The article will present the Braunwald classification of unstable angina.
With ischemic heart disease, angina attacks almost always occur. Severe pain develops when the myocardium begins to lack oxygen. When the syndrome develops against the background of physical activity, we are talking about stable angina pectoris, which accompanies increased heart activity. However, the following situations also occur: severe symptoms in the form of painful pressure in the chest, burning and suffocation are in no way related to the activity of the heart muscle. An anginal attack can strike a person suddenly, and it is impossible to predict its occurrence. In this case we are talking about unstable angina. In accordance with the tenth edition of the International Classification of Diseases, pathology refers to diseases of the circulatory system and has its own code 120.0.
Braunwald's classification of unstable angina will be presented below.
Stable and unstable angina
The very name of unstable angina characterizes the complex of symptoms that arise. The condition can manifest itself without reference to physical activity or other provoking factors. This is precisely the main difference between the pathology in question and stable type angina.
Stable angina is characterized by the presence of a certain set of provoking factors:
- Emotional stress.
- Unfavorable weather with snow, rain, cold wind.
- Established boundaries for physical activity (for example, walking at a fast pace for a distance of more than half a kilometer, climbing stairs higher than the first floor).
Stable angina can have one of four functional classes, each of which has certain permissible levels of physical activity and its own degree of severity of clinical symptoms.
An attack of stable angina stops with rest, can last a maximum of 15 minutes, and is effectively stopped by using Nitroglycerin.
With unstable angina, there is a great danger to the patient’s life, since it is impossible to predict its occurrence and clinical picture, there is no way to determine the permissible level of stress for the patient, and it is difficult to identify provocative factors. Any of these attacks occurs suddenly, is unpredictable in its manifestation, threatens the onset of myocardial infarction, and the patient may die from sudden cardiac arrest. In this case, the symptoms are more severe. An attack can last up to half an hour, and Nitroglycerin is not always effective.
Forecast
Since the unstable form manifests itself unpredictably, the prognosis for patients with such angina can hardly be called favorable. The course of the disease quickly worsens, attacks become more frequent, longer, and more severe. Their development is difficult to predict. The most common outcome is myocardial infarction.
The most successful result will be the result of surgical treatment. Patients can expect to return to a normal lifestyle with few restrictions if they strictly follow the instructions of their doctor and try to completely change their habits and attitude towards stress.
The seriousness of the complications caused leaves no doubt, so timely consultation with a doctor is simply necessary for any pain in the heart area. Unstable angina does not occur on its own. Anyone can maintain their health at an optimal level. To do this, you need to have an accurate understanding of the harm of provoking factors and be able to control yourself and your habits.
Causes of development of unstable angina
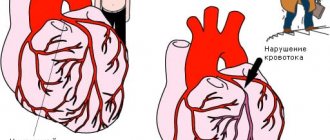
An attack in coronary artery disease occurs when a prerequisite is present - the patient has a violation of the coronary circulation and narrowing of the arteries. Excess cholesterol settles on the vascular walls, atherosclerotic plaques appear, as a result of which the lumen of the artery decreases. Thus, not enough blood flows to the heart. In such conditions, the myocardium begins to work more intensely to replenish the insufficient level of blood supply, but the situation only gets worse. This is due to the fact that the heart, during intense activity, requires an even greater amount of oxygen, which comes exclusively from the blood.
When arterial patency deteriorates by more than 50%, hypoxia increases, which reaches critical limits. Metabolic processes begin to disturb the cells, which is accompanied by pathological changes in intracellular structures. At such moments a person experiences unbearable angina pain. Due to a prolonged attack, tissue necrosis begins and spreads, resulting in myocardial infarction.
IHD and angina pectoris (ICD code 10 I20) develops when the heart has an acute need for large portions of oxygen (stress, physical activity), and damaged coronary vessels are not able to supply the heart muscle with a sufficient volume of blood.
When an atherosclerotic plaque grows to an impressive size, there is a possibility of a violation of its integrity. This happens in cases where there are a lot of fat deposits and not enough collagen, and the vascular wall is inflamed or the blood has increased viscosity. The detached part of the plaque is glued together by platelets, resulting in the formation of a blood clot that can partially or completely block the arterial lumen. This is the main cause of unstable angina. Such blood clots can migrate and penetrate into any part of the coronary vessels.
Another reason for the development of coronary artery disease and angina pectoris (ICD code 10 I20) pathology is sudden spasms of the coronary vessels that occur regardless of physical activity. In this case, arteries that are not affected by atherosclerosis can narrow. A similar situation is typical for vasospastic angina (Prinzmetal), which is a rather rare pathology.
Mechanism of pathology
The blood supply to the heart muscle requires a constant supply of sufficient blood through the coronary arteries. The heart's need for oxygen changes depending on the conditions: physical activity, complete immobility, excitement, intoxication of the body due to infectious diseases.
In contrast to the calm state, tachycardia occurs (increased heart rate). It requires more energy, which means oxygen consumption increases, since the heart muscle cells “extract” calories for themselves only in its presence.
If the patency of the coronary arteries is good, blood flows in sufficient quantities to compensate for the necessary costs. What happens if one or all arteries are narrowed? The working heart will experience a state of “hunger”, tissue hypoxia. Clinical symptoms can be called a “cry for help.”
Provoking factors
In addition to the main reasons for the development of unstable angina attacks, experts identify some additional factors that can increase the risk of severe exertional angina. Among them:
- Diseases not related to the heart (diabetes mellitus, pathological changes in the thyroid gland, iron deficiency anemia).
- Pathologies of a cardiac nature (heart defects, hypertrophic cardiomyopathy, condition after a heart attack, chronic myocardial failure).
- The harmful effects of ethyl and tobacco tar.
- Progressive hypertension.
- Strong mental stress, stressful situations, strong emotionality.
- Increased vascular susceptibility to the effects of vasoactive substances, such as serotonin.
- Increased cholesterol levels in the blood.
- Morphan's disease.
- Unfavorable heredity.
- Obesity.
- Insufficient rest, disturbances in night sleep.
- Physical inactivity.
- Excessive physical activity.
Symptoms of rest angina
An attack of anginal pain with angina at rest develops with complete physical calm, most often at night or early in the morning. From a sudden attack, the patient is forced to wake up from sudden suffocation or a feeling of tightness in the chest. An attack of angina at rest is accompanied by the following symptoms: a state of increased anxiety, anxiety, fear of death. The pain is intense, localized behind the sternum, has a compressive, pressing nature, spreading to the jaw, left arm, and shoulder blade.
Braunwald classification of unstable angina
What is this classification? On what principle is it built?
The most widely used classification is the system of Evgeniy Braunwald. In accordance with it, several classes and levels of pathology are distinguished:
- Class “A” has secondary angina pectoris. Symptoms of the pathology in this case develop under the influence of factors of extracoronary origin, which contribute to the worsening of ischemia: strong emotional outbursts, difficult to treat hypertension, hypotension, instability of the heart rate, infectious attack, fever, anemia. How else are heart diseases classified according to Braunwald?
- Class “B” includes primary angina syndromes. They develop against the background of cardiac pathologies and disorders in the coronary circulatory system.
- According to the Braunwald classification of unstable angina, class “C” is a pathology that is diagnosed against the background of a myocardial infarction (during the first two weeks after it).
Classes of unstable angina, in accordance with this classification, reflect the circumstances of the development of ischemic symptoms, characterized by an unstable manifestation.
The Braunwald classification table for unstable angina is presented in the article.
What are the complications?
A form of unstable angina without proper treatment leads to complications such as myocardial infarction, ventricular fibrillation (a disorder of heart contractions with a frequent and erratic rhythm). And this could already end in death.
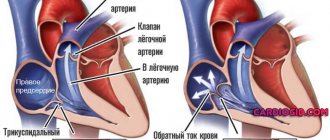
The danger of this form of pathology lies in its development into a heart attack, acute heart failure with simultaneous pulmonary edema, as well as thromboembolism of the pulmonary arteries. Therefore, you should not risk your own life, and when the first symptoms of the disease appear, you should immediately see a doctor.
Classification depending on the severity of the attack
The pathology is also classified into groups that characterize the severity of the resulting anginal attack:
- The first group includes angina pectoris, which was recorded for the first time within a month before the day the patient consulted a doctor. Such angina pectoris manifests itself stably in conditions of physical activity.
- The second group includes subacute syndromes. The attacks that occur have a more severe course and can manifest themselves at rest. Occurs within a month before contacting a specialist, with the exception of the last two days.
- Angina pectoris of the third group is characterized by acute manifestation of symptoms. Angina pain occurs without reference to physical activity during the last two days.
Many people are interested in what it is - angina pectoris. Its symptoms are very unpleasant. A sudden attack of acute pain in the chest in most cases is a sign of chronic angina pectoris (other names are angina pectoris, acute coronary insufficiency, angina pectoris).
It is the paroxysmal nature of the painful sensations that makes it possible to accurately diagnose the disease. Angina pectoris is considered a form of cardiac ischemia. The most serious complication of the disease is myocardial infarction.
Typical signs of Prinzmetal's angina
New York cardiologist M. Prinzmetal described a type of angina pectoris in 1959, which is included in the modern classification of unstable forms of angina pectoris. In pathogenesis, great importance is attached to the increased tone of the vagus nerve.
Features of the clinic:
- occurs more often in young men;
- attacks of pain occur at rest, there are characteristic ECG changes;
- patients do not complain of pain during physical activity and tolerate it well;
- attacks often occur in the morning rather than during the day or at night;
- good effectiveness in treatment with drugs from the group of nitrates and calcium antagonists.
The prognosis of this form is unfavorable due to the high probability of transition to acute myocardial infarction.
Symptoms of unstable angina
There is no difference between the symptoms of different types of angina. For any type of pathology, the patient indicates the manifestation of the following symptoms:
- Sharp jumps in blood pressure.
- Nausea.
- Weakness.
- Dizziness.
- The appearance of anxious thoughts.
- Increased heart rate.
- Increased sweating.
- Feeling of suffocation.
- Pain in the chest, heart, having a compressive nature.
- Pain in the lower back, shoulder blades, teeth, stomach, arms.
These are the symptoms of angina pectoris. What it is is now clear.
Differences in unstable angina
Unstable angina can be distinguished by the following signs:
- Symptoms progress during an attack, the attack is more difficult to bear, pain affects adjacent areas (jaw, back, neck, left arm).
- An anginal attack has acute manifestations (feeling of heaviness in the chest, heat, squeezing) and, along with suffocation, occurs more and more often.
- For an attack to occur, less and less load is required each time; angina pectoris can occur even at rest.
- Signs of acute ischemic disorders were detected after coronary artery bypass surgery, no later than 90 days before contacting a specialist.
- The pain is poorly relieved by the use of Nitroglycerin.
- The paroxysm lasts more than a quarter of an hour.
- Prinzmetal's angina occurs, as a rule, in males, and it develops regardless of their physical activity. Between attacks, the patient is able to withstand severe muscle tension without consequences. More often, heart pain appears in the morning. They are provoked by spasms in the coronary arteries, in which atherosclerotic changes are not always observed. The pathological condition is characterized by rapid progression and carries a high risk of myocardial infarction.
How to get rid of heart pain due to angina pectoris?
Prognosis: is there a chance of recovery?
The answer to this question sounds disappointing: absolute recovery will not be achieved. But don't rush to panic. In the 21st century, almost all diseases have a chronic course: hypertension, diabetes, obstructive pulmonary disease, and so on. The causes of these pathologies are not bacteria, which doctors have successfully learned to fight, but lifestyle and environmental conditions.
The basis of coronary heart disease is atherosclerosis, which begins to develop with the birth of a person. Unstable angina is an acute manifestation of this process. By removing the symptoms by stenting, we do not destroy the root cause. To prevent new exacerbations, constant use of medications is necessary to prevent pathologies from progressing.
All patients want to minimize the use of pharmaceutical drugs, and some of them stop treatment after relief occurs. In their understanding, discharge from the hospital means freedom from medications, because there is no more pain. Unfortunately, such a decision often turns against them with serious consequences - a hospital bed and life-threatening complications.
In conclusion, I would like to add that cardiovascular diseases cannot always be defeated, but it is quite possible to prevent them. Weight control, smoking cessation, regular physical activity, normal cholesterol and glucose levels will help you in the fight for your health.
An important part of my work is preventive education of patients. Everyone does their own thing, and mine is to help people get rid of heart problems. Since this can only be done in the early stages of development of the pathology or at the stage of formation of a predisposition to it, I pay a lot of attention to issues of nutrition, lifestyle and screening. Only in this way - together - can we significantly improve the health of the nation.
Diagnostics
The diagnosis is established based on the patient’s complaints about the progression of angina attacks, medical history, and the results of various laboratory and instrumental studies:
- Analyzes of samples of biological fluids.
- Coronary angiography.
- Echocardiography.
- Centigraphy.
- Daily monitoring using the Holter method.
Due to the fact that the symptoms may be atypical, differential diagnosis should be carried out and myocarditis, mitral valve disease, pneumonia, esophagitis, pleurisy, osteochondrosis, pancreatitis, and gastrointestinal disorders should be excluded.
Treatment
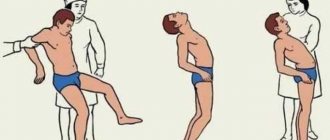
Treatment of unstable angina should be carried out exclusively in a hospital setting. When an attack occurs, the patient should call emergency assistance, while waiting for it to take Nitroglycerin and Aspirin. After admission to the hospital, the patient is provided with assistance according to the following algorithm:
- Elimination of pain syndrome.
- Removing obstacles to normal blood circulation.
- Providing measures to prevent sudden cardiac arrest and the onset of the acute phase of myocardium.
- Rehabilitation therapy to stabilize the condition.
Medicines
After stopping the attack, the patient is prescribed a special diet, bed rest, complete emotional rest, and taking special medications, including:
- Nitrates (“Isosorbide dinitrate”, “Nitroglycerin”). Able to dilate coronary arteries and reduce myocardial oxygen demand.
- Antiplatelet agents, anticoagulants (“Fraxiparin”, “Aspirin”). To prevent the formation of blood clots and increase blood flow.
- Metabolic drugs.
- Calcium channel inhibitors (Verapamil, Cinnarizine), which improve patency in the coronary arteries.
- Painkillers (narcotic origin, antipsychotics), for example, Fentanyl, Droperidol. Indicated for the relief of acute pain.
- Statins (Lovastatin, Rosuvastatin), which help lower cholesterol levels and prevent the formation and hardening of cholesterol plaques.
- Beta blockers (“Proprnalol”, “Carvedilol”), which reduce the heart rate and improve blood flow.
Publications in the media
Unstable angina includes several clinical situations: • New-onset angina pectoris • Progressive angina pectoris (characterized by an increase in angina attacks and/or an increase in their duration and strength) • Angina pectoris that first appeared at rest.
Every patient with unstable angina must be hospitalized, because further development of the disease is unpredictable.
Statistical data. In the United States, approximately 750,000 patients are hospitalized each year for unstable angina.
Etiology - see Stable angina pectoris.
Pathogenesis . Rupture of the fibrous plaque capsule in the coronary artery, which provokes the formation of a blood clot with incomplete closure of the lumen of the vessel. The presence of a thrombus in the coronary artery prevents adequate blood supply to the myocardium, which leads to pain and full-blown unstable angina. The rupture of fibrous plaque is facilitated by the accumulation of large amounts of lipids and insufficient collagen content, inflammation and hemodynamic factors. Other mechanisms responsible for the development of unstable angina include: • intraplaque hemorrhage due to rupture of the vasa vasorum • increased platelet aggregation • decreased antithrombotic properties of the endothelium • local vasoconstriction due to the release of vasoactive agents such as serotonin, thromboxane A2, endothelin in response to disrupt the integrity of the fibrous plaque.
Classification. There is no generally accepted classification. In practice, the Braunwald classification (1989) is often used, dividing unstable angina into three classes (the higher the functional class, the greater the likelihood of complications).
• Class I - new angina or worsening of existing angina within a month.
• Class II - angina at rest during the previous month.
• Class III - angina at rest during the last 48 hours.
Clinical manifestations. Unstable angina pectoris is manifested by typical attacks, however, when collecting an anamnesis, characteristic signs of progression of angina pectoris can be identified.
• Over the past 1–2 months, the number, severity and duration of angina attacks (so-called crescendo angina) have increased.
• Attacks have never occurred before, appeared no more than 1 month ago (new-onset angina, de novo angina).
• Angina attacks began to appear at rest or at night.
• An important clinical sign is the absence or decrease in the effect of nitroglycerin, which previously stopped attacks of angina.
Diagnosis and differential diagnosis. The leading clinical manifestation of unstable angina is pain. The main condition with which unstable angina should be differentiated is MI, primarily small-focal (without a Q wave).
• ECG for unstable angina - changes in the final part of the ventricular complex (similar changes in MI with a Q wave) •• ST segment depression in 30% of patients •• T wave inversion - in 20% •• transient ST segment elevation - in 5%. A normal ECG does not exclude the presence of unstable angina. A resting ECG helps differentiate between large focal MI and unstable angina, since the former has an abnormal Q wave.
• Daily ECG monitoring allows you to identify changes characteristic of unstable angina, especially episodes of silent myocardial ischemia.
• Enzyme diagnostics. With MI, the following changes occur (unlike unstable angina): •• The MB fraction of CPK increases after 6–12 hours •• The myoglobin content increases after 3 hours •• Troponin T and troponin I react simultaneously with the MB fraction of CPK.
• EchoCG is not very informative (pathological movement of the walls of the left ventricle can be detected only during a painful episode).
• Coronary angiography is indicated when discussing the surgical treatment of unstable angina (percutaneous transluminal coronary angioplasty or coronary bypass surgery) or in patients with prognostically unfavorable signs of the disease. Angiographic examination can detect thrombi in the coronary arteries (in 40% of patients) and stenosis of the coronary arteries (in 40–60% of patients). At the same time, 15% of patients may have hemodynamically insignificant stenosis of the coronary arteries (narrowing of the artery lumen less than 60%), which confirms the greater importance of the nature of the fibrous plaque in the development of unstable angina than the severity of the stenosis.
TREATMENT
General tactics • Emergency hospitalization • Sharp limitation of physical activity • Relief of pain • Drugs to reduce myocardial oxygen demand • Anticoagulant and antiplatelet therapy.
Relief of pain syndrome. Administration of nitroglycerin solution at a dose of 5–10 mcg/min IV, increasing every 15 minutes by 5–10 mcg/min (up to 200 mcg/min) until pain disappears or a side effect appears in the form of arterial hypotension. After 24 hours, transfer to oral nitrates is carried out - isosorbide dinitrate or isosorbide mononitrate. Reduced myocardial oxygen demand
• b-Adrenergic blockers - propranolol 1-5 mg IV on the first day to all patients in the absence of contraindications. Subsequently, long-acting beta-blockers orally (for example, metoprolol retard, atenolol). Dosages are selected individually with the calculation of reducing heart rate to 55–60 per minute.
• If there are contraindications to the use of beta-blockers, slow calcium channel blockers (verapamil and diltiazem) are used. In the absence of sufficient antianginal effect from monotherapy, it is possible to use combination therapy - nitrates and beta-blockers, nitrates and slow calcium channel blockers.
Antiplatelet and anticoagulant therapy
• Acetylsalicylic acid at a dose of 75–325 mg/day (antiplatelet agent).
• If there are contraindications to taking acetylsalicylic acid, clopidogrel can be used at a dose of 75 mg 2 times a day.
• Anticoagulants •• Heparin - at an initial dose of 80 IU/kg (5000–7000 IU) intravenously, and then dropwise at 18 IU/kg/h (up to 1500 IU) for 1–2 days, followed by switching to subcutaneous administration at the same daily dose for several days. Heparin treatment is carried out under the control of PTT, which should be 2–2.5 times higher than the initial one (within 45–70 s) •• Low molecular weight heparins (calcium nadroparin, sodium enoxaparin) are prescribed 2 times/day subcutaneously.
Endovascular methods and coronary bypass surgery are performed according to general indications (see Atherosclerosis of the coronary arteries). Autovenous veins are preferred as shunts.
Flow. With adequate therapy, the condition of most patients (80%) improves within 24–48 hours. If there is no effect of drug treatment after 48 hours, surgical treatment methods (percutaneous transluminal coronary angioplasty with the installation of stents or coronary artery bypass grafting) should be considered. Indications for surgical intervention and the choice of method are similar to those for stable angina.
Forecast. Within 3 months, 10–20% of cases develop MI with a mortality rate of 4–10%. Sudden cardiac death is also possible. Prognostically unfavorable signs of unstable angina: • duration of pain more than 20 minutes • night pain • repeated pain with increasing duration • depression of the ST segment more than 1 mm • deep negative T waves • increased content of the MB-fraction of CPK • increased concentration of troponin T or troponin I • History of MI • History of coronary artery bypass grafting • Unstable hemodynamics (low blood pressure, labile pulse).
ICD-10 • I20.0 Unstable angina