Indicators of normal sizes
In the human body, the ventricular system consists of several cavities that anastomize with each other. They communicate with the subarachnoid space, as well as the spinal cord canal. A special liquid, cerebrospinal fluid, moves directly inside the cavities. With its help, tissues receive nutrients and oxygen molecules.
The largest intracerebral hollow formations are, of course, the lateral ventricles. They are localized below the corpus callosum - on both sides of the midline of the brain, symmetrical relative to each other. In each, it is customary to distinguish several sections - the anterior and lower, as well as the posterior horns and the body itself. The shape resembles the English S.
The normal size of the ventricles is assessed taking into account individual anatomical characteristics - there are no uniform standards. Experts focus on average parameters. It is important to know these sizes for babies under one year old - for the purpose of early diagnosis of hydrocephalus.
Normal values for children:
| Anatomical unit | Newborns, mm | 3 months, mm | 6 months – 9 months, mm | 12 months, mm |
| Lateral ventricle | 23.5-/+ 6.8 | 36.2 -/+3.9 | 60.8-/+6.7 | 64.7-/+12.7 |
For adults, the parameters should be in the range - the anterior horn of the lateral ventricle is less than 12 mm in people under 40 years of age, while its body is 18–21 mm in people under 60 years of age. Exceeding the age-related size of the brain ventricles by more than 10% requires additional research to identify and eliminate the root cause.
Ventricular system of the brain
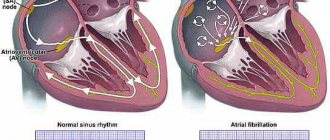
The ventricles of the brain are several interconnected collectors in which the formation and distribution of liquor fluid occurs.
Liquor washes the brain and spinal cord. Normally, there is always a certain amount of cerebrospinal fluid in the ventricles. Two large collectors of cerebrospinal fluid are located on either side of the corpus callosum. Both ventricles are connected to each other. On the left side is the first ventricle, and on the right is the second. They consist of horns and a body. The lateral ventricles are connected through a system of small holes to the 3rd ventricle.
In the distal part of the brain, between the cerebellum and the medulla oblongata, there is the 4th ventricle. It is quite large in size. The fourth ventricle is diamond-shaped. At the very bottom there is a hole called the diamond-shaped fossa.
Proper functioning of the ventricles allows cerebrospinal fluid to enter the subarachnoid space when necessary. This zone is located between the dura mater and the arachnoid membrane of the brain. This ability allows you to maintain the required volume of cerebrospinal fluid in various pathological conditions.
In newborn babies, dilatation of the lateral ventricles is often observed. In this condition, the horns of the ventricles are enlarged, and increased accumulation of fluid in the area of their bodies may also be observed. This condition often causes both left and right ventricle enlargement. In differential diagnosis, asymmetry in the area of the main brain collectors is excluded.
Classification
The main criteria for separating dilatations of the lateral ventricles in the brain are the size of the cavities, the etiology of the dilation, the age of the patient, and the localization of pathological changes.
Each neurologist chooses the optimal classification of the disorder for himself. However, most doctors adhere to the average principles of diagnosis:
- According to the time of expected appearance of the lesion in the brain:
- prenatal period;
- detection of enlarged cerebral ventricles in newborns;
- expansion of brain cavities in adults.
- By localization:
- left ventricle enlargement;
- right-sided lesion;
- bilateral defeat.
- By etiology:
- post-infectious ventricular dilatation;
- post-traumatic changes;
- toxic expansion;
- tumor focus in the brain;
- vascular diseases.
- By severity:
- slightly enlarged ventricles of the brain in infants;
- moderate dilatation;
- severe changes in the ventricles.
Additionally, the specialist can indicate in the diagnosis whether complications are present - for example, hydrocephalus or intellectual/neurological problems.
Causes
The stages of development of the central nervous system in humans provide that as the size of the brain increases, the parameters of the ventricles will also change. For each period, the reasons for dilatation of the lateral cavities have their own characteristics.
In general, the main provoking factors will be as follows:
- brain injuries or falls;
- neuroinfections - for example, meningitis or congenital syphilis;
- brain tumors;
- thrombosis of cerebral vessels;
- strokes;
- abnormalities in the development of brain structures - for example, the anterior horns of the ventricles.
The mechanism for the development of dilatation is the overproduction of cerebrospinal fluid, or a violation of its adsorption/outflow from the cavities of the brain.
In some cases, it is not possible to determine the exact cause of the expansion of the cavities - the idiopathic version of the disorder. The doctor will select the treatment regimen taking into account the main clinical signs. Less often, the basis of dilatation is seen as an atypical anlage of brain structures - it is necessary to carefully collect an anamnesis from the child’s mother, what diseases she suffered during pregnancy. Sometimes the pathology is hereditary in nature - genetic abnormalities.
The size of the ventricles is normal
In infants, the ventricles are often dilated. This condition does not at all mean that the child is seriously ill. The dimensions of each ventricle have specific values. These indicators are shown in the table.
| Anatomical structure | Depth in mm. |
| First and second ventricles (lateral) | 4 |
| Third ventricle | 5 |
| Fourth ventricle | 4 |
To assess normal indicators, the determination of all structural elements of the lateral ventricles is also used. The lateral cisterns should be less than 4 mm deep, the anterior horns between 2 and 4 mm, and the occipital horns between 10 and 15 mm.
Symptoms
At the initial stage of formation of dilated ventricles of the brain in an infant, any special clinical signs may not be detected - the child behaves according to the age norm. After all, adaptation mechanisms are capable of combating overproduction of cerebrospinal fluid.
However, as the expansion of the lateral ventricles of the child’s brain increases, he begins to worry about the consequences of hydrocephalus - pathological pressure on the brain structures due to tissue swelling. The main signs of intracranial hypertension:
- frequent attacks of headache;
- slow growth of fontanelles;
- swelling of tissue between the sutures of the skull;
- nausea and vomiting without improvement of well-being;
- decreased appetite, frequent regurgitation;
- worsening sleep;
- throwing the head back;
- muscle hypertonicity;
- lack of interest in current events, apathy;
- tendency to epilepsy.
In adult patients, a violation of the outflow of cerebrospinal fluid from the lateral ventricles is manifested by a feeling of constant distension inside the head, persistent dizziness with nausea. A person’s ability to work decreases, and he develops anxiety-phobic conditions. At the same time, taking standard analgesics does not improve well-being.
With persistent hypertensive-hydrocephalic syndrome, people develop paresis/paralysis, as well as serious difficulties with speech, vision, hearing, and decreased intellectual capabilities.
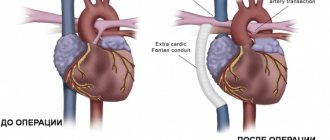
Aortic dilatation
The aorta is the largest vessel in the body, which receives oxygen-rich blood from the left ventricle.
A dangerous condition is enlargement (dilatation) or aneurysm of the aorta. Typically, the aorta dilates at a “weak spot.” One of the reasons for this condition is arterial hypertension. Atherosclerosis and inflammation of the aortic wall can also lead to pathology.
The danger of an aneurysm is:
- In sudden rupture of the aorta. This results in severe internal bleeding, which is life-threatening.
- In the formation of blood clots. This condition is also extremely life-threatening.
More often, an aortic aneurysm is discovered during examination by chance. But still, some signs are sometimes present:
- Unreasonable sore throat and cough.
- Hoarseness of voice.
- Difficulty swallowing due to compression of the esophagus.
- When the aorta ruptures, there is severe chest pain that spreads to the neck and arms. The prognosis in this case is unfavorable - the person quickly goes into shock due to large blood loss and dies.
Aortic dilatation does not develop immediately. This is a long process, as a result of which the vessel wall undergoes gradual changes. Timely detection of pathology can prevent the terrible consequences of the disease.
In addition to the aorta, smaller vessels also undergo expansion. This occurs due to abnormally increased blood volume, exposure to hormones or chemicals. Vascular dilatation leads to circulatory disorders, which affects the functioning of all body systems.
Diagnostics
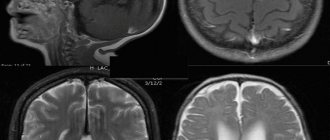
If a specialist observes signs of a malfunction in the circulation of cerebrospinal fluid through the cerebral ventricles, or the patient has complaints of deterioration in health, then instrumental confirmation of dilatation of the brain cavities is required.
It is possible to identify signs of slight dilation of the lateral ventricles using such a modern diagnostic examination method as magnetic resonance imaging. On the resulting images of brain structures, you can see in detail the area of expansion, the area of damage, and the involvement of neighboring brain tissues in the process.
Increased intracranial pressure will also be diagnosed using the following procedures:
- echoencephaloscopy;
- electroencephalography;
- ophthalmoscopy;
- examination of cerebrospinal fluid - identification of previous neuroinfections;
- blood tests - general, biochemical, for autoimmune processes.
Only after careful comparison of all information from diagnostic procedures, a neurologist will be able to assess the severity of dilatation of the lateral ventricles, establish the root cause of the pathological condition and select optimal therapeutic measures.
How is the presence of dilatation determined?
Minor dilatation is, as a rule, an asymptomatic pathology. In this case, patients do not present any complaints that could lead one to suspect the presence of enlargement. But if, as a result of this pathological process, the pumping function of the heart decreases, then the patient may show signs of heart failure: weakness, fatigue, shortness of breath, swelling of the extremities, etc.
Signs of dilatation can be determined by the results of an ECG, but it is impossible to accurately identify it only with the help of this examination. The main method for this is ultrasound of the heart. It helps to detect a previous heart attack or heart defects, and this, in turn, indicates the presence of enlargement. Using ultrasound, the diameter of the ventricle is also measured (in other words, its end-diastolic size - EDS).
However, it should be taken into account that the GDR is not an absolute indicator. With an average norm of 56 mm, it can vary depending on the height, weight and physical fitness of a particular person. If for a two-meter athlete weighing more than 100 kg the norm may be 58 mm, then for a woman weighing 45 kg and reaching a height of only 155 cm, this figure is already a sign of dilatation.
- Features of left atrium dilatation, types of pathology
Treatment tactics
In itself, the expansion of the size of the ventricles of the brain does not require intervention - if there are no clinical signs of intracranial pressure failure. Whereas in the case of a violation of liquorodynamics and symptoms of deterioration of well-being formed against this background, doctors will recommend conservative therapy:
- diuretics – removing swelling from brain tissue;
- neuroprotectors – correction of the conduction of nerve impulses;
- vasoactive agents – improving brain nutrition;
- nootropics – improvement of local blood circulation;
- sedative medications – normalization of the psychosomatic background;
- anti-inflammatory/antibacterial drugs – if the disorder is caused by an infectious process.
Neurosurgical intervention will be required if ventricular dilatation is caused by brain tumors or thromboembolism of cerebral vessels. If necessary, ventriculostomy is performed to create a new connection between the cavities of the brain.
Consequences
The consequences of increased intracranial pressure are manifested in the following symptoms:
- The baby becomes lethargic and loses appetite.
- A pronounced venous network appears on the forehead due to obstruction of outflow from the cranial cavity.
- Muscle tone in the limbs changes, tendon reflexes, which normally should be moderate, are revived.
- Changes occur in the fundus in the form of congestion.
- Sometimes tremor appears in the limbs.
- Both grasping and swallowing and sucking reflexes are reduced.
- The baby spits up often. This is caused by the fact that increased cerebrospinal fluid pressure irritates the vomiting centers at the bottom of the rhomboid fossa (in the fourth ventricle). The adult equivalent is cerebral vomiting without nausea.
- Tension and bulging of the fontanelles appear, and an increase in their linear dimensions occurs.
- The baby has a disproportionately large head.
Of course, the symptoms described above are not necessarily associated with ventriculomegaly. As mentioned above, a slight increase in size, and even asymmetry of structures, in the absence of a clinical picture, changes in reflexes and the fundus of the eye, should not bother parents. They should simply observe the baby and do neurosonography on him regularly.
Prognosis and prevention
The consequences of asymmetry of the lateral ventricles are varied. Their severity and severity directly depend on the size of the pathological expansion and the age of the patient. Thus, in mild forms of the disorder, children experience short-term developmental delays, both intellectual and physical. With timely medical care, hydrocephalus is completely eliminated.
Whereas with severe dilatation of the cavities, various neurological diseases are formed - for example, cerebral palsy, or persistent mental disorders. There is no specific prevention of ventricular asymmetry, since it is almost impossible to predict its occurrence. However, experts point out that when the expectant mother strives for a healthy image, she contributes to the birth of a baby with normal sizes of brain cavities. To do this, you need to give up bad individual habits even before pregnancy, eat right, get good sleep, and avoid psycho-emotional and stress overload.
MORPHOLOGY OF TUMORS OF THE III VENTRICLE
The morphology of tumors of the third ventricle is different. In the anterior parts of the ventricle, colloid cysts are more often observed, which are classified as dysembryogenetic neoplasms. Previously it was believed that they are derivatives of the neuroectoderm (paraphysis - an embryonic structure that is a pocket between the telencephalon and the anterior parts of the midbrain), but more data indicate their endodermal origin. They have an epithelial lining and characteristic mucous contents and are more common in adults. Macroscopically, colloid cysts are round or oval-shaped formations, the diameter of which ranges from 0.3 to 4 cm. The cyst has a dense capsule with a smooth wall and viscous contents of a greenish-gray color. Recently, their endodermal origin has been established.
Ependymomas arise from the inner lining of the ventricles of the brain and account for 5–10% of all tumors of the central nervous system. Of these, 2/3 arise in the posterior cranial fossa, 10% in the spinal canal and the rest supratentorially in the lateral and third ventricles. Within the third ventricle, ependymal tumors are predominantly localized in its posterior sections; macroscopically they have the appearance of a node with a predominant localization in the ventricular cavity. They are well demarcated from the brain, but in some areas they grow into the medulla. The depth of germination depends on the malignancy. Ependymomas have well-visualized borders, and therefore their complete removal is possible. Implantation metastases of malignant ependymomas are rare. According to RI Ernestus (1996), in children the frequency of ependymomas is 18.6%, less than astrocytomas and medulloblastomas (sex ratio 6:5 with a predominance of men).
In the pineal region there are: germ cell tumors - germinoma, teratoma (or epidermoid, dermoid), teratoma with malignant transformation, embryonal carcinoma, endodermal sinus tumor, choroid carcinoma and mixed germ cell tumors; tumors from the pineal parenchyma - pinealoma, pineocytoma, pineoblastoma; gliomas and tumors from the velum interpositum - meningiomas, hemangiopericytomas, angiomas, cysts, less often - pineocytomas.
Pinealomas and germinomas, according to the same author, could be located in the suprasellar-hypothalamic region and in other sections. Pineoblastomas have an invasive growth pattern, often metastasize and are close to medulloblastomas in their histological structure and degree of malignancy. Pinealocytomas are well-circumscribed benign tumors that often have a capsule and cysts. Choroid carcinomas and yolk sac tumors look like large infiltrating formations that early disseminate along the spinal canal and in 10% of cases metastasize beyond the central nervous system (to bones, lungs, lymph nodes).
Meningioma is a very rare neoplasm of this area, especially in childhood. Their frequency is 1.5 – 2.5%.
Craniopharyngiomas localized in this area are often cystic, located in the cavity of the third ventricle, penetrate into the lateral ventricles, extraventricularly and often reach gigantic sizes. In the world literature, there is one report on the diagnosis of craniopharyngioma of the pineal region, accidentally discovered at autopsy in a 58-year-old woman who died in a fire, and a second observation in our clinic. Germinomas originate from embryonic cells, 20% of them are located in the suprasellar region, involve the floor and walls of the third ventricle, and may primarily originate from the basal ganglia. Germinomas can metastasize to the walls of the ventricles and basal cisterns.
According to the histological structure of the tumor of the bottom of the third ventricle, almost all are astrocytomas, most often low-grade juvenile pilocytic and sometimes fibrillary astrocytomas. Our data support this statement. Astrocytomas of this localization are benign neuroectodermal tumors, the histological structure of which does not change in most cases over many years of growth before and after surgical interventions. Macroscopically, astrocytomas in most cases are poorly demarcated from the surrounding tissue and are homogeneous. Pilocytic astrocytomas have the appearance of a grayish nodule. The boundaries of the tumor are quite clear, and cysts are often found. Pilocytic astrocytomas have many papillae, and tumors with severe angiomatosis are sometimes found.
Hypothalamic hamartomas are rightfully classified as developmental defects, located between the pituitary infundibulum and the mamillary bodies, and histologically consist of tissue similar to the hypothalamus. There are hormonally active and hormonally inactive forms.
Choroid papillomas make up less than 1% (0.65% according to our data) of all intracranial tumors, and only less than 10% of them are localized in the third ventricle. Most often, these tumors arise as functioning intraventricular papillomas of the roof of the third ventricle, secreting cerebrospinal fluid. Tumors of the choroid plexus have a fairly slow growth rate and reach a large size. Macroscopically, they have the appearance of a node with a finely granular lobulated surface (cauliflower-like appearance), dark red in color, dense consistency, with a predominant localization in the lumen of the ventricle. Choroid plexus carcinoma is a more aggressive tumor, accounting for 10–20% of all choroid plexus tumors. It is rightly believed that choroid carcinomas can invade the medulla over a large area. This tumor is characterized by features characteristic of anaplastic tumors and has a tendency to diffuse extracranial spread. Although choroid plexus papillomas can spread beyond the skull, their deposits are benign and, as a rule, asymptomatic. Choroid carcinomas tend to form implantation metastases, which usually become clinically apparent during the first months after surgery.
There are reports in the literature of 23 cavernous malformations of the third ventricle.
Hemangioblastomas, metastatic medulloblastomas, glioblastomas, and epidermoid cysts can also be found in the third ventricle.