The first signs of the development of varicose veins are often attributed to ordinary fatigue, a trip to the doctor is ignored, and they continue to lead their usual lifestyle, aggravating the condition of the veins. Complications with varicose veins develop very quickly. Mostly those who require surgical intervention come to the specialist. Until this moment, everyone is trying to cure themselves with the help of tinctures and tablets.
How not to bring yourself to a deplorable state and take the necessary measures in time? First, you need to understand when you need to see a doctor. Secondly, go to the doctor as soon as you realize it’s time. This is not a case where you should wait a little and see what happens to the veins. Any delay can cost you dearly. The article contains descriptions of the signs of different types of varicose veins, which will help determine whether you suspect the disease.
How are the veins in the legs arranged?
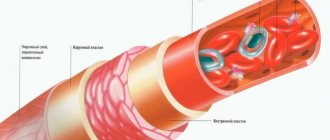
The legs have two groups of venous vessels: superficial and deep or deep. The first are located in the subcutaneous tissue, that is, on the surface of the leg. The latter are located deeper, in the thickness of the muscles, next to the arteries and tendons. The deep and superficial vessels are connected by perforating or perforating veins. Their wall consists of collagen and elastin fibers, with weak and few smooth muscles. The venous wall has a three-layer structure:
- At the top is the adventitia, which is composed of loose connective fibers, smooth muscle cells elongated along the walls, surrounded by small capillaries and nerves responsible for the trophism of the vessel.
- In the middle is the media, consisting of circular smooth muscle fibers.
- The intima is located on the inside. The basis of the intima is the endothelium; between its cells there are longitudinal fibers of smooth muscles. The inner shell is folded, the thickenings are opposite each other and resemble swallows' nests or patch pockets. They are called valves and are responsible for the correct direction of blood flow.
Venous valves direct blood from the peripheral parts to the heart, as well as from the superficial to the deep veins. They prevent reverse outflow and increase venous pressure. In addition to the valves, smooth muscles, tendons and muscles of the leg take part in maintaining normal tone. When any of the layers (usually the median and internal layers) are damaged, the veins lose their tone and expand, and varicose veins occur.
- There are several superficial veins:
- The great saphenous vein is located on the inside of the leg; its walls are equipped with several valves; blood from the anterior femoral surface is collected into this vein through a series of smaller vessels.
- The small saphenous vein is located on the outside of the leg, equipped with valves, and collects blood from the veins on the front and back of the leg.
Communication between the large and small veins occurs through connecting vessels.
- The deep veins are the posterior and anterior tibial veins, the popliteal vein, and the femoral vein. Varicose veins develop in them at advanced stages, when the disease is not treated for a long time.
How to determine the appearance of varicocele
Varicocele is a purely male type of varicose veins, which is an expansion of the veins of the spermatic cord. Signs of varicocele include nagging pain and a feeling of heaviness in the groin area, shrinkage of one of the testicles, enlarged veins under the skin, and frequent urination.
Why does pathology occur:
- the valves of the spermatic cord veins do not work well;
- there is not enough connective tissue forming the venous wall;
- the valves of the spermatic cord and testicles are underdeveloped;
- disruptions in the process of formation of the inferior genital vein in the womb.
If a man has high abdominal pressure, often experiences constipation, spends a lot of time sitting or standing, or exposes his body to excessive physical activity, then the risk of varicocele increases significantly. This disease has three degrees of severity: at first the veins can only be palpated in a standing position, at the second stage the lumps can be palpated while lying down, and at the third stage the swollen veins of the spermatic cord on the testicle are visible to the naked eye.
The stage when the testicles are covered with numerous clusters of veins is considered final and requires emergency treatment. After all, neglected varicocele very often becomes the cause of male infertility, thrombosis, thrombophlebitis and other complications. Pathology is diagnosed using an external examination, ultrasound, MRI or CT. Adult patients are often prescribed a spermogram to determine sperm activity and exclude asthenozoospermia.
For what reasons does varicose veins appear, and who is at risk of getting sick?
It is difficult to say why people get varicose veins at the moment. Only a number of risk factors have been identified, due to which the valves weaken and the elasticity and tone of the walls of the superficial and perforating veins decrease.
Here are the factors that lead to the development of the disease:
- Heredity. The structure of the walls of blood vessels is determined genetically; with some changes in the genes, they weaken and the valves do not close well. As a result, with the slightest increase in pressure in the veins, a reverse outflow of blood occurs, the vessels overflow and expand.
- Hormonal changes in the body in women. This situation is typical for pregnant women or for the second half of the cycle, when the amount of progesterone increases and the level of estrogen decreases. As a result, blood rheology changes (coagulability increases), vascular tone decreases, elastin and collagen fibers are destroyed, and the risk of blood clots increases.
- Obesity. People who are overweight move little, which slows down blood flow throughout the body. Excess subcutaneous fat on the abdomen leads to increased pressure in the abdominal cavity and compression of the main veins. This leads to stagnation of blood in the vessels of the legs, and further to varicose veins.
- Diabetes. Sugar, the level of which increases in this disease, damages the vascular endothelium, which increases the risk of blood clots.
- Alcoholism. When drinking large doses of alcohol, dehydration occurs, the blood thickens, clots form, clogging small blood vessels and causing congestion.
- Static occupational loads, such as lifting heavy loads, standing or sitting work. In such a situation, muscle tone drops, blood moves worse from the lower extremities to the heart, stagnation occurs, and the veins in the legs dilate because of this.
- Congenital pathologies of blood clotting. Hypercoagulation, in which too many factors are produced that are responsible for the formation of clots in the blood, provokes thrombosis and impedes the movement of blood through the vessels.
- Wrong diet. A diet deficient in a number of vitamins (C, E, PP) and plant fiber leads to disturbances in the structure of the endothelium and other structural elements of the vascular walls.
- Tight underwear. When wearing tight underwear, some of the veins are pinched, which causes obstructed blood flow from the lower half of the body.
- Frequent constipation. People suffering from this problem have to constantly push, this increases the pressure inside the abdomen, as a result, the outflow of blood becomes difficult.
- High heel. Overstraining the calf muscles and insufficient contraction causes blood to stagnate in the veins.
- Hot climate. In summer, during the heat, the body becomes dehydrated. If you do not compensate for the problem by drinking a sufficient volume of fluid, the risk of blood clots in the vessels will increase.
- Pathologies of the heart and kidneys. These may be congenital or acquired heart defects, renal failure.
- Exceeding doses of medications that affect coagulation. In this case, the blood vessels may become clogged with blood clots.
- Operation. The risk of thrombosis in this case increases due to blood loss and compression of veins during the intervention.
Why do varicose veins appear?
If you know the causes of varicose veins, you can protect yourself in time by taking preventive measures.
Heredity. If one of your relatives suffers from varicose veins, then there is a chance that you will have it too. Varicose veins themselves are not inherited, but you may inherit structural features of the veins or, for example, a tendency to be overweight, which will affect the occurrence of problems with the veins.
Pregnancy. During pregnancy, a woman's body produces an increased amount of progesterone, which relaxes the walls of the veins. They can't do their job and the blood stagnates. Also during pregnancy, a woman’s body weight increases and the amount of circulating blood increases, which increases the load on the veins.
Overweight. Large body weight creates a constant load on the lower limbs. It is more difficult for the veins to supply blood to the heart and lungs, the blood stagnates, and the veins dilate. As a result, venous expansion of the veins occurs.
Wearing uncomfortable clothes and shoes. If the shoes are too narrow and tight, it prevents blood from circulating normally in the legs. The same goes for clothes that are too tight.
Elderly age. Age-related negative changes occur in the walls of blood vessels. They lose their elasticity, the vessels stretch and blood accumulates and stagnates in them.
How can varicose veins be complicated?
- Thrombosis due to blood stagnation.
- Vascular thromboembolism as a result of blood clot detachment.
- Thrombophlebitis or inflammation of the venous wall.
- PE (pulmonary embolism). In this case, blood flow in the pulmonary circulation is sharply disrupted, which leads to death. Small blood clots can lodge in the small pulmonary arteries and cause a heart attack or pulmonary edema.
- Trophic ulcers, eczema on the skin of the legs due to tissue malnutrition. With poor blood circulation, little oxygen and nutrients enter the tissues, which impairs regeneration or causes massive cell necrosis.
- Edema syndrome. As a result of impaired blood outflow and stagnation, fluid leaks through the walls of blood vessels into the intercellular space. The swelling is soft in consistency, elastic, and most often appears near the affected vein, regardless of the time of day.
- Dermatitis. The inflammatory process in the skin develops due to impaired blood flow and tissue nutrition.
- Hyperpigmentation, cyanosis of the affected areas of the skin.
- Consolidation of subcutaneous fat due to swelling and hemorrhage.
What are internal varicose veins
With internal varicose veins, it is not the superficial, but the deep veins that are affected. The usual external signs in the form of bulging veins and vascular networks are often absent. The pathology is manifested by soreness of the lower extremities, which is often mistaken for banal fatigue. Elderly people are susceptible to internal varicose veins, whose deep veins transform due to age-related changes, become less flexible and elastic, and the valve system suffers from wear and tear. If the pathology is not treated, ulcers form on the lower extremities, which are difficult to heal.
How to diagnose varicose veins
- Using functional tests (application of a tourniquet), the condition of the valves is studied. They are named after the authors - Troyanov-Trendelenburg, Pratt, Sheinis, Delbe-Perthes, etc.. For the Troyanov-Trendelenburg test, you need to lay the patient horizontally, then offer to raise the leg 450. In this position, the doctor strokes the limb from the foot upward to empty the superficial veins. The next step is to apply a tourniquet to the upper half of the thigh, after which the patient rises from the couch. Healthy veins in the legs should fill up after 15 seconds.
- Duplex ultrasound scanning of veins (ultrasound angioscanning) provides the most information and allows you to visualize the vessels and blood flow through them.
- Dopplerography is a method for assessing blood circulation through vessels.
- Phlebography or X-ray examination using contrast, which helps to study the internal structure of the vessel.
- Phleboscintigraphy is a technique using radioactive substances with further study on a special device for their distribution.
To study the superficial veins, they are examined and palpated. The first three methods are used as additional examinations. The last two methods are necessary to study the condition of the deep or deep veins.
Diagnostics
Diagnosis of varicose veins, the symptoms of which are described above, poses the following tasks:
- Determining the presence of pathology in each individual patient. It often happens that people who do not have varicose veins are confident in their presence, and vice versa. However, only an experienced phlebologist, based on an external examination and a series of comprehensive studies, can make an accurate diagnosis.
- Establishing the type characteristic of venous pathology. The doctor determines exactly which veins have undergone pathological damage, and also establishes the extent of this damage and possible or already occurring consequences.
- Prescribing the correct course of treatment. Based on the diagnosis and the characteristics of each specific organism, the attending physician makes a choice in favor of one or another treatment or a set of therapeutic measures.
- Assessment of the level of effectiveness of therapy, which is carried out by the attending physician during the elimination of the disease or after the patient’s complete recovery.
The main methods for diagnosing VV include:
- Plethysmography.
- Thermography.
- Magnetic resonance imaging.
- Ultrasound angioscanning.
- Computed tomography.
- Clinical studies: conversation with the patient, his external examination and manual examination.
- Radionuclide phlebography.
- Intravascular ultrasound.
- X-ray phlebography.
Most often, it is enough for a professional specialist to conduct a clinical examination and ultrasound angiography in order to diagnose varicose veins in the legs. At the Yuzhny clinic, you can undergo a full examination in order to make an accurate diagnosis by an experienced phlebologist. Our specialists work closely with clients, clearly explaining to each of them the specifics of the disease and possible ways to combat it.
Treatment of varicose veins
Conservative treatment options
- Drug therapy does not cure varicose veins, but with the help of drugs, valve function, vascular trophism, blood circulation are partially improved, and the risk of thrombosis is reduced.
For this purpose, venotonics are used (Detralex, Troxivazin, Lyoton gel, etc.). They can be prescribed for any type of varicose veins. Ointments with nonsteroidal anti-inflammatory drugs (Indomethacin, Diclofenac, etc.) are indicated for thrombophlebitis. Also in this situation, anticoagulants are used (Heparin, Clexane, Fraxiparine, etc.), which effectively resolve blood clots. Treatment should be selected by a doctor, after a thorough diagnosis and taking into account the characteristics of the patient. - Herbal medicine and additional techniques are of auxiliary value. It is advised to wear compression stockings, do gymnastics, skiing, cycling, and swimming. The “bicycle” exercise in a supine position, flexion and extension of the feet, gives good results; it improves the outflow of blood from the extremities. You can do the exercises if there are no complications. It is also recommended to take a contrast shower in the morning (water your leg first with warm water, then gradually reduce the temperature to cold). Cool baths with decoctions of oak bark, horse chestnut, chamomile, St. John's wort, rubbing the skin with tincture of white acacia flowers, Kalanchoe leaves, and apple cider vinegar help. Leeches help get rid of thrombophlebitis.
- Mode. You need to get out of bed slowly, 5-10 minutes. Your legs should be raised 10-15⁰ at night; to do this, place a cushion under your heels. You need to walk calmly, it is undesirable to cross your legs when sitting, and do not overwork. All patients are advised to wear compression stockings.
- You need to eat right, include coarse fiber and foods rich in vitamins in your menu. Citrus fruits, tomatoes, rose hips, black currants, nuts, legumes, liver, onions, eggs, and seafood will be useful. It is important not to drink alcohol, not to smoke, and to drink enough water during the day. For persistent constipation, it is recommended to drink a laxative.
Surgery
Phlebectomy or complete removal of veins
The indication for such a radical operation is varicose veins, which involve a large number of veins. At the same time, there are complications - trophic ulcers that are difficult to treat, thrombophlebitis, persistent swelling in the legs, general symptoms (fatigue, dizziness, fainting).
The operation is contraindicated in case of ischemic heart disease, severe infections, in very old patients, in the second half of pregnancy, in case of local inflammation of the legs (erysipelas, pustular rashes, eczema). Only surgery can radically rid the patient of varicose veins and restore the function of the valves. If the situation is too severe, untreated and neglected, this method of treatment remains the only one. The disadvantages of the intervention are the need to give anesthesia and keep the patient in the hospital for several days under observation, postoperative trauma with scars.
Laser therapy (endovascular microthermocoagulation)
Laser treatment of varicose veins is used if the pathology is combined with diseases of the cardiovascular system (CHI, hypertension), changes in peripheral vessels (phlebitis, thrombophlebitis), diseases of the respiratory system (asthma, chronic bronchitis, pleurisy), gastrointestinal pathologies (cholecystitis, ulcers, peritonitis ), nervous system (FM injuries, meningitis, encephalitis and their consequences), genitourinary system (inflammation of the kidneys, prostate, pathology of the uterus with appendages), with skin diseases (furunculosis, dermatitis, psoriasis, etc.).
Contraindications to the use of laser are oncology, decompensated pathology of the kidneys, liver, heart, cerebral sclerosis, pregnancy.
The main advantages of laser therapy are its effectiveness in eliminating dilation of superficial veins, speed (duration of manipulation is 15-20 minutes), no need to go to the hospital, and low trauma. Among the disadvantages, it is worth highlighting the poor accessibility of the technique; not all clinics have the appropriate equipment. Treatment is expensive and is of little use for severely affected and deep veins. If the laser is used incorrectly, you can get a thermal burn, and sometimes depigmentation occurs at the sites of exposure.
Radiofrequency coagulation (ablation)
The operation is indicated for extensive lesions of the saphenous veins, trophic ulcers resulting from long-term and untreated varicose veins.
Radiofrequency coagulation is contraindicated in acute thrombophlebitis, limited mobility of the patient, pregnancy, and mental disorders.
The main advantages of the method are its painlessness, absence of injury, and the need for hospital stay. Patients can return to normal activities the very next day.
The disadvantage is the high cost of the intervention.
Sclerotherapy
Indicated for varicose veins of small and large superficial veins (on large vessels it is carried out under the control of duplex Doppler ultrasound) in the initial stage and without complications. Pregnant and nursing mothers, allergies to drugs, deep vein thrombosis, infectious and inflammatory skin lesions on the legs are not treated with this method. The main advantages are low price, quick recovery, no need for hospitalization. The procedure leaves no marks and does not cause injury.
The disadvantage is the risk of the sclerosing drug entering a deep vein, reduced effectiveness upon contact with blood, and the ability to use only in the initial stages.
Classification and stages
Like any disease, VV has several stages, differing from each other in the degree of spread of the pathology and symptoms. Among them, the following stages are distinguished:
- Initial (or compensation).
- Second (or subcompensation).
- Third (or decompensation).
A detailed description of each stage can be found here.
It is worth noting that complications can occur at any of the above stages, but their greatest likelihood is inherent in the last two. VV can serve as an impetus for the development of diseases such as:
- Thrombophlebitis.
- Erysipelas.
- Deep vein thrombosis.
- Trophic eczema.
A visit to a specialist, made at the first signs of the disease, will help reduce the risks of worsening the situation and begin removing varicose veins. You should not ignore even minor symptoms, because this can lead to undesirable and extremely negative consequences.
Is it possible to cure varicose veins at home?
At home, it is allowed to use auxiliary methods for treating varicose veins, which alleviate symptoms. They use ointments from pharmacies or self-prepared ones, baths and lotions based on herbs, compresses, drink decoctions and infusions to improve blood flow and relieve swelling. Below are some recipes.
Chestnut tincture
Take about 200 g of ripened and peeled chestnuts. Pass through a meat grinder or grind with a blender. Fill everything with a liter of vodka, put it in a dark corner and leave for a couple of weeks. To make the product smell good, add a couple of drops of peppermint oil. In the evening, lubricate the legs with the tincture to get rid of heaviness and itching, strengthen blood vessels, and prevent their fragility. It is also recommended to make a compress from the tincture. If there is no chestnut, it is replaced with nutmeg, the recipe remains the same. Tincture with musk nuts can not only be used to rub sore feet; it is recommended to drink 20 drops a day. After the bottle is finished, a new tincture is made. But there should be a pause of 2 weeks between taking the next portion.
Calendula-based ointment
An infusion is made from calendula flowers - pour a tablespoon of boiling water, put on fire, cook for a couple of minutes, leave for 3 hours in a thermos. Strain the infusion and add it to some kind of fat; lanolin, Vaseline, badger fat are suitable. For the smell, it is recommended to add a drop of aromatic oil (rose, bergamot, citrus, sage, lavender, etc.) Rub the ointment in the morning and evening, with gentle movements from the bottom of the leg to the knee, until completely absorbed. Thyme, hop cones, and nettle are also added to the calendula infusion.
Chamomile oil
Medicinal chamomile flowers are placed in a half-liter glass jar of a dark shade so that the container is filled to the top. Pour in half a liter of any type of vegetable oil, for example, from olives, corn, hemp. Leave for a month, shaking or stirring from time to time. After this, the oil infusion is filtered. For scent, add a couple drops of tea tree, mint, lavender, and grapefruit aroma oil. Apply chamomile oil to the foot early in the morning and late in the evening, while simultaneously doing a light massage. You can also make night compresses from the infusion.
Compress based on wormwood
Take a package of kefir or fermented baked milk, 3 tablespoons of dried wormwood. The grass is crushed and mixed with kefir (ryazhenka). When the grass is wet, place it on cheesecloth along with a thick liquid. Then a compress is applied to the leg, covered with wax paper on top (cellophane film is not used), and everything is fixed with several layers of bandage. Keep your legs elevated and remove the compress after half an hour. It is recommended to do the procedure twice a day. Instead of wormwood, you can take hops, chamomile flowers, string, clover, oak or birch leaves, St. John's wort, horsetail, tricolor violet flowers, yarrow. Combinations of different plants give a good effect. To improve the effect of the compress after the procedure, it is recommended to lie down for a while with your legs raised up. All of the herbs listed can be infused and used to make a foot bath. The water in such a bath should be warm, the duration of the procedure is about 25 minutes. It relieves fatigue, swelling, reduces skin itching and pain.
Traditional recipes for internal use
Various herbal infusions improve blood flow in the veins well. The following herbs are used:
- Clover
- in succession
- Leaves and berries of lingonberries, viburnum, strawberries, raspberries
- Coltsfoot
- Calendula
- Japanese Sophora
- Melissa
- Schisandra
- Hawthorn
The grass is dried, then crushed and made into a mixture of different types of plants. Then take 3 tablespoons, pour a liter of boiling water, leave overnight in a thermos and drink 1/3 glass before meals.
Varicose veins are well treated with bee pollen and honey. Pollen should be consumed internally. Honey can also be eaten, but it still makes good compresses. It is recommended to add infusions of various herbs to honey.
Varicose veins of the lower extremities - diagnosis
To accurately diagnose the disease, you must consult a doctor. Vascular surgery deals with varicose veins of the lower extremities. To make a diagnosis, in addition to complaints and visual examination, it is necessary to use special research methods.
Ultrasound diagnosis of varicose veins of the lower extremities
Duplex angioscanning is considered the gold standard. This method combines ultrasound and Doppler scanning. Thus, it is possible to see the condition of the vascular wall in real time and assess the speed of blood flow in the venous system of the lower extremities.
Treatment of varicose veins in pregnant women
Carrying a baby is accompanied by a hormonal storm in the female body and overload, which often provokes varicose veins. Treatment during this period is carried out conservatively, with the help of local creams, ointments and gels. The most effective ointments have a decongestant effect and eliminate heaviness in the limbs. Asklesan, Venorutin, Lyoton give good results. Apply them in a thin layer, moving from bottom to top, with soft massage movements. The frequency of manipulations is 1-3 times a day.
Folk remedies also help. It is recommended to prepare baths with herbal decoctions (from chamomile, thyme, hop cones, calendula, wormwood, coltsfoot, oak bark, birch leaves, etc.).
You can fight swelling by applying cabbage leaves or raw grated potatoes to your feet. You need to cover the compress with waxed or regular thick paper, not cellophane, so that the skin can breathe. The procedure is done before bedtime and the lotion is left overnight.
Doctors also prescribe medications for internal use to pregnant women. There are venotonics that do not negatively affect the development of the fetus and the health of the mother. They are most often based on plant extracts. Here are some popular drugs:
- Antistax
- Venoruton
- Troxevasin
- Detralex
- Vasocket
- Phlebodia
- Aescusan
After taking the medications, venous tone increases, the walls become elastic, they don’t stretch as much, lymph flow improves, the liquid part of the blood stops leaking into the intercellular space, and swelling goes away. You cannot take these medications without a doctor's prescription.
Caution - varicose veins of the lower extremities
Treatment with traditional methods (prices for herbs and creams differ), but still do not place too much hope on a green pharmacy.
Excess weight provokes the development of varicose veins
It is important to pay attention to nutrition if you have varicose veins of the lower extremities, treatment with traditional methods, the price of which is pennies. It is necessary to limit the consumption of meat, spicy, salty and smoked foods, increase the amount of vegetables and fruits in the diet and eliminate alcohol and coffee.
An optimal daily routine and therapeutic exercises will help improve blood circulation in the extremities. This will take 10-15 minutes a day.
Simple traditional methods of treatment can complement the complex of measures for the treatment of varicose veins. Rubbing the feet with horse chestnut tincture, apple cider vinegar, butter with garlic and many other remedies have been known since ancient times. They will ease varicose veins of the lower extremities, the cost, photos and results can be viewed on our website on the Internet.
Effective external remedies for the treatment of varicose veins
External remedies are not able to cure varicose veins completely, but they slow down the process and relieve some symptoms. In the initial stages, they can be the main treatment.
| № | Medicine | Mechanism of action | Method of use, effectiveness |
| 1 | Venitan Forte Suitable for use with compression garments. | Relieves inflammation, improves vein tone, reduces the risk of thrombosis, and heals wounds. | Apply to the leg from bottom to top, with gentle massage movements 1 to 3 times a day. If there is a trophic ulcer on the leg, ointment is applied along the edges. Course - 8 weeks. Heaviness in the limbs decreases, swelling and pain disappear. |
| 2 | Gepatrombin Allowed for use together with compression garments. | Activates blood flow, lymph flow, removes toxic metabolic products, improves skin trophism. | The ointment is applied to the area of the affected vein in the form of a strip, about 5 cm long. Then rubbed in lightly, moving from bottom to top. If the vein is inflamed, the ointment is not rubbed in, but applied like a bandage. The treatment reduces swelling, relieves leg fatigue and a feeling of heaviness, eliminates cramps and spasms in the calves, and promotes the healing of skin ulcers. |
| 3 | Troxevasin | Eliminates capillary fragility, reduces the permeability of venous walls, relieves inflammation, and prevents thrombosis. | Rub into the skin through a light massage, without touching areas with wounds and ulcers. After use, swelling, pain, and cramps disappear. The healing of trophic ulcers accelerates. |
| 4 | Essaven gel | Improves blood rheology, reduces blood clotting, has an anti-inflammatory effect, strengthens the walls of blood vessels, and improves tissue trophism. | Apply a couple of times a day to the skin over the affected veins. Swelling becomes less pronounced, heaviness, fatigue of the legs, convulsive contractions of the calf muscles disappear, and ulcers heal. |
| 5 | Lyoton 1000 gel, Lyogel | It improves blood flow in small veins, reduces the likelihood of blood clots, has an analgesic effect, and relieves edema. | A strip of gel, 30-10 cm long, is applied along the affected vein and rubbed in with a gentle movement. Relieves fatigue and heaviness in the legs, cramps in the calves, eliminates swelling. |
| 6 | Fastum-gel | It has analgesic, anti-edematous and anti-inflammatory effects, reduces the permeability of venous walls. | A strip of gel, 3-5 cm long, is applied along the diseased vein. Lubricate the leg 1-2 times a day, the course should last at least 3 weeks. The gel helps eliminate swelling, a feeling of heaviness, and fatigue. |
| 7 | Heparin ointment | A good remedy for the prevention of thrombosis, reduces blood clotting and vascular permeability. | A thin layer is applied to the leg and applied twice a day. Swelling decreases and the risk of blood clots decreases. |
| 8 | Ginkor gel | It has a positive effect on vascular tone, reduces their permeability, and improves tissue trophism. | Apply a small volume of gel to the skin 2-4 times a day for 4 weeks. After use, swelling, pain, seizures, heaviness and a feeling of numbness in the legs disappear. |
Team of Doctors
Internal varicose veins are very difficult to recognize in the initial stages. Therefore, everyone who has a genetic predisposition to this disease is recommended to undergo a preventive ultrasound at least once a year. Since the deep veins are surrounded on all sides by muscles, it is impossible to detect their deformation during visual inspection
Effective creams for the treatment of varicose veins
Creams for the treatment of varicose veins are used only at the very beginning of the development of pathology. The following products have proven effectiveness:
| № | Medicine | Mechanism of action | How to use and how it helps |
| 1 | Cyclo 3 cream | The effect is associated with a decrease in blood clotting and an improvement in its rheological properties. Has an anti-inflammatory effect, normalizes lymph flow and blood flow. | The cream is applied to the leg after sleep and in the evening, while simultaneously doing a massage for 2-3 minutes, moving from the heel to the knee. After use, heaviness, numbness, and cramps in the calves disappear, swelling and pain are significantly reduced. |
| 2 | Girudoven | Strengthens the walls of veins, corrects their permeability, partially dissolves blood clots and prevents their formation. | You can lubricate your feet with cream or gel up to 5 times a day, using a small amount of the drug. Swelling, pain, fatigue and heaviness of the limbs disappear. The skin color is evened out and it becomes elastic. |
| 3 | Venitan cream Suitable for combined use with compression garments. | Eliminates inflammation, prevents thrombus formation, strengthens the vein wall, heals trophic ulcers. | Use from once to three times a day, lubricate the skin with light massaging movements, from the periphery to the center, apply along the edges of the ulcers. The course of therapy is 8 weeks. Leg pain and heaviness disappear, the area of ulcers decreases, and swelling subsides. |
| 4 | Venoruton Suitable for use with compression garments. | Strengthens capillaries, reduces their permeability, has an anti-inflammatory effect, prevents the formation of blood clots, and normalizes blood rheology. | Lubricate the damaged areas on the legs twice a day, while doing a light massage of the limb. The legs do not get so tired when walking, heaviness, swelling, and cramps disappear, and the risk of thrombosis decreases. |
| 5 | Cream-balm based on horse chestnut | Increases the tone of blood vessels, strengthens their walls. | Apply in a lying position 2-3 times a day for 6-8 weeks. The balm relieves heaviness and fatigue from the legs, reduces pain. |
| 6 | Venotonic cream "Doctor Ven". | Improves vascular tone, wall permeability, trophism. | Apply to the leg twice a day, gently massaging. Course – 6-8 weeks. After treatment, the skin becomes elastic, the legs are less tired, do not hurt and do not swell. |
| 7 | Foot cream with cooling effect | Increases tone and reduces the permeability of vascular walls, improves tissue nutrition. | Treatment should last 6-8 weeks, the cream is applied to the skin twice a day, lightly rubbing. After application, the cream pleasantly cools the skin, heaviness, fatigue and pain in the legs disappear. |
FAQ
Very often people are interested not only in the question of how to treat varicose veins. Many patients suffering from this disease are interested in what they can do and what they cannot do, in order not to worsen their health condition and not provoke the emergence of other health problems. Below are frequently asked questions of interest to people with VV.
Is it possible to get vaccinated against coronavirus if you have varicose veins?
The answer to the question of whether coronavirus vaccination is allowed for varicose veins is yes. This pathology is not a limitation for vaccination against COVID-19 in the absence of its exacerbation. If a person does not suffer from acute thrombophlebitis, then this refers to decompensation of varicose veins of the legs, and he is not prohibited from being vaccinated against coronavirus infection.
Is it possible to drink coffee if you have varicose veins?
Caffeine has the ability to increase blood pressure and increase heart rate, which are unfavorable factors for fragile, swollen veins damaged by varicose veins. Coffee has the following effects on blood vessels:
- Increased load on the vein walls.
- Increased blood pressure.
- Short-term venous expansion.
Therefore, with varicose veins, you can drink coffee, but not exceeding the daily norm. Completely giving up your favorite tonic drink will not lead to the restoration of veins affected by pathology, so you should not torture yourself and not drink coffee. You just shouldn't drink more than 1-2 cups a day. It is also recommended to dilute coffee with milk.
Is massage allowed?
Comprehensive treatment of varicose veins at an early stage includes massage. However, it requires proper execution.
For varicose veins, you can only do a light massage of the lower extremities. It is also indicated for patients with uncomplicated forms of varicose veins.
It is advisable to perform a professional manual massage for patients with varicose veins, but it is imperative to take into account all the features of the course of the disease. It is recommended that you consult with a specialist before you begin massaging the area where the veins are affected by varicose veins.
Is it possible to warm your feet?
When the legs are heated, the veins expand, blood circulation increases and the load on the venous walls only increases. This can worsen the already poor condition of varicose veins. This is why it is recommended to limit hot baths for patients with varicose veins. It will be better to reduce the temperature of the water from hot to warm, which will not cause vasodilation and will not lead to a worsening of the person’s condition. You should always remember that consultation with a specialist is necessary regardless of whether we are talking about hot baths or vaccination for varicose veins.
Are running and squatting allowed?
Experts recommend starting jogging at the first signs of developing VV. It is important to ensure that these activities are systematic. During running, the blood is saturated with oxygen. Therefore, it is better to give preference to jogging in the forest or park, where the air is always clean.
However, you should adequately assess your capabilities and endurance, and avoid excessive stress, which is contraindicated for varicose veins. It is important to monitor a gradual increase in loads that do not exceed values that are comfortable for the body.
A person with BB should not feel tired while jogging. Only short-distance running using compression socks is allowed. In case of thrombophlebitis, jogging should be avoided. The admissibility of running and squats with pelvic varicose veins should be discussed with your doctor.
What is the best treatment for varicose veins?
Today there is no clear answer to the question of which therapeutic method is the most effective for varicose veins. The fact is that success in treatment depends on a number of factors that must be assessed by a qualified specialist in each specific case. Only after this can they make a final decision on prescribing one or another treatment for IV.
In order to prevent the situation from worsening, you should stop self-medicating at the first manifestations of the disease and consult a doctor. This will make it possible to make a correct diagnosis in a timely manner and prescribe adequate treatment, which will stop the progression of the disease and reduce to zero the risks of developing other pathologies.
Traditional methods of treating varicose veins
There are many folk recipes for infusions, decoctions, lotions and compresses. A number of remedies are advised to be taken even internally. Below are several options for treating varicose veins using traditional methods.
Lilac tincture
Take a container with a volume of one and a half liters, pour flowers and lilac leaves into it. Then everything is filled with vodka or medical alcohol so that the liquid completely covers the grass (to the very edge of the container). Infuse for a week, shaking occasionally, then filter and rub the tincture on your feet every day. Rub the skin with soft massage movements, from fingers to knees.
With the help of tincture they fight inflammation, swelling, cramps, and pain in the legs.
Garlic ointment
Garlic cloves from a whole head are peeled, ground in a meat grinder or pressed through a garlic press. After this, you need to take butter (unsalted) and mix with crushed garlic in a ratio of 1:2 (2 parts butter and 1 part garlic). Apply this mixture to the affected leg, cover with wax paper, bandage it, the compress can be kept overnight.
The compress eliminates pain and burning sensation, it has antiseptic properties, softens the skin, and helps heal wounds.
Honey with garlic
You need to take a head of garlic and 250 ml of honey (preferably linden or buckwheat). Both ingredients are thoroughly mixed and left for a week. Drink a tablespoon three times a day, before meals. The product relieves swelling and fatigue, pain, and varicose veins become less noticeable.
Potato juice
Raw potatoes are crushed on a grater or in a blender, and the pulp is applied to sore spots. Keep the compress for about half an hour; if desired, you can leave it on all night. To increase efficiency, drink half a glass of potato juice at the same time. The product relieves swelling and discomfort in the leg, eliminates heaviness, reduces fatigue and inflammation.
Butter with onions
A glass of olive oil and the same amount of onion peels are mixed in a glass bowl, two teaspoons of apple cider vinegar are added there. The mixture is hidden in a dark corner for 2 weeks, shaken periodically.
Before applying oil and onions to your feet, make a bath from a decoction of onion peels. Rub the limb with oil from the fingers to the knee. It is best to perform the manipulation before bedtime. Rubbing eliminates the heaviness and fatigue of the legs, although they cannot completely cure varicose veins.
Calendula-based ointment
Pour 2-3 tablespoons of dried calendula flowers with a glass of boiling water, leave until it cools down (you can use a thermos). Strain the infusion and mix with 250 g of any fatty substance (take Vaseline, lanolin, badger fat, etc.). To improve the smell, add a couple of drops of aromatic oil from mint, grapefruit, rose, lavender, and sage to the mixture. Rub the ointment on your feet until it is absorbed, apply twice a day. The infusion can be made combined; in addition to calendula, add thyme, hop cones, chamomile, and nettle.
Varicose veins of the lower extremities - stages
There are several stages of disease development:
- compensation – spider veins and tortuous veins appear on the legs, no complaints
- subcompensation – there are complaints of swelling, cramps of the calf muscles, a feeling of heaviness, fatigue in the legs, pronounced dilated veins are visually determined
- decompensation – dermatitis, minor hemorrhages are added, the skin becomes dense, dry, easily wounded, pigment spots appear
The earlier the disease is detected, the easier it is to treat.
What is the effect of wearing compression garments for varicose veins?
Compression garments cannot cure varicose veins. But wearing it slows down the disease, relieves many of the symptoms caused by it, and improves well-being.
After putting on compression hosiery, the lumen of the saphenous veins narrows, blood and lymph flow better and do not stagnate in the limbs. At the same time, swelling is relieved, convulsive contractions of the calves disappear, legs are less tired, and there is no feeling of heaviness.
The main types of compression garments prescribed for varicose veins are leggings, socks, stockings, and long tights. It is recommended to wear the products every day; you need to put them on in the morning, before getting out of bed, always in a lying position.
There are different degrees of compression of knitwear, they are chosen depending on the stage of varicose veins. Only the right underwear will have the proper therapeutic effect. It is best to be prescribed by a doctor, but stockings or tights with low compression, for prevention, are easy to purchase yourself.
Here's how different types of compression products are labeled:
- Class I – (18.4-21.1 mm Hg) – this is underwear with starting compression. It is suitable for preventing varicose veins in pregnant women, in people whose work involves significant physical exertion, or in the initial stages of the disease.
- Class II – (25.2-32.3 mmHg). Underwear with medium compression. It is used as a prophylactic against thrombophlebitis, after operations or sclerosis of veins.
- III Class (36.5-46.6 mmHg). High compression underwear. Indicated for patients with trophic ulcers on the legs, tissue nutritional disorders, in the presence of thrombosis in the deep veins, significant disturbances in the outflow of lymph and blood circulation.
- IV Class (more than 59 mmHg). Ultra-high compression underwear. Used in patients with elephantiasis and severe venous abnormalities.
Before purchasing, you need to determine exactly what compression class you need. Inquire about the labeling features of the products of your chosen company. Reputable companies always use the word “compression” to define the class and define it in mmHg. If “DEN” is written on the packaging, then this product has nothing to do with medical underwear.
Varicose veins of the lower extremities - treatment: surgery or still a procedure?
- Intravascular coagulation. Do you have varicose veins of the lower extremities? Laser treatment in Moscow is a small endovascular operation during which a vein is obliterated with a laser. Varicose veins of the lower extremities will be removed; laser treatment is based on the introduction of blood flow into the desired vein. This is how varicose veins of the lower extremities are defeated. Laser treatment, the cost of which is not so high, takes little time and is well tolerated by patients, and they forget that they had varicose veins of the lower extremities; laser treatment (the price in our center is affordable) is very effective. The final figure depends on the stage of the disease and the amount of work the doctor does. Do not be afraid that varicose veins of the lower extremities will attack again later. Laser treatment (there are quite a lot of reviews!) will definitely put you “on your feet”!
- Short stripping is a minimally invasive technique in which a small section of the affected main vein is removed. In this way, it is possible to preserve as many healthy sections of veins as possible.
- Cryophlebectomy – removal of a vein using a cryoprobe. The operation is low-traumatic - however, one small incision is made to insert the probe. After the operation, you see results immediately.
What effect does laser treatment bring?
Endovasal laser coagulation or treatment of varicose veins with a laser is a fairly effective technique. There are different options for this method of treatment - laser monotherapy, combined therapy (complex laser treatment with the use of drug sclerotherapy, deep vein ligation). Through the impact of laser beams on the diseased organ, they try to achieve sclerosis of too large and dilated veins, thus the altered areas are removed, some vessels are narrowed and blood flow is normalized. In addition, the treatment also has a cosmetic effect: stars and dilated vessels are removed, and the limb regains its normal appearance. The mechanism of action of the laser resembles the effect of sclerosing drugs. Soldering and further resorption of the affected vessels occurs. But with laser therapy there is no need to administer medications that may have side effects. During the operation, a small puncture is made in the area of the affected vein, and a laser light guide is inserted into it using a needle. Movements in the vein are monitored through an ultrasound machine. When the light guide reaches the desired location, the doctor turns on the radiation, which acts on the vein for several seconds. The walls are burned, and after some time their sclerosis occurs. The operation is performed under local anesthesia. The duration of the procedure is a little over an hour, it does not cause pain or discomfort to the patient. After just a couple of hours, the patient can get to his feet and go home on his own. Restrictions regarding work and physical activity are lifted after a week. During this period, it is recommended to lubricate problem areas (where the intervention was performed) with ointments or gels with heparin. A week after completing treatment, the person can return to their normal activities. To improve the condition of the limb and achieve optimal results, compression stockings are prescribed and must be worn constantly.
Laser treatment is indicated in the following situations:
- Varicose veins in relatively small areas of the vein.
- The mouth of the great saphenous vein is dilated by no more than 10 mm.
- Trophic disorders in the lower leg area.
There are few contraindications for laser therapy for varicose veins. One of the main ones is a strong expansion of the veins. There is a certain diameter of the vessel at which laser treatment can bring results and will not lead to relapse of the disease.
Why is reticular varicose veins considered a mild form?
Varicose veins of the lower extremities have a separate type - reticular varicose veins. It is common mainly among women and is considered a mild form of varicose veins because in this case only the thin veins dilate.
Reticular varicose veins are often called cosmetic, since the main symptoms are external manifestations in the form of spider veins on the calves and thighs. Reticular varicose veins occur most often due to wearing high-heeled shoes, severe physical activity and taking hormonal pills.
Despite the fact that reticular varicose veins are mild, they need to be treated to avoid possible complications. Treatment of pathology of this type is carried out with the help of ointments, gels, venotonic nature, drug therapy, laser. Traditional surgical operations performed with a laser, especially a scalpel, are very rarely used.
Varicose veins causes (mechanism). Risk factors for developing varicose veins:
- Staying on your feet for a long time (more than 50% of working time)
- Work involving heavy lifting (loaders, athletes)
- Overweight and obesity (increases strain on legs)
- Inactive lifestyle (“office work”)
- Pregnancy and childbirth (especially repeated ones)
- Chronic constipation (increased intra-abdominal pressure)
- Taking hormonal medications (including contraceptives)
- Private, long-haul air travel (“Economy class varicose veins”)
- Thermal loads (baths, saunas, hot baths)
- High heels (shifting the center of gravity increases the load on the legs)
Varicose veins complicated by venous eczema
Against the background of existing swelling, foci of hyperemia (redness), exfoliation of the epidermis (peeling of the skin) appear, accompanied by itching of the skin. This complication already brings significant discomfort to the patient’s life and most often forces him to seek medical help. Often such patients can be treated by a dermatologist for a long time without success. It is very important that at this stage the patient still reaches a good phlebologist. Only in this case will he be provided with truly adequate medical care.