Vegetative-vascular dystonia is one of the most frequently diagnosed diagnoses in neurological practice, especially at the outpatient stage of treatment. However, I personally am increasingly asked the question of what it is if there is information on the Internet that “there is no such diagnosis in the West.” That is why I decided to touch upon the topic of vegetative dystonia on this site and consider this issue within the framework of the symptom of dizziness. And also at the same time tell why there is no point in using information on the Internet without having the proper medical data for its full processing and understanding.
Causes of VSD: the essence of the diagnosis
In the human body, as I prefer to say during my appointment, there are three sections of the nervous system: central (brain and spinal cord), peripheral (spinal cord roots and individual nerves) and autonomic (including the vagus nerve - emerging from the structures of the brain, autonomic nerve plexuses, including the solar-celiac plexus and carotid glomerulus, as well as individual vegetative cells). So, the functions of the central nervous system are the mind, information processing, most of the sensory organs due to the cranial nerves (vision, hearing, taste, etc.), integrative tasks, as well as the development of a command to act. The peripheral nervous system provides control over the human body, facilitates the collection of information (temperature sensitivity, tactile sensitivity, etc.), and also ensures the execution of commands for action. The autonomic nervous system is practically independent of our consciousness and controls autonomic functions: vascular tone, including the brain, blood pressure, heart rate, respiratory rate, production of exocrine and internal secretion glands (including sweat glands). All this provides a double and sometimes even triple system of control of important functions of the human body. At the same time, in the autonomic nervous system there are inhibitory and excitatory influences in balance, which, by changing the strength of these influences, regulate the functions described above.
However, the autonomic nervous system is in close relationship with other departments, in particular, through the work of the vagus nerve, which is a cranial nerve. The vagus nerve nuclei, in turn, interact to some extent with the limbic structures of the brain responsible for emotions and perceptions of stress. In general, the human body is a single and very complex structure. Therefore, an imbalance in one part of the nervous system can lead to disturbances in another part. Thus, the presence of chronic or simply severe acute stress, congenital structural features of the autonomic nervous system, the influence of debilitating diseases, hormonal changes (during puberty, as well as during menopause in women), as well as some other factors lead to an imbalance of inhibitory and excitatory influences and the development of various types of disorders, including changes in cerebral vascular tone. This is exactly how, due to this imbalance and changes in vascular tone, a symptom complex of such a condition as vegetative-vascular dystonia (VSD, vegetative dystonia, vegetative dystonia syndrome, these are all synonyms) is formed.
So, VSD is not a disease in the full sense of the word, “in the West” there are no separate codings according to the ICD 10 system for various forms of VSD, this is what led to the appearance of information about the absence of such a diagnosis in European and American practice. At the same time, psychological and psychotherapeutic assistance is very well developed there, and since one of the most important factors in the development of vegetative dystonia is stress, very often this problem is dealt with there more often not by doctors, but by psychologists, and, less often, by psychotherapists (and the diagnosis implies somatoform autonomic dysfunction, which is encrypted in class F and cannot be made as the main diagnosis by a therapist or neurologist).
In domestic realities, going to a psychotherapist for a patient means the presence of a certain “stigma”, and psychological support is unsatisfactorily developed and is quite expensive. Therefore, neurologists often deal with these problems. And they are forced to make a diagnosis due to the bureaucratic aspects of paying for visits, diagnostic procedures, etc. In this case, the generally accepted ICD 10 system is used, which still contains the term other disorders of the autonomic nervous system - code G90.8. And it is the code G90.8 that is the ICD 10 code for autonomic dysfunction. At the same time, according to the data I have, in the near future, with the adoption of ICD 11, a whole list of codes for this classification system will appear, responsible for coding this diagnosis. And there is a whole section 8D** responsible for coding these diagnoses.
Diagnosis of vegetative-vascular dystonia
Body aches, weakness in the arms and legs, and a crawling sensation can be symptoms of many diseases. Neurologists at the Yusupov Hospital conduct a comprehensive examination of patients with signs of VSD. Instrumental studies are carried out using the latest equipment from leading global manufacturers. For laboratory research, high-quality reagents are used to obtain accurate test results.
The cause of pain in the body, crawling sensations, numbness of the limbs, trembling of the hands may not be VSD, but organic lesions of the brain. At the Yusupov Hospital they are excluded or confirmed using magnetic resonance imaging. When performing an MRI of the brain using special modes, doctors see changes in the brain tissue itself.
If a patient with VSD has blood pressure that rises infrequently, these changes are reversible. With persistently high blood pressure, dyscirculatory encephalopathy develops. More often, such changes occur in areas of the brain with initially reduced blood flow. In the process of diagnosing the causes of VSD, a clear analysis of the cerebral vessels is necessary. Such a study is carried out at the Yusupov Hospital using the latest generation MRI machines using special MRI programs. They make it possible to determine the state of cerebral vessels without administering contrast. Timely assessment of the state of the brain is important for the prevention of hypertensive crises, since hypertensive VSD can result in a cerebral stroke.
An important addition to MRI studies for VSD is ultrasound of the vessels of the brain and neck. It shows the function of blood vessels in dynamics, allows you to navigate those parts of the VSD that are disturbed, clarify the cause of autonomic dysfunction and make a decision on the choice of treatment tactics. Ultrasound examinations at the Yusupov Hospital are carried out using expert-class equipment. In order to identify vascular disorders of the brain and VSD in particular, doctors analyze the venous component of cerebral blood flow. For this purpose, unique diagnostic developments are used, which make it possible to determine with a high degree of reliability the nature and cause of VSD using computer and ultrasound analysis of slow and fast cerebral venous blood flow.
Symptoms
The symptoms of vegetative dystonia can be practically loved, without exaggeration. These may include changes in blood pressure, increased sweating, rapid heartbeat, sleep disturbances, bowel movements (vomiting, constipation, etc.), headaches, general weakness, and mood swings. There may be muscle pain, transient, numbness and crawling that do not have a clear localization. The person may experience discomfort in the chest and a lump in the throat. The symptoms of autonomic dysfunction are diverse and multifaceted. However, as part of the site about dizziness, I wanted to dwell on this symptom in more detail.
Dizziness with VSD may occur. However, nevertheless, it is rarely (almost never) systemic in nature, but fits more into the framework of non-systemic dizziness in the form of a fainting state or general lightheadedness, and may have signs of psychogenic dizziness. It does not have a fixed time frame and often depends on stress factors and weather conditions. Most often, it is not accompanied by tinnitus or nausea leading to vomiting, although nausea may be present.
Symptoms of VSD in the acute stage
The cardiovascular symptom complex in VSD is manifested by the following symptoms:
- changes in heart rate;
- lability of blood pressure;
- pathological vasomotor reactions (redness, cyanosis, pallor of the skin, hot flashes, chilliness of the feet and hands).
In the acute stage, burning, stabbing, pressing, throbbing pain or discomfort in the heart area is observed.
The respiratory symptom complex is manifested by increased ventilation (rapid deep breathing), psychogenic shortness of breath (sniffling, yawning, coughing, periodic deep breaths). Hyperventilation always accompanies anxiety. Shortness of breath is accompanied by dissatisfaction with inhalation, a feeling of lack of air, intermittent breathing, and a feeling of stopping breathing. In the acute stage, muscle spasms and a crawling sensation around the mouth and in the distal limbs occur. Neurologists define Chvostek's symptom - contraction of the muscle that raises the corner of the mouth when tapped in the projection of the facial nerve. Hyperventilation may cause the following symptoms:
- headache;
- fainting state;
- pain in the heart area;
- heart rhythm disturbance;
- abdominal pain, combined with increased peristalsis, nausea, and belching of air.
The gastrointestinal symptom complex is characterized by a disorder of the functions of the digestive organs. May exhibit the following symptoms:
- disturbances of appetite, motility of the esophagus, stomach or intestines;
- psychogenic dysphagia (difficulty, discomfort during the act of swallowing or the inability to take a sip);
- vomiting;
- feeling of heaviness in the epigastrium;
- transient flatulence (bloating);
- diarrhea;
- pain in the abdominal cavity.
The thermoregulatory symptom complex is manifested by an increase or decrease in temperature, chill syndrome. The vasomotor symptom complex consists of several symptoms:
- pallor, cyanosis of the skin;
- chilliness of hands, feet;
- sensations of hot or cold flashes;
- changes in dermographism (weak mechanical irritation of the skin when carried out with a blunt object causes a trace in the form of inflamed swelling);
- increased sweating of the palms and feet.
The genitourinary complex is characterized by cystalgia (frequent, painful, imperative urination in the absence of pathology of the urinary system or changes in urine) and sexual dysfunction (impaired erection or ejaculation in men, vaginismus or anorgasmia in women with preserved or reduced libido, painful menstruation). Hormonal fluctuations, including endocrine changes in the body after childbirth, and postpartum stress provoke an exacerbation of VSD symptoms.
The neurotic symptom complex is manifested by the following symptoms:
- fatigue;
- asthenia;
- low threshold of pain sensitivity;
- sleep disorders;
- irritability;
- senestopathies (pain in the heart, a feeling of dissatisfaction with inhalation, a burning sensation in different parts of the body).
VSD occurs with a wave-like increase and decrease in the manifestations of symptom complexes. This is due to changes in etiological factors and living conditions of the patient. An exacerbation of VSD may occur in the fall. Symptoms of the disease are most pronounced during a “vegetative storm” or crisis.
Diagnostics
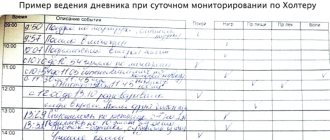
The diagnosis of vegetative-vascular dystonia is still rather a diagnosis of exclusion. If the neurological status does not have any focal neurological symptoms, pathological reflexes, and there is vegetative stigmatization (hyperhidrosis, marbling of the skin color, increased dermographism, etc.), and there is not the slightest evidence for the presence of other diseases that could would cause this condition, we can talk about VSD. Relatively reliable studies that confirm the presence of autonomic dysfunction are REG, EEG, as well as stress autonomic tests (orthoclinoplasty and others).
Most often, “real” vegetative-vascular dystonia occurs at the age of 14-30 years, as well as in the age period of 45-55 years in women.
Treatment
Treatment of vegetative-vascular dystonia is the subject of enormous controversy in the scientific community. Who should make this diagnosis? Neurologist, therapist or psychiatrist? How to treat this condition and how – symptomatically or try to find the mechanisms of pathogenesis of this condition?
But disputes are disputes, and on this site I share my opinion. The most important thing is non-drug therapy, namely psychological support, stabilization of lifestyle (sleep, work conditions, family situation, bad habits, etc.); in the presence of panic conditions, consultation with a psychiatrist and the prescription of anti-anxiety therapy are indicated. In all cases, restorative therapy will not be harmful (including B vitamins, their derivatives, in particular Enerion, such “soft” drugs as Mexidol, Neurox, Ethoxidol, Armadin, Fnibut, etc.). In the presence of dizziness, the prescription of vertigolytics (Betaserc, Vestibo, etc.) is controversial, because there is usually no substrate for their work. It is more important to use vestibular rehabilitation and vestibular gymnastics techniques than drug treatment.