Stenosis is a term used to describe a narrowing of the lumen of any hollow organ or blood vessel. Often stenosis is also called a stricture, for example, urethral stricture is a narrowing of the urethra.
Narrowing of the lumen of an organ inevitably leads to disruption of its function. As a rule, stenosis increases over time and does not go away without treatment. It can act as a symptom or complication of many diseases.
What are the causes of stenosis?
There are many different causes of stenosis. The main ones:
- Congenital malformations (for example, congenital urethral valves, congenital intestinal obstruction due to intestinal underdevelopment).
- Proliferative inflammation of the organ wall is an inflammatory process in which tissue proliferation occurs.
- Scarring of the organ wall after damage, inflammation, or ulcers.
- Benign and malignant tumors.
- In vessels, the cause of stenosis is often blood clots and atherosclerotic plaques.
- Compression of a hollow organ from the outside, for example, by a tumor located in a neighboring organ.
- Hypertrophy of the organ wall - for example, this condition often causes narrowing of the pylorus of the stomach.
- Injuries and osteophytes (bone growths) can cause stenosis of bone canals, in particular the spinal canal.
In which organs can stenosis occur?
Stenosis can occur in any organs that have a lumen, in the heart and in vessels of different diameters, in various anatomical canals. Symptoms of stenosis are very diverse - they depend on the affected organ and impaired functions.
Common types of stenoses:
- Stenoses of the digestive system organs: esophagus, stomach, intestines, bile ducts, pancreatic duct, papilla of Vater (the place where the bile duct and pancreatic duct enter the duodenum).
- Stenosis of the respiratory tract: larynx, trachea, bronchi.
- Stenoses of organs of the cardiovascular system: heart valves, aorta, arteries and veins of different diameters.
- Stenoses of the urinary system organs: ureters, urethra, bladder neck, renal arteries.
- Spinal stenosis. Frequent causes are previous spinal injuries, osteophytes, tumors, herniated intervertebral discs.
- Stenoses in the nervous system: the most striking example is non-communicating hydrocephalus; Among the causes may be tumor processes in the brain and spinal cord.
Book a consultation around the clock +7+7+78
Medical Internet conferences
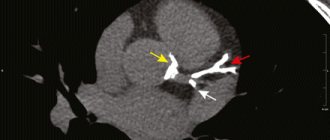
Introduction. The muscular bridge (MM), partially blocking the lumen of the coronary artery, is a congenital anatomical variant and is more common in the LAD. MM causes the development of IHD through two independent mechanisms, depending on its anatomical features (extent, thickness, localization). One of the mechanisms is direct mechanical compression of the LAD at the time of systole, which helps to delay diastolic relaxation of the artery, reduces the blood flow reserve and the severity of perfusion. The second mechanism is an increase in the progression of coronary atherosclerosis, causing stenosis of the LAD proximal to the MM, due to endothelial damage against the background of abnormal hemodynamics (retrograde blood flow to the orifice of the LAD during systole). The anatomical features of MM are associated with the choice of tactics and outcome of intervention in patients with coronary artery disease. Thus, in cases of stenting for an atherosclerotic plaque located proximal to the MM, it is possible to position part of the stent in the area of the MM, which increases the frequency of long-term adverse outcomes, mainly due to disorders in the area of the stented area of the MM. Thus, the anatomical features of MM must be taken into account when diagnosing and choosing treatment tactics for coronary artery disease in patients with this anatomical feature.
Purpose of the study. To determine the effect of the degree of systolic compression of the LAD caused by MM on the incidence of cardiovascular events in the immediate and long-term period after stenting of an atherosclerotic lesion located proximal to the MM.
Material and methods. The prospective study included 17 patients with coronary artery disease who underwent LAD stenting between January 2012 and August 2013. Inclusion criteria were: the presence of a MM in the middle third of the LAD and stenosis located proximal to the MM. IVUS was used to position the stents to prevent unintentional stenting of a portion of the MM. The angiographic effectiveness of stenting was assessed immediately after the procedure, as well as after 6 months. The immediate results were taken into account: the development of myocardial infarction (MI) in the immediate period after stenting, as well as the presence and degree of residual stenosis. As long-term clinical outcomes, the degree of stent stenosis was assessed depending on the initial degree of systolic compression of the artery, as well as the presence of complications (myocardial infarction, the need for repeated revascularization in a given localization, deaths). The presence and degree of residual stenosis was determined by control angiography and IVUS immediately after stenting and 6 months later. In this study, only drug-eluting stents were used.
Statistical processing of the results was performed in the Statistica 7.0 application package; the data are presented in the form “Median (standard deviation)”. Differences in the frequencies of outcomes were determined using Fisher's and c2 tests; differences in unrelated groups by quantitative characteristics were assessed using the Mann-Whitney test.
Results. The average age of the patients included in the study was 56.6 (4.7) years, the number of men was 13. According to the results of coronary angiography (CAG), the myocardial bridge with a maximum degree of narrowing in systole of more than 50% was observed in 8 patients (group I, men - 6, women - 2), and less than 50% - in 9 patients (group II, men - 7, women - 2), the difference between the groups by gender and age was not clinically significant (p(c2) = 0.66, p(U)= 0.45, respectively). In all patients, after stent implantation, restoration of optimal antegrade blood flow was noted.
There were no adverse outcomes in the immediate period (acute coronary circulatory disorders, artery dissections, etc.) in both groups.
During the 6-month follow-up, there were no acute coronary events or the need for repeated myocardial revascularization in patients of both groups I and II.
In the long-term period, the frequency of stent restenosis did not differ in groups of patients with different degrees of systolic compression of the artery: thus, in group 1, restenosis occurred in 2 patients, and in group 2 – in 1 patient (p(c2) = 0.55).
Conclusions. A prerequisite for stenting the LAD with a distally located MM is the use of IVUS to control the positioning of the stent. There was no effect of the degree of systolic compression of the LAD (more or less than 50%) caused by the myocardial bridge on the incidence of adverse events after coronary stenting in the area of a proximal atherosclerotic plaque. Further study of the relationship between the anatomical parameters of the MM and the frequency of restenosis of stents implanted for proximal atherosclerotic lesions of the LAD is necessary.
Stenoses in oncology
Malignant tumors often block the lumen of hollow organs, disrupting their functions. In this case, the patient’s condition always worsens significantly, and the prognosis becomes more serious. If radical surgery for a malignant neoplasm is not possible, then the doctor performs palliative surgery to eliminate stenosis, restore organ function, and improve the patient’s condition.
The patient's condition improves when the tumor begins to disintegrate - it no longer blocks the lumen of the organ. The tumor disintegrates under the influence of chemotherapy, less often on its own. Substances that are released into the blood during massive decay of tumor cells poison the body and can lead to serious complications.
How is stenosis detected?
If stenosis is suspected, the doctor may order the following tests:
- X-ray and fluoroscopy (including contrast-enhanced).
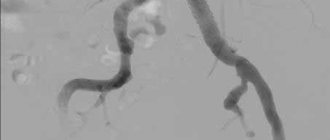
- Angiography is radiography with the introduction of a radiopaque solution into the vessels.
- Computed tomography (CT) and magnetic resonance imaging (MRI). These studies can also be performed with contrast enhancement.
- Ultrasound examination (ultrasound). Dopplerography is also performed - studying blood flow in vessels using ultrasound.
- Endoscopic studies, for example, fibroesophagogastroduodenoscopy (FEGDS) to detect stenosis of the esophagus, stomach, duodenum.
Stenting of vessels and coronary arteries
Coronary artery stenting with angioplasty
This is a modern, low-traumatic operation performed on vessels with atherosclerotic changes and aimed at restoring the lumen of the arteries, most often the coronary artery.
Angioplasty is a medical procedure in which a special balloon is inserted into a vessel damaged by plaque. At the site of damage to the vessel, the balloon is inflated under high pressure, destroys the plaque and presses it into the wall of the vessel.
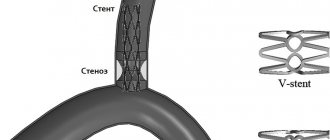
Typically, an additional supporting structure, a stent, is installed in the coronary artery. The stent in its initial state has the form of a mesh metal cylinder made of a special alloy and is compressed and placed on a balloon. When the balloon is delivered to the location of the plaque, it is inflated, the stent expands with it, after which the balloon is deflated and removed from the artery, and the stent remains in it forever.
Indications for vascular stenting
Stenting surgery is performed on patients whose coronary arteries are narrowed due to existing atherosclerotic plaques. Plaques reduce blood flow through the arteries, which leads to a lack of oxygen and nutrients flowing to the heart, and as a result causes angina attacks in the patient.
Indications for surgery are determined for each patient by a cardiac surgeon. Before stenting, coronary angiography is required, which shows how damaged the vessels are, how many stents are available and in which areas of the arteries they need to be installed. Vascular stenting , compared to bypass surgery, does not require an incision in the chest, suturing, or long recovery after surgery. However, the choice in favor of bypass surgery or stenting is made by the attending physician, based on the severity of the damage to the arteries of the heart and the general condition of the patient. Neither one nor the other operation is a panacea and does not exempt the patient from subsequent conservative treatment by cardiologists.
Preparation for vascular stenting
Before the operation, you will be examined in standard quantities that comply with the standards for preoperative preparation. Depending on whether you have any additional concomitant diseases, your attending physician may prescribe additional tests or studies. Vascular stenting surgery is performed on an empty stomach, so several hours before the procedure the patient is prohibited from eating, and, accordingly, all medications intended to correct diabetes are discontinued. Taking other medications is at the discretion of the attending physician. Additionally, before stenting, a drug (clopidogrel) is prescribed to prevent the formation of blood clots in the vessels. As a rule, it is prescribed three days before stenting surgery, but it is also possible to take a significant dose immediately before the procedure. True, the second option is less desirable, as it can lead to some complications from the stomach.
Method of performing stenting surgery
To begin coronary artery stenting surgery, a large artery in the leg or arm is punctured. The choice of access depends on the doctor performing the operation and the individual patient. As a rule, access through the leg (in the groin area) is used because it is simpler and more reliable. A special short plastic tube (introducer) is inserted into the artery through this puncture, which will act as a “gate” for all other instruments. A long plastic tube (catheter) is inserted through the introducer and brought to the damaged coronary artery. A catheter is installed in the artery and through it a stent placed on a special deflated balloon is brought to the site of the atherosclerotic plaque. Vascular stenting is carried out using the most modern X-ray equipment, which allows for precise positioning of the stent balloon at the location of the atherosclerotic plaque.
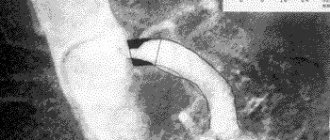
After checking the position of the stent at the site of the plaque in the coronary artery, the balloon is inflated by injecting a contrast agent into it at high pressure. When the balloon is inflated, the stent expands and is pressed into the walls of the vessel, where it remains forever. Angioplasty with stenting usually takes no more than an hour, but the total operation time depends on each specific case.
In case of severe damage to the heart vessels, the operation can last several hours. When a surgeon inflates a balloon containing a stent in a heart artery, blood flow through that coronary artery is temporarily stopped, which can cause chest pain (angina). It is advisable to inform the operating doctor about any pain that occurs so that he can plan his further manipulations.
After the stenting operation is completed, all instruments inserted inside are removed, except for the stent, which, as mentioned above, remains in the human body forever. There are various modifications of stents, which differ in the type of design and the alloy from which it is composed, but usually there are two main groups: simple (“bare”) and drug-eluting (“coated”). There are no ideal stents today.
All of their modifications have their pros and cons, so the choice of an implantable stent ultimately remains with the surgeon, who is based on his own experience and the characteristics of this particular patient. After the operation is completed, the puncture site is sutured or taped, or pressed for a while, and a special bandage is applied to the patient’s limb.
Complications of stenting
When performing balloon angioplasty and stenting, a wide variety of complications can occur, the most common of which are: blockage of the operated artery, damage to the vessel wall, the development of bleeding or the formation of a hematoma at the puncture site, allergic reactions to the contrast agent of varying severity, up to and including impaired renal function.
Considering that blood flow circulates in the human body, in some cases, when performing this operation, complications may arise in other arteries, even those that were not affected by the operation.
People with severe kidney disease, untreated diabetes, and bleeding disorders are more likely to develop complications after stenting and angioplasty surgery.
Therefore, such patients are examined more thoroughly before surgery, additionally prepared, including by prescribing special medications, and subsequently, after the stenting procedure, they are observed in an intensive care unit or resuscitation room.
Stenting surgery does not guarantee complete relief from coronary heart disease. The disease can progress, new atherosclerotic plaques can form in the arteries or existing ones can increase.
And the stent itself can restenose (“overgrow”) or thrombose (“clog”) over time. Therefore, all patients who have undergone coronary artery stenting are under constant supervision of a cardiologist, so that, if necessary, a relapse of the disease is recognized in time and re-referred to a cardiac surgeon.
Stent thrombosis is one of the most dangerous complications after stenting surgery. The most unpleasant thing about it is that no one is immune from it, and it can develop at any time: either in the early or late postoperative period. As a rule, this complication leads to the development of an acute painful attack, and if left untreated, can lead to myocardial infarction. A less dangerous complication, but much more common, is stent restenosis, which develops due to the “ingrowth” of the stent into the vessel wall. In fact, this is a natural process, but in some people it is so active that the lumen of the operated artery narrows greatly, causing the return of angina.
And of course, if you do not comply with drug therapy, diet and regimen prescribed by your cardiologist, the process of formation of atherosclerotic plaques in your body can progress, which will lead to the development of new lesions in previously healthy arteries.
After stenting - recommendations from a cardiac surgeon
After stenting, the patient is on bed rest in the hospital under the supervision of medical personnel.
To prevent bleeding from the punctured artery, the patient after stenting surgery is limited in his movements and is prohibited from moving the limb through which the heart was accessed.
Subsequently, as a rule, after 2-3 days the patient is discharged home with recommendations for a specific regimen and medications. In addition to the standard set of medications selected for you by a cardiologist, a blood thinning drug (clopidogrel) is added for a long period of time (from six months to 2 years). Stopping this medication may cause a blood clot to form in the installed stent.
Cost of stenting
In city hospital No. 40, angioplasty and stenting will be performed for you free of charge when you register a quota for this procedure, or in emergency cases the operation is performed at the expense of compulsory medical insurance.
← Back