Dilatation is a persistent diffuse expansion of the lumen of a hollow organ. The reasons for this condition are different, for example, the heart can become enlarged due to heavy physical activity, then the reason will be natural. But if this happens due to any disease, then the nature of the cause will be pathological.
Do not self-medicate. At the first signs of illness, consult a doctor.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Possible complications
- Prevention
As mentioned earlier, this can happen to any hollow internal organ of the body. But most often the concept of dilatation is applied to pathologies of the heart cavities.
Depending on where exactly the expansion occurred, cardiac dilatation can be divided into:
- dilatation of the left atrium;
- dilatation of the left ventricle;
- dilatation of the right atrium;
- dilatation of the right ventricle.
Typically, one chamber of the heart dilates; in rare cases, this can happen to the atria or ventricles. This condition can lead to arrhythmia, heart failure, thromboembolism or other diseases. Aortic dilatation is a direct symptom of connective tissue dysplasia.
Reasons causing dilatation
Sometimes dilatation of the left ventricle is caused by previous inflammation of the heart - viral myocarditis. Often the cause of lumen expansion is coronary heart disease or hypertension.
Ventricular dilatation may appear in a patient in the post-infarction period, caused first by stretching of the infarction area itself (due to the divergence of muscle fibers), and then by neighboring areas. The reason for this is the weakening of the wall of the left ventricle and its loss of elasticity, which provokes excessive stretching.
Treatment
Treatment is aimed at getting rid of or correcting the primary pathology that caused the expansion. Therefore, the prescribed therapy will be aimed at eliminating the root cause.
The doctor may prescribe drugs with the following spectrum of action:
- antibiotics;
- glucocorticosteroids;
- drugs against coronary disease;
- drugs that reduce heart rate;
- beta blockers;
- blood pressure lowering agents;
- blood thinning medications;
- diuretics.
If the prescribed treatment does not help, it is necessary to undergo surgery, during which a pacemaker will be installed.
In general, if treatment is started correctly and in a timely manner, the risk of developing any complications can be significantly reduced, but in this case it is impossible to completely eliminate them.
There is not and cannot be an unambiguous prognosis, since everything will depend on the nature of the course of the clinical picture, the severity of the pathology, as well as the general health indicators of the patient.
How is the presence of dilatation determined?
Minor dilatation is, as a rule, an asymptomatic pathology. In this case, patients do not present any complaints that could lead one to suspect the presence of enlargement. But if, as a result of this pathological process, the pumping function of the heart decreases, then the patient may show signs of heart failure: weakness, fatigue, shortness of breath, swelling of the extremities, etc.
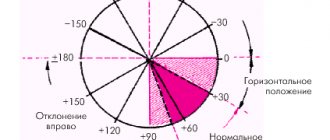
Signs of dilatation can be determined by the results of an ECG, but it is impossible to accurately identify it only with the help of this examination. The main method for this is ultrasound of the heart. It helps to detect a previous heart attack or heart defects, and this, in turn, indicates the presence of enlargement. Using ultrasound, the diameter of the ventricle is also measured (in other words, its end-diastolic size - EDS).
However, it should be taken into account that the GDR is not an absolute indicator. With an average norm of 56 mm, it can vary depending on the height, weight and physical fitness of a particular person. If for a two-meter athlete weighing more than 100 kg the norm may be 58 mm, then for a woman weighing 45 kg and reaching a height of only 155 cm, this figure is already a sign of dilatation.
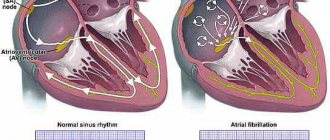
In patients with AF, the main, and sometimes the only finding is pathology of the atria of the heart.
Hypertrophy (thickening of the fibers) and dilatation (expansion of the cavity) of the atria can be both a cause and a consequence of AF, and can occur due to any heart disease. It is assumed that two main mechanisms are involved in the development of AF, which can coexist separately and simultaneously:
1. The presence of one or more focuses with fast impulses. (Focus is a region of the myocardium that can initiate arrhythmia.) Foci are most often located in the area of the superior pulmonary veins flowing into the left atrium. Foci are also found in the area of the muscular couplings of the pulmonary veins, in the right atrium and rarely in the superior vena cava or coronary sinus, as well as in the Marshall ligament. Dilatation (expansion) of the pulmonary veins is one of the important anatomical factors in the occurrence of AF.
2. The presence of one or many small waves (loops) of excitation of the re-entry type (re-entry is re-entry of excitation). Unlike other arrhythmias, which typically involve a single re-entry loop, multiple loops may be involved in the underlying cause of AF because the dissipation of the wave front as it travels through the atria results in the generation of self-sustaining “daughter waves.”
Electrical remodeling of the atria. If the duration of AF is less than 24 hours, then restoration of sinus rhythm is usually completed successfully, while a longer duration of AF reduces the likelihood of restoration and maintenance of sinus rhythm. These observations gave rise to the popular expression “atrial fibrillation begets atrial fibrillation.” The increased susceptibility to AF is associated with a gradual shortening of the effective refractory period as the duration of the attack increases. This phenomenon is called “electrical remodeling.”
Atrioventricular conduction. The atrioventricular node limits impulse conduction in AF (in the absence of an additional pathway). The frequency of ventricular contractions in AF depends on the properties of the node, as well as the drugs acting on it and the activity of the sympathetic and parasympathetic nervous system.
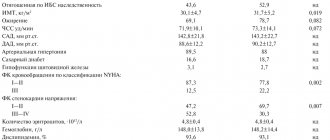
Clinical conditions predisposing to AF
AF is associated with a variety of cardiovascular conditions that can maintain the arrhythmia.
Arterial hypertension is the most common underlying condition in patients with AF; is found in approximately 2/3 of all patients with AF according to various examinations. Insufficient blood pressure control is a risk factor for the occurrence (first detection) of AF in patients with hypertension and a risk factor for complications of AF: stroke and systemic thromboembolism, even in patients on anticoagulant therapy.
Chronic heart failure, defined as heart failure with dyspnea on exertion (HYHA class II-IV), is detected in 30% of patients with AF. In turn, AF is found in 5-50% of patients with HF. The prevalence of AF increases with the clinical progression of CHF: in patients with NYHA class IV CHF, AF is detected in almost 50% of cases.
Valvular pathology of the heart, especially mitral valve defects (stenosis and insufficiency), which cause overload of the left atrium with pressure or volume and, thus, provoke AF.
Cardiomyopathies (hypertrophic, dilated, right ventricular), including primary electrical heart diseases (long QT syndrome, short QT syndrome, Brugada syndrome and catecholaminergic VT), carry a high individual risk of developing AF.
Congenital heart disease (CHD) and atrial septal defect (ASD), according to studies, are associated with AF in 10-15% of patients.
Other congenital heart defects are often associated with AF. Patients with a single ventricle, patients who have undergone atrial repair surgery (Masterda procedure), transposition of the great arteries, or patients who have undergone a Fontan procedure have an increased risk of developing AF. Altered atrial anatomy due to primary abnormalities, surgery, or subsequent hemodynamic abnormalities may be a major predisposing factor in the development of AF. In these patients, AF can be severely symptomatic and often difficult to treat.
IHD is present in 20% of cases among patients with AF. Whether CAD itself predisposes to the occurrence of AF is unknown. But it is necessary to take into account that AF in coronary artery disease can be caused by CHF after a myocardial infarction (MI), arterial hypertension. AF is rare in patients with stable coronary artery disease and preserved LV function, but its presence indicates a poor prognosis after MI.
Thyroid dysfunction is an important cause of AF. Studies have shown the relationship between AF, both with hypo- and hyperfunction of the thyroid gland, and with subclinical hyperthyroidism. Free T4 concentration was independently associated with AF.
Obesity is detected in 25% of patients with AF. A meta-analysis of population-based cohort studies found that obese individuals had a 49% higher risk of developing AF compared with nonobese individuals. Among other factors, obesity is associated with hypertension, sleep apnea, COPD and diabetes mellitus. Obesity is the most likely marker of cardiovascular risk associated with, among other things, AF.
Many patients with metabolic syndrome develop AF; on the other hand, this association depends on conditions predisposing to AF (arterial hypertension, obesity).
Sleep apnea is associated with increased intraatrial pressure and dilatation and may predispose to the development of AF.
High height is associated with AF. The mechanism of this phenomenon is unclear, but it is assumed that mechanical distension of the pulmonary veins (PV) and dilatation of the left atrium may contribute to the development of arrhythmia.
Diabetes mellitus, as a condition requiring treatment, is found in 20% of patients with AF. Poorly controlled diabetes may potentially promote atrial cell death and “structural remodeling” and thus be responsible for the maintenance of AF.
Chronic obstructive pulmonary disease (COPD) is detected in 10-15% of patients with AF. In some patients, lung disease may be more a marker of cardiovascular risk in general than a specific predisposing factor for AF. Bronchial cancer can also occur with AF.
Chronic renal failure (CRF) is present in 10-15% of patients with AF. ESRD may increase the risk of complications associated with AF, especially cardiovascular complications. ESRD, diabetes mellitus, and COPD are even more common in patients with persistent AF.
Consequences of AF
Hemodynamic consequences of AF. In AF, three factors can affect hemodynamics: lack of atrial synchrony, erratic ventricular response, and excessively high heart rate. Due to deterioration of atrial contractile function, a significant decrease in cardiac output may be observed, especially in patients with decreased ventricular diastolic filling, arterial hypertension, mitral stenosis, hypertrophic or restrictive cardiomyopathy. In addition to affecting atrial function, the persistently accelerated ventricular rate in AF may cause dilated cardiomyopathy (an arrhythmogenic cardiomyopathy caused by tachycardia).
Thromboembolic consequences of AF. Stroke is the most devastating consequence of AF. Approximately every 5-6th stroke occurs due to AF. The main source of disabling ischemic strokes of cardioembolic etiology in patients with AF are considered to be thrombi that form in the left atrial appendage as a result of blood stasis. Up to 25% of strokes associated with AF may be a consequence of pre-existing cerebrovascular disease and may develop due to thromboembolism from other cardiac sources or atherosclerotic plaques of the aorta.
The mechanism of thrombus formation is associated with a decrease in blood flow velocity in the left atrium. In AF, there is no full atrial systole, the left atrial appendage empties passively, as a result of which the speed of blood flow in its cavity decreases. With a decrease in the LV ejection fraction, the blood flow in the left atrial appendage slows down even more, up to complete stasis (stagnation) of the blood, and the size of the left atrium increases, which in turn promotes thrombus formation.
The quality of life. The quality of life of patients with AF is reported to be significantly worse than that of individuals in the same age group without AF. Restoring and maintaining sinus rhythm is associated with improved quality of life and better exercise capacity in some studies, but not all. In typical studies, the majority of patients with paroxysmal AF perceived that the arrhythmia interfered with their lifestyle, but this perception was not associated with either the duration or frequency of attacks accompanied by clinical manifestations.
Revishvili A. Sh. “Clinical cardiology: diagnosis and treatment”, 2011. edited by Bockeria L.A., Golukhova E.Z.
What is mild dilatation of the lateral ventricles?
The human brain also has cavities called ventricles. There, cerebrospinal fluid (CSF) is produced, which is discharged through special channels. As a rule, dilatation of the ventricles is a sign that either fluid is produced in excess, or it does not have time to be eliminated normally, or there are some obstacles in its way.
Normally, the depth of the lateral ventricles of the brain is from 1 to 4 mm. At high rates, causing the disappearance of their lateral curvature, we are talking about dilatation. But it should be borne in mind that this is not a diagnosis, but a symptom of some disease that doctors must identify and eliminate.
Symptoms
Symptoms of cardiac enlargement, if slight, are practically unnoticeable because moderate dilatation shows no signs.
If the expansion of the left atrium is too large, the work of the heart deteriorates and the following symptoms occur:
- dyspnea;
- cardiopalmus;
- heart failure;
- fibrillation;
- thromboembolism.
They cannot be called specific, and they are practically invisible. A doctor can identify such a pathology during a preventive examination.
Is dilatation always dangerous?
Clinical practice shows that dilation is not always a sign of the presence of some significant pathology. It most often occurs in premature babies, due to the fact that the size of these ventricles is much larger than in babies born at term, or it is a feature of the structure of the skull of a particular child.
But nevertheless, the presence of diagnosed dilatation of the lateral ventricles of the brain requires monitoring the dynamics of the baby’s growth and development. If no abnormalities are detected during the control period, then the baby is considered healthy.
Do not be ill!
Diagnostics
To detect heart enlargement, the doctor prescribes the following diagnostic methods:
- Echocardiography. This ultrasound examination will help establish the correct diagnosis. In addition, it will be possible to identify the cause of this condition, for example, myocardial infarction, valve insufficiency and much more.
- Electrocardiography. Prescribed if necessary as an additional diagnosis.
- Scintigraphy. It is prescribed for differential diagnosis, in which it is possible to distinguish organ enlargement from ischemic disease.
- X-ray.
Cardiac scintigraphy
If the results show that the chambers have expanded by more than 5%, then the doctor will make an appropriate diagnosis.
Prevention
Preventive measures are part of the treatment of this condition: without them there will be no positive result.
In this regard, the following rules should be adhered to:
- balance your diet, which will contain only plant foods, lean meat and fish, seafood, dairy products, nuts and grains;
- spend more time outdoors;
- doing physical exercise;
- stop smoking and drinking alcohol.
All this will help improve blood circulation, strengthen myocardial muscles, increase immunity, and then life expectancy will increase.
Symptoms
The manifestation of clinical signs is heterogeneous. The nature of the clinic will depend on which areas are enlarged.
Typically this is:
- chest discomfort or pain;
- dyspnea;
- loss of strength, fatigue;
- cardiomyopathy;
- rhythm disturbance;
- peripheral edema.
Other symptoms will depend on the underlying cause that causes the dilatation.
The appearance of shortness of breath is one of the first signs of the disease