Angina pectoris (angina pectoris) is a sharp pain or discomfort in the chest area. The reason for this is a lack of blood supply to certain areas of the heart. Angina pectoris is noted as a leading symptom in coronary heart disease (CHD), which develops due to blockage or narrowing of the blood vessels of the heart. All patients experience approximately the same sensations - pressing or squeezing pain behind the chest, which often radiates to the arm, shoulder, jaw or neck. The pain usually does not last more than 5 minutes and disappears after taking certain medications or relieving tension. However, the duration of the attack is purely individual; some patients experienced pain from 30 seconds to 30 minutes.
Symptoms
When angina occurs, the pain is usually intense and can be relieved by taking nitroglycerin along with stopping physical activity. These pain sensations have characteristic features: a pronounced time of onset and cessation (nature of the attack), occurrence in certain circumstances.
Among the most common conditions for the occurrence of an attack of angina pectoris are active walking (acceleration of movement, climbing a mountain, difficulty in the form of a sharp headwind, heavy load). Also, other physical efforts and significant emotional stress can cause symptoms of angina pectoris. To determine pain arising from physical effort, it is enough to stop the tension. And the discomfort will subside within 5 minutes. The complete elimination of the symptoms of angina pectoris is facilitated by taking nitroglycerin. As a rule, to make a diagnosis, it is enough to take into account the above symptoms and signs: an increase in pain during physical activity, a favorable reaction to nitroglycerin and the nature of the attack.
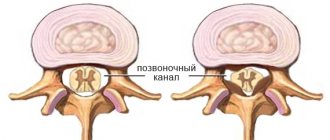
Symptoms of vasospasm
The first sign is a headache, which is accompanied by spasms with a feeling of compression or squeezing of the brain in the temples, eyes, back of the head and forehead.
Symptoms also include:
- Constant ringing in the ears;
- Unpleasant sensations in the head when coughing and sneezing;
- Nausea;
- Fainting;
- Vomit;
- Sharp darkening in the eyes;
- "Floaters" in the eyes;
- Disorientation;
- Radiation of pain to the neck and eyes;
- Problems with remembering and assimilating information;
- Low performance;
- Heavy sweating;
- Sudden fatigue.
Causes
The main phenomenon characterizing the symptoms of angina pectoris is an imbalance between the heart's need for oxygen and its direct supply. Due to lack of nutrition of the muscle, its necrosis can develop.
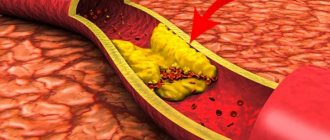
Thus, among the reasons for the lack of oxygen supply to the heart, local disturbances in blood flow are often identified. It can be triggered by chronic narrowing of the lumen of the artery supplying the heart due to atherosclerotic plaque. Angina also occurs due to a sharp and prolonged spasm of the heart vessels. As a result, one part of the heart receives less oxygen than it needs to function properly. During physical activity, this deficiency is felt especially strongly. This is the reason why the vast majority of acute attacks of angina are the result of exhausting and difficult work or stress.
Diagnostics
Not all pain in the chest or heart can be called angina. If it lasts less than 30–40 seconds and is eliminated by taking a deep breath or changing body position, there is no need to worry about angina. To make such a diagnosis, the doctor must analyze your complaints, find out the symptoms and the circumstances of their manifestation. In order to exclude concomitant diseases when diagnosing angina, a number of medical tests are carried out, including an electrocardiogram (ECG) in two states (rest and stress), a stress test, blood pressure measurements and x-rays of the coronary arteries.
Thanks to an ECG, the doctor can determine the electrical impulses of the heart, and with them the symptoms of angina pectoris. They show the absence or presence of ischemia (lack of blood supply), characteristics of changes in heart rate and some other parameters. To get a complete picture of cardiac activity, the specialist compares the ECG readings after exercise and at rest, and then decides on the need to treat angina pectoris.
A comprehensive stress test makes it possible to diagnose angina pectoris and assess blood flow in the heart muscle. A small amount of a radioisotope (usually thallium) is used, which is injected into a vein by microinjection during physical activity. Using a special device, the doctor monitors the distribution of thallium in the heart. Uneven concentration or absence of this element in one or another part of the muscle reveals areas of insufficient blood supply.
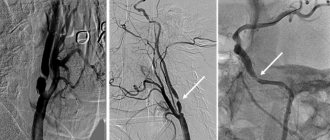
The most accurate way to determine angina pectoris (angina pectoris) is an angiogram, or x-ray of the coronary artery. The catheter is placed in an artery in the groin or forearm, and then it moves along the bloodstream to one of the heart arteries. Next, a radiopaque liquid is injected, which makes it possible to observe changes in the arteries under study, diagnosing angina pectoris.
Forms of coronary disease
Classification of IHD (ICD-10; 1992)
- Angina pectoris
- — Stable angina pectoris
- - Unstable angina
- Primary myocardial infarction
- Recurrent myocardial infarction
- Old (previous) myocardial infarction (post-infarction cardiosclerosis)
- Sudden cardiac (arrhythmic) death
- Heart failure (myocardial damage due to ischemic heart disease)
The main cause of impaired oxygen supply to the myocardium is the discrepancy between coronary blood flow and the metabolic needs of the heart muscle. This may be a consequence:
- — Atherosclerosis of the coronary arteries with a narrowing of their lumen by more than 70%.
- — Spasm of unchanged (little changed) coronary arteries.
- — Microcirculation disorders in the myocardium.
- - Increased activity of the blood coagulation system (or decreased activity of the anticoagulation system).
The main etiological factor in the development of coronary heart disease is atherosclerosis of the coronary arteries. Atherosclerosis develops consistently, in waves and steadily. As a result of the accumulation of cholesterol in the artery wall, an atherosclerotic plaque is formed. Excess cholesterol leads to an increase in plaque size and obstructions to blood flow. Subsequently, under the influence of systemic unfavorable factors, the plaque transforms from stable to unstable (cracks and ruptures occur). The mechanism of platelet activation and the formation of blood clots on the surface of an unstable plaque is triggered. The symptoms worsen with the growth of atherosclerotic plaque, which gradually narrows the lumen of the artery. A decrease in the lumen area of the artery by more than 90-95% is critical, causing a decrease in coronary blood flow and deterioration of well-being even at rest.
Risk factors for coronary heart disease:
- Gender (male)
- Age >40-50 years
- Heredity
- Smoking (10 or more cigarettes per day during the past 5 years)
- Hyperlipidemia (plasma total cholesterol > 240 mg/dL; LDL cholesterol > 160 mg/dL)
- Arterial hypertension
- Diabetes
- Obesity
- Physical inactivity
Treatment
Successful treatment of angina is usually associated with a reduction in risk factors that can cause cardiovascular problems. These include: high blood pressure, excess cholesterol, excess weight, smoking. The doctor will prescribe you all the necessary medications to bring your blood pressure back to normal, suggest the right diet and help you create a physical exercise program for the treatment of angina pectoris.
Currently, mononitrates, dinitrates and trinitrates are used to relieve the symptoms of angina pectoris. Their mechanism of action is dilation of the blood vessels of the heart, which increases the flow of oxygen and reduces tension in the myocardial wall. Undesirable effects of nitrates in the treatment of angina include headache, decreased blood pressure, facial flushing, dizziness, and insensitivity to certain doses of the drug. Beta blockers, which reduce the strength and frequency of the heartbeat, and calcium channel blockers, which prevent vasospasm, are also used.
In cases where the symptoms of angina are severe and medications are not able to help, surgery (in the form of coronary artery bypass grafting) and balloon angioplasty are prescribed. Coronary artery bypass grafting involves the implantation of a blood vessel into a blocked section of the coronary artery. In this way, blood flow in this part of the heart is restored using a bypass. Angioplasty is an operation to treat angina using a catheter with a small balloon at the end. It is injected into the axillary or femoral artery and then advanced to the site of narrowing of the coronary vessel. Here it quickly inflates or stretches, eliminating the spasm.
Particular attention needs to be paid to the treatment of unstable angina, which can occur even in the absence of strain. Such chest pain does not have predictable boundaries of onset, unlike stable angina, and does not need a reason for its occurrence.
Coronary artery stenosis - symptoms and treatment
There are two groups of treatment methods:
- conservative and medicinal;
- surgical.
In the early stages of the disease, conservative treatment . It involves changing your lifestyle towards a healthy one, giving up bad habits, optimizing your level of physical activity and following a low-cholesterol diet. Meals should be fractional. The consumption of salt, sweets, alcohol, fatty meats and baked goods is limited. The diet includes vegetable oils, fish oil and complex carbohydrates found in cereals. It is also important to drink up to 2 liters of liquid and change the principle of cooking: foods should be boiled, stewed or baked.
For coronary heart disease, medications are prescribed , for example:
- hypocholesterol drugs - reduce blood cholesterol levels (statins, fibrates, PCSK9 inhibitors, ezetimibe);
- disaggregants and anticoagulants - “thin” the blood, reduce its coagulability and viscosity, prevent the formation of blood clots (acetylsalicylic acid, clopidogrel, warfarin, apixaban, rivaroxaban, dabigatran, prasugrel);
- antianginal - dilate blood vessels, prevent attacks of angina (nitroglycerin, amlodipine, sidnopharm, bisoprolol, ranolazine);
- angioprotectors - protect blood vessels from damage and stretching (ACE inhibitors);
- medications to stabilize blood pressure, reduce heart rate and prevent arrhythmias - diuretics (indapamide, hypothiazide, torsemide), ACE inhibitors (ramipril, perindopril), beta-blockers (metoprolol, bisoprolol) and ivabradine;
- metabolic - normalize metabolism (trimetazidine, neoton).
The duration of use for each drug is different. Dose adjustments and replacement of medications are carried out strictly under the supervision of a physician.
Surgical treatment includes two main types of treatment for coronary artery stenosis:
- stenting;
- shunting.
Stenting involves installing a stent into a narrowed vessel. The stent is a metal frame. Using a guide through the femoral or radial artery, this frame is advanced to the affected coronary artery, fixed there and straightened. It prevents the artery from narrowing and normalizes blood flow.
Stenting is performed both planned for the prevention of myocardial infarction and urgently. The operation is minimally invasive: it does not require extensive incisions or general anesthesia.
Bypass surgery aims to create a new blood flow path around the blocked vessel. The material for the shunt is the patient's own veins and arteries. The surgeon stitches them above and below the narrowing of the coronary artery.
Such manipulation involves opening the chest, often leading to long rehabilitation and serious complications, such as ischemic stroke, anemia, arrhythmia, blockage of shunts with a blood clot, prolonged healing of the sternum with the formation of a false joint and the formation of fluid in the lungs, swelling and long healing of the leg [1] [2][3][4][5][6][7][8][9][10][13][14][15][16][17][18][19][20 ][21].
There is also a third surgical method for treating stenosis - endarterectomy . It involves removing a blood clot and cholesterol plaque from the lumen of the heart artery. However, now endarterectomy is practically not used, since it is accompanied by high risks and does not exclude the re-formation of blood clots.
Prevention
Basic methods of prevention and treatment of angina:
- absolute cessation of smoking and alcohol;
- long walks in a relaxed manner, physical activity within reasonable limits in accordance with doctor’s prescriptions;
- blood pressure control;
- You should follow the diet prescribed by your doctor, limit the consumption of animal fats and salt, increase the use of vegetables, vegetable fats and fruits in your diet;
- detection and appropriate treatment of diabetes mellitus, control of blood glucose levels;
- absence of unnecessary emotional stress.
If you are bothered by regular pain in the chest area during physical activity, this may be a manifestation of stable or unstable angina, which is treated by specialists at our clinics. You should consult a doctor, as each attack of angina inevitably worsens the condition of the heart muscle. You can get professional help at one of our clinics in Moscow. Make an appointment with us by phone +7.