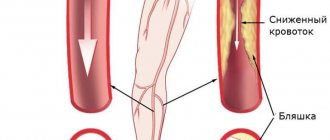
With atherosclerosis, plaques in the carotid arteries grow at the bifurcation (carotid bifurcation), where the common carotid is divided into the internal and external carotid. The plaque can gradually narrow the lumen of the vessel, a condition called stenosis.
Plaque rupture can lead to the formation of a blood clot in the vessel. Part of the resulting blood clot can break off and move through the lumen into the brain, where it blocks blood circulation and leads to the death of brain tissue - ischemic stroke.
Sometimes carotid bifurcation stenosis causes temporary symptoms of cerebrovascular accidents, which are called transient ischemic attack. TIAs are a sign of a high risk of developing a full-blown ischemic stroke and require the active attention of a vascular surgeon.
Even if the atherosclerotic plaque does not cause symptoms, a patient with stenosis is at high risk of developing an ischemic stroke. Based on the results of the studies, it was decided that a narrowing of the carotid bifurcation by 70% or more is a condition threatening the development of a stroke and requires endarterectomy or stenting.
Anesthesia during surgery
In the preoperative room, the patient is fitted with a urinary catheter, an intravenous catheter, and a monitor is connected to monitor the ECG during the operation.
In our clinic, for carotid endarterectomy, local anesthesia with a weak solution of lidocaine is most often used, but with the mandatory supervision of an anesthesiologist. Local anesthesia has enormous advantages over anesthesia in terms of preventing cerebral complications. Local anesthesia provides good pain relief throughout the operation.
A conscious patient is the best neurological monitor. To ensure the safety of carotid endarterectomy, it is necessary to understand how the brain responds to temporary compression of the carotid artery. For this we use local anesthesia. After identifying the carotid bifurcation, we temporarily clamp it, but maintain contact with the patient and give him a number of tasks. If the patient understands and performs the tasks well, then we perform the operation without using a temporary shunt. If we notice that the patient begins to “float away,” we use a special tube to perform the operation under a temporary shunt. Blood flows through this tube during clamping.
Contraindications for surgery
Despite the benefits of surgical interventions, in some cases they cannot be performed. Like other operations, carotid endarterectomy also has contraindications. Reviews from patients suffering from atherosclerosis make it clear that many different examinations are performed before surgery. Only after the doctor is convinced that there are no contraindications, the patient begins to be prepared for surgery. Carotid endarterectomy is prohibited in the following cases:
- Uncontrolled by medications (decompensated) hypertension.
- Extensive acute cerebrovascular accident.
- Unstable angina or recent myocardial infarction.
- Acute heart failure.
- Recently suffered a stroke.
- Chronic circulatory failure of 2 and 3 degrees.
- Alzheimer's disease.
- Severe oncological diseases.
How is the operation performed?
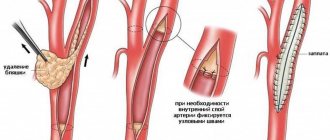
After anesthesia, a 5-10 cm long incision is made along the inner edge of the sternocleidomastoid muscle. The internal, common and external carotid arteries are isolated from the surrounding tissues and rise onto the supports.
During the operation, we perform a test with temporary clamping of the lumen for 3 minutes. The patient is asked to count to 100, shake hands, and move a leg. If there are no signs of circulatory failure in the brain, then we open the vessel and perform an endarterectomy. Otherwise, a special temporary shunt is installed in the lumen.
After arteriotomy, endarterectomy is performed - removal of the atherosclerotic plaque. The removal method may vary. With a longitudinal section, the atherosclerotic plaque peels off from the outer wall of the vessel. With the eversion technique, the internal carotid artery is divided transversely, after which it is everted, and the hard plaque moves away from the wall and comes off. After removal of the atherosclerotic plaque, the vessels are sutured. After a longitudinal dissection, to expand the lumen of the vessel, it is necessary to sew a special patch into the incision, but with the eversion endarterectomy technique, a patch is not required.
After starting the reconstructed artery, ultrasound monitoring of blood flow is mandatory. After this, the wound on the neck is closed with stitches after eliminating all possible bleeding. The skin is closed with an absorbable suture that will not need to be removed. Additionally, to control bleeding, a drainage tube with a bulb is installed, which is removed the next day.
Causes of plaques in the carotid arteries
The formation of cholesterol plaques in the carotid arteries is one of the forms of systemic atherosclerosis, rarely occurring in isolation.
As a rule, atherosclerosis of the brachiocephalic arteries (brachio - shoulder, cephalis - head (Greek)), which includes the carotid arteries, is combined with atherosclerosis of the aorta, coronary arteries, and arteries of the lower extremities. Atherosclerosis
- a chronic disease of arteries of the elastic and muscular-elastic type, arising as a result of lipid metabolism disorders and accompanied by the deposition of cholesterol and some fractions of lipoproteins in the intima of blood vessels. Deposits form in the form of atheromatous plaques. The subsequent proliferation of connective tissue in them (sclerosis), and calcification of the vessel wall lead to deformation and narrowing of the lumen up to obliteration (blockage). It is impossible to name one single reason leading to atherosclerotic restructuring of the artery wall and the formation of atherosclerotic plaques.
Most researchers agree with the fact that atherosclerosis is based on a violation of fat metabolism (more precisely, cholesterol esters) at the level of genetic predisposition. Familial hypercholesterolemia (FH) is a known disease. This is a disease caused by a decrease in the rate of removal of low-density lipoprotein (LDL) from the bloodstream due to mutations in the specific LDL receptor gene. Familial hypercholesterolemia is the most common genetic disease due to a single gene mutation (monogenic disease). The modern medical scientific community, based on numerous studies, considers risk factors to be the main triggers for the progression of atherosclerosis (an increase in the size and number of plaques).
Possible complications
Eversion carotid endarterectomy in our clinic is a safe intervention. We noted serious complications in the postoperative period only in 0.5% of patients. The following complications sometimes occur after surgery:
- Stroke during or after surgery develops for various reasons. Most often, this may be thrombosis of the reconstructed artery or embolism (transfer of a piece of plaque) to the cerebral vessels. The patient should be closely monitored in the early postoperative period to notice neurological problems as early as possible and take action. The incidence of these complications in our clinic was 0.5%.
- Bleeding from the surgical area is potentially life-threatening, as the hematoma can compress the trachea and cause suffocation. Installing drainage allows you to suspect this complication in time and take action.
- Damage to the hypoglossal or recurrent nerve is a consequence of inaccurate technique during surgery. This complication is manifested by loss of voice or deviation of the tongue and difficulty eating and speaking. We have not encountered this in our practice.
Carotid endarterectomy – follow-up therapy and risks
21.10.2019
Aspirin therapy should be initiated at the time of diagnosis of transient ischemic attack (TIA) or stroke. Recent studies of aspirin and carotid endarterectomy suggest that low dose (80–325 mg per day) aspirin is optimal for preventing thromboembolic events after carotid endarterectomy . After a carotid endarterectomy, blood should be checked (complete blood and electrolytes). Cardiac function can be monitored using ECG recordings. Frequent neurological evaluation is necessary, as well as hemodynamic monitoring (to maintain blood pressure within its previous range). Antiplatelet therapy is necessary. Approximately two weeks postoperatively, patients are assessed for neurological and wound complications. Carotid ultrasound examinations are performed six months after surgery and are scheduled annually.
Risks
There are several important complications that can occur after carotid endarterectomy . A stroke or short-term neurological deficit may occur within 12-24 hours after surgery . These conditions are usually caused by thromboembolic complications, which usually originate from the endarterectomy site or damaged vessels that were involved during the operative procedure (internal, common and external carotid arteries ). Hypertension may occur in approximately 33-50% of patients . Complications such as hematoma formation can cause pain and deviation of the trachea, which can interfere with normal breathing. During surgery , damage to vital nerves , such as the cervical nerves that give sensation to the neck, . Patients may complain of numbness in the ear , lower neck , and upper face . Damage to the hypoglobular nerve (which supplies the tongue) can cause the tongue to deviate from the paralyzed side and impair speech . Additionally, the problem may recur, leading to stenosis and symptoms. The normal progression of outcomes after carotid endarterectomy is stroke prevention, which is approximately 1.6% (two-year stroke risk) compared with 12.2% for patients who are medically treated .
The study results show that the stroke rate for the post-surgical group (those who received carotid endarterectomy ) was 5.1%; for the medically treated group , the incidence was 11%. As with all surgical procedures, it is important for patients to choose a surgeon who is experienced in the specific procedure and in managing the condition.
It is important to know
Approximately 30% of stroke survivors die within the first 12 months. Within 12 years, approximately 66% will eventually die from a stroke, making this condition the third leading cause of death. The cause of atherosclerosis is unknown, but damage to the arteries can occur from infectious agents, hyperlipidemia, cigarette smoking, and hypertension . Among those who have experienced one stroke, the incidence of stroke within five years is 40-50%. Research conducted in 2002 concludes that carotid endarterectomy remains the standard of care for carotid atherosclerosis .
Published in Cardiology Premium Clinic
Prognosis in the postoperative period
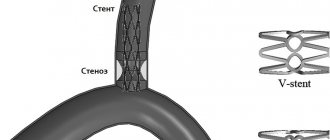
After successful surgery, the risk of stroke is reduced by 5-7 times. The patency of the carotid artery remains satisfactory in most patients for many years. To prevent thrombotic complications, blood thinning drugs (Plavix, aspirin), drugs to lower blood cholesterol levels, and changes in diet and lifestyle are prescribed. However, some patients may develop repeated narrowing in the endarterectomy area - restenosis. For timely diagnosis of restenosis, we examine our patients with ultrasound every year, and if restenosis is detected, we prescribe MSCT of the vessels of the neck and head. Detection of restenosis of the internal carotid artery forces the surgeon to suggest re-intervention. Most often, to correct such pathology, we use endovascular intervention without incisions - balloon angioplasty and stenting. The effect of such treatment lasts for a long time.
Description of the procedure
Carotid endarterectomy is a surgical intervention that involves clearing the inner layer of a vessel from atherosclerotic plaque. It is performed in cases where drug treatment is powerless or the risk of developing stroke is too high. Medicines are not able to have the desired effect when the atherosclerotic plaque occupies more than half the diameter of the carotid artery. Or if cholesterol closes the lumen of the vessel from several sides at the same time. In addition, the risk of stroke increases significantly in the presence of uncontrolled hypertension. In this case, the atherosclerotic plaque can break away from the endothelium at any time, regardless of its size. The result may be a blockage not of the carotid artery itself, but of its branches that supply the brain. As a result, an ischemic stroke develops.
Risk factors
Risk factors include manifestations of atherosclerosis, which add stress to the arteries and increase the risk of damage, and also contribute to the development of atherosclerotic plaques. These factors include a family history of atherosclerosis and coronary heart disease (CHD), high blood pressure (hypertension), obesity accompanied by a sedentary lifestyle, diabetes mellitus, abnormal blood lipid levels, smoking, lack of physical activity and older age.