Atherosclerosis of the carotid arteries as a cause of stroke
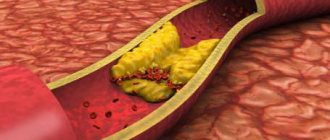
Atherosclerosis is a lesion of the arteries, in which dense growths (atherosclerotic plaques) appear on the inner wall, which narrow the lumen of the artery and impair blood flow through it.
The disease usually develops after 40 years of age, especially in patients with high blood cholesterol levels, as well as in smokers. The carotid arteries are no exception. With the development of atherosclerosis, plaques also appear in them, the lumen of the vessel narrows (this is called stenosis), and with stenosis of more than 60%, there is a high risk of developing such a formidable complication as a stroke. With atherosclerosis of the carotid arteries and increased blood pressure, plaques can break off from the vessel wall and enter the cerebral vessels with the blood flow. When large vessels are blocked, the blood supply to a certain area of the brain is cut off and an ischemic stroke develops. When small vessels are blocked, a microstroke occurs (also called a transient ischemic attack).
For small, less than 50% of the lumen of the vessel, stenoses, it is possible to carry out conservative therapy aimed at lowering cholesterol levels in the blood, improving cerebral circulation, and improving metabolic processes in brain tissue. With more significant stenoses, and especially in the presence of neurological symptoms, conservative therapy is not enough, and to avoid stroke, surgical treatment is required - carotid endarterectomy or endovascular interventions.
WELCOME!
GBUZ JSC "AOKB" provides planned, urgent, emergency specialized and consultative and diagnostic medical care to patients in the city of Arkhangelsk and the Arkhangelsk region in the following areas:
| Chief physician Petchin Igor Vasilievich |
cardiology, neurology, gastroenterology, pulmonology, rheumatology, allergology, hematology, nephrology, endocrinology, neurosurgery, surgery (including purulent surgery), urology, traumatology, orthopedics, combustiology (burn medicine), otorhinolaryngology, maxillofacial surgery, vascular surgery , cardiac surgery, thoracic surgery, infectious diseases, obstetrics and gynecology, neonatal pathology, intensive care (including neonatal intensive care).
The institution's 24-hour hospital has 877 beds. Intensive care unit with 40 beds. 10 beds have been deployed in the Solovetsky District Hospital branch. Every year, more than 20 thousand patients are treated in the 24-hour hospital.
Up to 500 patients per shift and more than 100 thousand people annually seek advice from specialist doctors at the clinic. There is a day hospital. The structure of the hospital includes specialized centers for patients, as well as schools and offices in which regular meetings of patients are held with the participation of their relatives, friends and medical specialists.
In total, the institution employs almost 2 thousand medical and general hospital personnel.
For a long time, the State Budgetary Healthcare Institution JSC "AOKB" has been participating in a joint Russian-Norwegian project to reduce road traffic injuries in the Arkhangelsk region.
The hospital operates under the federal program “M8 Highway” as a first-level trauma center. All people injured as a result of road accidents on the Kholmogory highway are taken to the State Budgetary Healthcare Institution JSC "AOKB". This work involves ambulances equipped with the GLONASS system - a system for determining the location of a vehicle involved in an accident.
To help the population of the Arkhangelsk region and the city of Arkhangelsk, an emergency consultative emergency medical care department (ECMC) was created on the basis of the State Budgetary Healthcare Institution JSC "AOKB" in order to improve medical care for adults and, in some cases, children with emergency conditions.
In 2014, a new surgical building was put into operation, which greatly improved the living conditions of patients and the working conditions of doctors in surgical departments.
Read more…
Examination before carotid endarterectomy
Before hospitalization, the patient must have the following results of laboratory and instrumental examinations with him:
- Clinical blood test
- General urine analysis
- Blood biochemistry (AST, ALT, total bilirubin, direct bilirubin, urea, creatinine, total protein)
- Blood test for hepatitis B, C, HIV, syphilis.
- Chest X-ray or fluorography
- ECG
- Already in the hospital, before the operation, the patient undergoes:
- Duplex ultrasound angioscanning
- Computed tomography of the brain
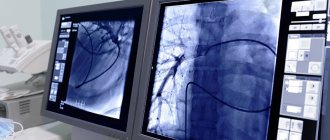
- Angiography
These examinations help to find out how narrowed the lumen of the vessel is, the size and location of atherosclerotic plaques, the speed characteristics of blood flow through the carotid arteries, and the characteristics of cerebral blood flow.
After operation
In the postoperative period, the patient is prescribed antiplatelet therapy - drugs that “thin” the blood. These drugs should be taken only as prescribed by a doctor with strict adherence to the dosage and regimen. Self-cancellation or replacement with other drugs without a doctor’s prescription is unacceptable.
Otherwise, the postoperative period after surgery on the carotid arteries does not differ significantly from any other operations: limiting physical activity, wound care.
In the vast majority of cases, the operation is quite comfortable and well tolerated by patients.
A timely operation saved the lives of many thousands of patients. Remember, there is nothing more expensive than your life and health.
Technique for carotid endarterectomy
At its core, the operation is the removal of atherosclerotic plaque from the carotid artery.
The operation in Moscow is performed under local anesthesia, but anesthesia is also possible. Local anesthesia is preferable, with fewer complications and faster recovery.
During the operation, a small incision is made in the artery with “scraping” of its inner wall along with atherosclerotic plaques. A suture is placed on the wall of the vessel, blood flow is restored. In some cases, replacement of the damaged vessel wall is required, which is performed from a fragment of a vein taken from the patient.
Some aspects of the operation are shown in the photo below:
A comment
The article presents a clinical case dedicated to the surgical treatment of a patient with widespread atherosclerotic lesions of the brachycephalic arteries, manifested by the clinical manifestations of cerebrovascular insufficiency in both the carotid and vertebrobasilar areas. In this situation, the authors made a successful attempt at radical surgical intervention on the carotid and vertebral arteries, which made it possible to restore adequate blood flow in the compromised areas.
The presented publication will be of interest to a wide range of specialists – vascular neurosurgeons and vascular surgeons.
V.N. Dan (Moscow)
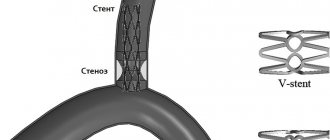
Endovascular interventions on the carotid arteries
Such manipulations include balloon angioplasty and stenting. With balloon angioplasty, the lumen of the vessel is expanded from the inside using a special catheter inserted through the subclavian artery. When stenting, a special metal stent is placed in the lumen of the vessel in the area of stenosis, which expands the lumen of the vessel and prevents it from narrowing.
These interventions are used in patients with severe concomitant pathology who cannot undergo standard carotid endarterectomy. This is due to the fact that with balloon angioplasty there is a high risk of vessel rupture, and with stenting the service life of the stent is usually no more than 5 years, after which a more complex operation is required.
Preparing for a non-surgical procedure
Before elective stenting, your endovascular surgeon will review your medical history and perform a physical examination. Can be assigned:
- Ultrasound . To obtain images using sound waves of the narrowed artery and the speed of blood flow to the brain.
- Contrast-enhanced computed tomography (MSCT) or Magnetic resonance angiography (MRA) . This diagnostic produces highly detailed images of blood vessels using radiofrequency waves in a magnetic field or X-rays injected with a radiopaque contrast agent.
Food and medicine
You will receive instructions about what you can eat or drink before your angioplasty and ICA stenting. Preparation may be different if you are already in the hospital before the intervention.
The night before your endovascular surgery:
- Follow your doctor's instructions about adjustments to your current medications. Your doctor may tell you to stop taking certain medications before having angioplasty, especially if you take certain diabetes medications or blood thinners.
- Arrange transportation home in advance. Angioplasty usually requires a hospital stay, and you may not be able to go home the next day due to the lingering effects of the sedation.
Rehabilitation period
Recovery after stenting takes minimal time. The patient will stay in the clinic for 6-24 hours, depending on the current condition. This is necessary so that the doctor can monitor the occurrence of complications. You should drink plenty of fluids for 2-3 days after surgery to flush the contrast agent out of your body. It is also necessary to limit physical activity, follow a diet, and give up bad habits. A healthy lifestyle will help prevent the development of complications and restenosis.
Still have questions about carotid artery stenting?
Free consultation with AngioClinic specialists
Author
Salmina Daria Vladimirovna
Geneticist. Graduated from the Chelyabinsk State Medical Academy. She completed an internship at the Northwestern State Medical University named after I.I. Mechnikov.
The cause of age-related changes in the vessels of the neck
Throughout life, the human body is affected by many negative factors. The environment, lifestyle, and foods consumed play an important role. With excessive consumption of foods high in cholesterol, atherosclerotic plaques form. As you age, they grow, causing partial blockage of the arteries, a condition called stenosis.
Another reason for age-related changes in the vessels of the neck is a decrease in the synthesis of collagen and elastin by the body. Vascular tissues become less elastic and more susceptible to negative influences.
Risk factors for complications of carotid stenting
These factors include:
- High blood pressure;
- Allergy to X-ray contrast agents;
- Calcification (impregnation with lime) and large-scale narrowing of the carotid arteries;
- Sharp bends and other anatomical features leading to difficulties in stent placement;
- Plaques of significant size, or atherosclerosis of the aorta in the area of the beginning of the carotid arteries;
- Age over 80 years;
- Concomitant blockages of the arteries of the vessels of the arms and legs.
Carotid-subclavian shunt
The patient is placed on his back with a bolster under the neck and shoulders, with the arm adducted on the side of the surgical intervention. The patient's head should be turned in the opposite direction. A skin incision 5–6 cm long is made along the upper edge of the clavicle, 1 cm away from it. The incision begins 1 cm outward from the jugular fossa and continues above the lateral (clavicular) part of the sternocleidomastoid muscle. The platysma is dissected, the external jugular vein is ligated and transected. A dissector is placed under the clavicular portion of the sternocleidomastoid muscle and, at a distance of 1 cm from the clavicle, the muscle is crossed with an electric knife. In the medial part of the wound the internal jugular vein is found. The prescalene fatty tissue is pulled upward with a tuffer, exposing the anterior scalene muscle with the phrenic nerve located on its anterior surface. The nerve is mobilized, held on a holder and retracted medially upward. The anterior scalene muscle is mobilized laterally and posteriorly with a small tuff. Manipulations are carried out especially carefully behind the muscle, remembering the neurovascular bundle passing there. After placing the dissector under the muscle, it is crossed with an electric knife closer to the first rib. The left subclavian artery lies deeper than the right. Medial to the left subclavian artery are the esophagus and trachea with the recurrent nerve, and between the subclavian and common carotid arteries, bending around the subclavian artery from behind and above, the thoracic lymphatic duct runs. The vertebral artery arises from the posteromedial semicircle of the subclavian artery. In front, in this place, the subclavian artery is crossed by the vagus nerve, and laterally, next to the anterior scalene muscle, the phrenic nerve passes. The right subclavian artery in the first segment passes next to and slightly behind the right common carotid artery. There is no lymphatic duct here. Lateral to the carotid artery, the subclavian artery is crossed in front by the vagus nerve, the giving off recurrent nerve, which immediately goes behind the subclavian artery, bending around it. Anterior to the subclavian artery, the phrenic nerve passes between the thyrocervical trunk and the anterior scalene muscle. Knowledge of the topography of these nerves must be absolute to avoid postoperative complications. Below the muscle is the subclavian artery, which needs to be mobilized. At the jugular vein, the vertebral artery departs from the superoposterior part of the subclavian artery, which must be preserved. The next major branch, the thyrocervical trunk, can be ligated and divided to ensure better mobility of the subclavian artery. The internal mammary artery, which arises from the inferior part of the subclavian artery, is best preserved for possible future mammary coronary bypass surgery. The veins of the same name, flowing into the underlying subclavian vein (Pirogov’s angle), are also ligated and crossed, if necessary. When approaching from the left, it is necessary to remember that at the confluence of the subclavian and internal jugular veins, the easily wounded thoracic lymphatic duct opens, coming from the mediastinum. The common carotid and subclavian arteries are distinguished proximal to the vertebral artery. The 2nd segment of the subclavian artery is prepared, the artery is isolated from the surrounding tissues, taken on a holder, and the CCA is also taken on a holder. It is considered advisable to measure retrograde pressure in the CCA and maintain it at all stages of the operation at least 60 mmHg. Art. An end-to-side anastomosis is performed on the clamped arteries using a vascular synthetic prosthesis, or an end-to-side anastomosis between the transected subclavian artery and the common carotid artery is performed. A prerequisite is the prevention of air embolism before removing vascular clamps.