Chronic occlusions of the coronary arteries
Chronic occlusions make up a significant portion of coronary artery lesions detected in patients during diagnostic coronary angiography. In the case of multivessel disease, the patient may be offered either coronary artery bypass surgery or an endovascular coronary artery stenting procedure.
If multi-vessel lesions of the coronary arteries are detected, it is possible to perform a one-stage endovascular procedure for myocardial revascularization on several coronary vessels or to perform a staged endovascular procedure. Recanalization of chronic occlusions, in turn, requires special training of the radiosurgeon and sufficient experience in performing such operations.
An example of successful treatment of a patient with multivessel disease and chronic coronary occlusions
Patient A., 44 years old, was admitted to the Clinic of Innovative Surgery in September 2015. For a long time, the young man was bothered by chest pain and shortness of breath with little physical activity, and a sharp impairment in his ability to work. After a detailed examination, a diagnosis was made - coronary heart disease, functional class 3. Coronary angiography was recommended and performed.
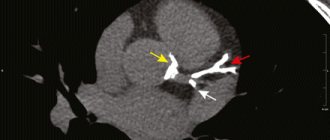
Coronary angiography revealed multi-vessel multi-level occlusive-stenotic lesion of the coronary bed:
- LKA barrel: normally positioned, not changed,
- RCA: in the proximal segment there is extensive chronic occlusion, the post-occlusion section is satisfactorily filled through intra- and intersystem collaterals.
- 1DV: large branch, in the proximal third from the mouth there is stenosis up to 80%.
- Intermediary artery: large branch, 80% stenosis in the proximal third.
- OA: in the middle segment there is chronic occlusion, the post-occlusion section is satisfactorily filled through intra- and intersystem collaterals.
- RCA: the previously installed stent in the middle segment is passable, without signs of restenosis.
Taking into account the data from the clinical picture, laboratory and instrumental research methods, and coronary angiography, a collective decision was made on the need for surgery to restore the patency of the arteries. Considering all the risks and possible complications, the patient categorically refused coronary bypass surgery and insisted on having coronary stenting. The department's doctors were ready to help him.
Operation stages
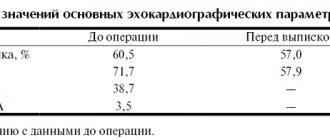
After careful medical preparation, the patient underwent recanalization and stenting of the circumflex branch of the left coronary artery, as well as recanalization of the anterior descending branch of the left coronary artery, followed by bifurcation stenting of the LAD and diagonal branch of the LMCA. The complex operation lasted several hours. However. For the patient, it was painless - the intervention was performed under local anesthesia with novocaine at the puncture area in the femoral artery. During the procedure, the anesthesiologist and surgeons were able to communicate with the patient, he was conscious.
The result of the long and painstaking work of the clinic’s team of doctors was the complete restoration of the patency of all arteries of the heart and, as a result, a significant improvement in the patient’s quality of life.
Acute coronary syndrome (ACS)
Symptoms of acute coronary syndrome
The main symptom of acute coronary syndrome is pain:
by nature - squeezing or pressing, often there is a feeling of heaviness or lack of air;
localization (location) of pain - behind the sternum or in the precordial region, that is, along the left edge of the sternum; pain radiates to the left arm, left shoulder or both arms, neck area, lower jaw, between the shoulder blades, left subscapular area;
More often, pain occurs after physical activity or psycho-emotional stress;
duration – more than 10 minutes;
after taking nitroglycerin the pain does not go away.
OKS forms
Forms of acute coronary syndrome are distinguished by changes in the electrocardiogram (ECG, a method of recording the electrical activity of the heart on paper) - by changes in the ST segment (a segment of the ECG curve that corresponds to the period of the cardiac cycle when both ventricles are completely covered by excitation).
Acute coronary syndrome with ST segment elevation - it reflects the presence of acute complete occlusion (blockage of the lumen) of the coronary artery.
Acute coronary syndrome without ST segment elevation - in the treatment of patients with this form of the disease, thrombolytics (drugs that destroy a thrombus (blood clot) closing the lumen of the vessel) are not used:
myocardial infarction (death of cells in an area of the heart muscle as a result of disruption of its blood supply);
unstable angina (a variant of acute myocardial ischemia, the severity and duration of which is insufficient for the development of myocardial infarction).
Causes
A sudden disruption of the blood supply to the heart muscle, resulting from a discrepancy between the supply of oxygen to the myocardium and the need for it, is the direct cause of the development of acute coronary syndrome. This happens for the following reasons:
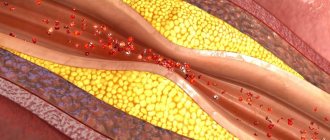
- atherosclerosis of the coronary arteries (feeding the heart muscle) is a chronic disease characterized by hardening and loss of elasticity of the walls of the arteries, narrowing of their lumen due to the so-called atherosclerotic plaques (a formation consisting of a mixture of fats (primarily cholesterol (a fat-like substance that is a “building material”) "for body cells) and calcium) with subsequent disruption of the blood supply to the heart;
- thrombosis (blockage) of the coronary arteries , which occurs when an atherosclerotic plaque breaks off - a formation consisting of a mixture of fats, primarily cholesterol (a fat-like substance that is a “building material” for the body’s cells) and calcium, which can be located in any vessel of the body, and transferring it with the bloodstream to the coronary artery.
The main cause of ACS is the formation of an unstable plaque with a high risk of capsular rupture and the formation of a partially or completely occluding thrombus of the coronary artery, which determines the clinical and electrophysiological picture of coronary pathology. A marker of the formation of an unstable atherosclerotic plaque is an increase in the concentration of pro-inflammatory cytokines (C-reactive peptide) in the blood serum.
ACS, according to the clinical course and dynamics of changes on the ECG, is divided into two subtypes: ACS without ST-segment elevation on the ECG (ACS-BPST) and ACS with ST-segment elevation on the ECG (ACS-PST).
NSTE-ACS - patients with chest pain, but without ST-segment elevation on the ECG.
ACS-PST - patients with typical pain or other unpleasant sensations (discomfort) in the chest, persistent ST-segment elevation, or new-onset left bundle branch block (LBBB).
Patients with suspected ACS, and especially acute MI, should be hospitalized in specialized hospitals to identify the diagnosis, decide on treatment tactics (conservative medication, artificial thrombolysis, mechanical recanalization, endovascular angioplasty, surgery), to monitor the rhythm of cardiac activity and indicators of central hemodynamics.
Factors to the occurrence of acute coronary syndrome include:
- heredity (heart disease is often found in close relatives);
- high level of cholesterol in the blood - a large amount of low-density lipoprotein (a combination of fat and protein) (LDL), or “bad” cholesterol (a combination of fat and protein) low-density lipoprotein (LDL), accumulates in the body, while the level of high-density lipoprotein (HDL), the “good” high-density lipoprotein (HDL) cholesterol, decreases;
- tobacco abuse (smoking tobacco in any form (cigarettes, cigars, pipes), chewing tobacco);
- obesity;
- high blood pressure (arterial hypertension);
- diabetes (a disease associated with an absolute or relative deficiency of insulin, a pancreatic hormone);
- lack of regular physical activity, sedentary lifestyle;
- excessive consumption of fatty foods;
- frequent psycho-emotional stress;
- male gender (men get sick more often than women);
- old age (the risk of getting sick increases with age, especially after 40 years).
Diagnostics
Recognition of ACS is based on three groups of criteria. The first group consists of signs determined during questioning and physical examination of the patient, the second group - data from instrumental studies, and the third - results of laboratory tests.
Typical clinical manifestations of ACS are anginal pain at rest lasting more than 20 minutes, new-onset angina of functional class III, progressive angina. Atypical manifestations of ACS include varied pain in the chest that occurs at rest, epigastric pain, acute digestive disorders, pain characteristic of pleural damage, and increasing shortness of breath. Physical examination of patients with ACS often does not reveal any abnormalities. Its results are important not so much for the diagnosis of ACS, but for detecting signs of possible complications of myocardial ischemia, identifying heart diseases of a non-ischemic nature and determining extracardiac causes of the patient’s complaints.
The main method of instrumental diagnosis of ACS is electrocardiography. The ECG of a patient with suspected ACS should, if possible, be compared with data from previous studies. In the presence of appropriate symptoms, NS is characterized by ST segment depression of at least 1 mm in two or more adjacent leads, as well as T wave inversion with a depth of more than 1 mm in leads with a predominant R wave. Developing MI with a Q wave is characterized by persistent ST segment elevation , for Prinzmetal's angina and developing MI without a Q wave - transient ST segment elevation. In addition to the usual resting ECG, Holter monitoring of the electrocardiosignal is used to diagnose ACS and monitor the effectiveness of treatment.
Of the biochemical tests used to diagnose ACS, the determination of the levels of cardiac troponins T and I in the blood is considered preferable, an increase in which is the most reliable criterion of myocardial necrosis. A less specific, but more accessible criterion for determination in clinical practice is an increase in the blood level of creatine phosphokinase (CPK) due to its isoenzyme MB-CPK. An increase in the content of MB-CPK (preferably mass rather than activity) in the blood by more than twice as compared to the upper limit of normal values in the presence of characteristic complaints, ECG changes and the absence of other causes of hyperenzymemia allows one to confidently diagnose MI.
Symptoms
Against the background of damage to the brachiocephalic vessels, there is a decrease in performance, weakness and dizziness . The brachiocephalic trunk is responsible for the blood supply to the soft tissues of the head and the brain. If the left artery is additionally involved in the pathological process, then the clinical picture worsens significantly. Main manifestations:
- pale skin;
- nausea;
- headache;
- pain during physical activity;
- confusion;
- paraplegia;
- swelling and development of necrosis;
- burning sensation or numbness;
- deterioration of visual perception;
- hallucinations;
- difficulty breathing, swallowing;
- speech disorders;
- cardiopalmus;
- absence of pulse in the affected area.
If any of the above symptoms appear, it is necessary to conduct a thorough analysis and diagnosis to identify the true cause and subsequently prevent the development of severe complications.
Causes
The role of emboli can be:
- foreign bodies;
- tumor fragments;
- blood clots;
- valve vegetations;
- atherosclerotic plaques.
Therefore, the causes of post-embolic occlusions can be listed:
- injuries;
- thrombosis;
- atherosclerosis;
- oncological diseases;
- endocarditis;
- myocardial infarction;
- surgical interventions (especially on blood vessels);
- heart defects;
- aneurysms;
- arrhythmias;
- vascular diseases (arteritis, vasculitis, etc.).
General information
Vascular occlusion is a blockage (more often of arteries than veins), which is characterized by a pronounced decrease in the speed and quality of blood flow. Occlusion can cause necrosis and, as a result, lead to death.
The pathology is quite common and can affect the organs of visual perception, the central nervous system, limbs and great vessels. sepsis and peritonitis develop . Abdominal ischemic syndrome develops against the background of a lack of adequate blood circulation in the digestive tract. The pathology is associated with occlusion of the unpaired visceral branches of the abdominal aorta - the celiac trunk and mesenteric arteries (superior, inferior). Abdominal toad can develop under the influence of both internal ( thrombosis ) and external factors (traumatic occlusion).
What is an occlusive dressing?
This method of sealing the lesion is used for wounds that require maintaining sterile conditions and protection from the external environment.
Applying an occlusive dressing to the knee joint requires certain skills and technique:
- cover the wound surface with sterile gauze;
- Place the top of the scarf on the thigh area and wrap it around the waist;
- bend the bandage at the base by 2 cm;
- cross the ends under the thigh, tie knots on the thigh;
- Throw the top over the knot formed and then pass it under the knot.
Diet for occlusion
To restore the elasticity of the vascular wall, strengthen it and reduce the severity of occlusion, it is recommended to adhere to certain dietary rules. In case of occlusion, it is recommended to adhere to a special cholesterol-lowering diet, which includes:
- Legumes . Beans and legumes are sources of protein, iron, folic acid and contain absolutely no fatty acids.
- Whole grains (wheat bread, buckwheat, oatmeal and brown rice).
- Cabbage (all types, especially broccoli). Prevents salt deposition, normalizes the lipid spectrum of cholesterol, enriches the body with vitamins K and C.
- Asparagus . Helps lower blood pressure and reduce cholesterol in the blood.
- Persimmon . Rich in fiber and has a pronounced antioxidant effect.
- Spinach . Allows you to reduce blood pressure in hypertensive patients.
- Turmeric . It has an anti-atherosclerotic effect, reduces the volume of cholesterol plaques, and reduces the severity of the inflammatory process.
Symptoms
Clinical manifestations largely depend on the location of the occlusion, the timing of the embolism (acute or chronic):
The symptoms of acute occlusion are similar to those of acute arterial thrombosis.
- Chronic occlusion gives the same clinical manifestations as obliterating atherosclerosis.
Occlusion of mesenteric vessels is accompanied by diarrhea, inhibition of intestinal motility, bloating, and shock.
When the carotid arteries are involved, the patient’s speech is impaired, their gait changes, convulsions and hematoparesis appear, and a stroke may occur.
Tests and diagnostics
It is recommended to consult a doctor at the first manifestations of the disease. After examination, collecting anamnesis and assessing the manifestations of clinical symptoms, they begin diagnostics, which includes:
- CT arteriography;
- Doppler ultrasound;
- cerebral angiography;
- MR angiography;
- coagulogram;
- MRI of the brain.
Only after a comprehensive examination is appropriate treatment prescribed, which is selected individually for each patient.