Causes
Doctors consider varicose veins to be the main cause of phlebitis. In addition, we can name a number of other factors that can provoke the development of pathology:
- Excess weight: this puts even more strain on the veins.
- Low physical activity: it has become the scourge of the 21st century.
- Prolonged vertical position, for example, store clerks are forced to stand behind the counter all day.
- Abnormal bowel movements, for example constipation.
In some cases, allergic reactions can also trigger the development of the disease. Much less often, the development of phlebitis is caused by injury to a vein or its damage as a result of the development of an infectious disease. No matter what the cause of the disease is, it cannot be left without treatment, so as not to develop serious complications.
At risk:
- People over 40 years old
- Trauma patients
- Patients with infectious and bacterial diseases
- People leading a sedentary lifestyle
- Obese patients
- Patients with heart failure
- People taking hormonal medications
- Pregnant
- Women taking birth control pills
- Cancer patients
- People who have undergone surgery on the pelvic organs and lower extremities.
Classification
Pathology is classified in several directions. According to the nature of its course, phlebitis can be:
- acute – accompanied by pain in the affected veins, weakness and fever;
- chronic - can be asymptomatic for a long time, appearing only during exacerbations.
At the location of the affected objects:
- phlebitis of superficial veins;
- Phlebitis of deep veins.
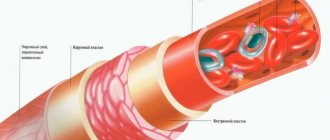
Depending on the location of the inflammatory process in the vein, the following forms of phlebitis are distinguished:
- endophlebitis – inflammation develops on the inner lining of the vein;
- periphlebitis – inflammation develops on the outer lining of the vein;
- panphlebitis - both the inner and outer lining of the vein are involved in the inflammatory process.
The main causes of thrombophlebitis
- Varicose veins.
Large varicose veins contain thick, slow-moving blood. In the presence of varicose veins, thrombosis and inflammation of the vessel wall may occur. Thrombophlebitis is accompanied by thickening of the venous wall, pain and fever. It can be life-threatening if a blood clot grows along the main venous trunks.
- Intravenous injections.
The third most common cause of the development of thrombophlebitis should be recognized as various medical procedures associated with intravenous administration of drugs. In most cases, this happens on the upper limbs. It should be recognized that these thrombophlebitis are very benign and in most cases do not require any treatment. The administration of certain medications and drugs greatly irritates the vein wall and causes inflammation and swelling. Blood flow through the vein slows down, and thrombosis occurs. A painful cord forms along the vein. It is usually not life-threatening. She is being treated on an outpatient basis. Systemic inflammatory diseases - systemic lupus erythematosus, endarteritis and many other diseases of the immune system damage the vascular wall. Antibodies are produced to one's own blood vessels, which attack the inner lining of the blood vessels and cause inflammation and the formation of blood clots. Treatment of the underlying disease contributes to the treatment of thrombophlebitis.
- Heredity
A hereditary tendency to form blood clots (thrombophilia) can cause thrombophlebitis, especially with varicose veins. A number of people have congenital deficiencies of various factors of the blood anticoagulation system. These patients are characterized by frequent thrombophlebitis and deep venous thrombosis. They often have to take medications that reduce blood clotting for life.
- Oncology
Oncological pathology also leads to significant disruption of blood clotting. Thrombophlebitis is often one of the first signs of cancer. A thorough examination of the patient (cancer search) allows one to identify a tumor at an early stage and radically cure it. If thrombophlebitis develops in a vessel unaffected by varicose veins, this may be the first sign of the so-called paraneoplastic syndrome - a thrombotic process that develops against the background of cancer. Very often, thrombophlebitis occurs when the pancreas is damaged. And this is one of the reasons why thrombophlebitis should not be treated as a mild disease; at the first signs of thrombophlebitis, you should immediately see a phlebologist.
- Local factors
Conditions under which thrombophlebitis often develops include trauma, surgery, immobilization, and prolonged bed rest. Often thrombophlebitis without varicose veins can occur after visiting steam rooms, saunas and other similar “thermal” procedures. The medical literature has repeatedly raised the issue of the development of varicothrombophlebitis in women taking hormonal contraceptives. In general, in women, hormonal levels greatly affect blood vessels, which is why pregnancy, childbirth, and abortions are often complicated by thrombophlebitis of the lower extremities.
Among other things, the location of the veins directly under the skin predisposes them to the possibility of injury in public transport or during sports. The more advanced a person’s varicose veins are, the greater the likelihood of thrombophlebitis.
Types of phlebitis
Depending on the cause of its occurrence, phlebitis is classified into the following types:
- Post-injection phlebitis. Caused by chemical irritation of the venous walls, an administered drug, or mechanical trauma.
- Allergic phlebitis. Caused by an allergic reaction to an allergen.
- Painful phlebitis. It often develops after childbirth, is acute and is accompanied by intense pain.
- Cerebral phlebitis. Inflammation of the cerebral veins is caused by infectious diseases or purulent inflammations (abscesses, phlegmons).
- Migrating phlebitis. Long-term inflammation of the leg veins, more often observed in young men. It occurs with relapses and may be accompanied by the spread of inflammation to the walls of the arteries.
- Phlebitis of the penis. Caused by varicose veins or infectious diseases (for example, gonorrhea). Accompanied by swelling of the skin and the formation of a voluminous cord-like compaction on the dorsum of the penis.
- Phlebitis of the portal vein (or pylephlebitis). Caused by a complicated course of inflammatory processes in the abdominal cavity (appendicitis, liver abscesses, peptic ulcers, purulent inflammation of the genital organs, hemorrhoids, dysentery, purulent infection of the umbilical vein of newborns, etc.). Often leads to death.
Symptoms and clinical manifestations
The onset of inflammation of the veins can be judged by pain in the legs. At the initial stage, it is short-term, usually towards the end of the day after prolonged work. Patients often mistake it simply for a sign of fatigue. The pain may be accompanied by swelling of the legs in the evening or in the morning.
Signs of superficial phlebitis
Due to the close proximity of the superficial veins, signs of inflammation are clearly visible:
- the appearance of pigmentation at the site of the lesion, the spots resemble red-brown bruises;
- the veins are hard to the touch, often protrude on the surface of the skin, the pulsation is clearly palpable;
- in places of inflammation - a noticeable increase in skin temperature, itching, soreness;
- the appearance of a “web” along the vein.
In the acute form of the disease, a rise in temperature, lethargy and dizziness are observed. When the form is advanced, ulcers and wounds may appear on the skin. Chronic phlebitis of superficial vessels has the same symptoms, but in a blurred form. Symptoms appear during exacerbations, in a state of remission - patients complain of fatigue, heaviness in the legs, low-grade fever (just over 37°).
Signs of deep vein phlebitis
Phlebitis, in which the deep veins are affected, is characterized by constant heaviness in the legs and swelling of the limbs. If the inflammation affects only one leg, it is noticeably different from the second. The patient's temperature rises to 37-38°; if treatment is not started, it can last for several months. The skin on the legs becomes bluish or pale.
There is constant pain in the legs, which intensifies with physical activity. Often inflammation of the deep veins is accompanied by the formation of blood clots and thrombophlebitis. Induration and ulceration appear.
Dangerous consequences of this disease can be heart attack and stroke or pulmonary embolism.
Exacerbation of phlebitis
In most cases, the patient does not notice the onset of the inflammatory process in the vessels. The pain is intermittent and goes away after rest. The patient does not consult a doctor in a timely manner. Therefore, it is often necessary to treat an exacerbation of the disease. During an exacerbation, there is a significant rise in temperature, above 38°, with a feverish state, pain in the legs, severe swelling of the extremities, general weakness and dizziness, swelling on the legs, with a sharp change in skin color, ulcers.
This condition requires immediate help. The disease is treated by a phlebologist-angiologist.
Diseases of the veins of the lower extremities: varicose veins, phlebitis, thrombophlebitis, thrombosis.
In addition to varicose veins, diseases of the veins of the lower extremities include quite a few diseases.
The causes of diseases of the veins of the lower extremities can be different. However, all diseases appear as a result of poor nutrition, poor lifestyle, bad habits, difficult working conditions, hormonal disorders or heredity.
The symptoms of vein diseases are similar.
Establishing a correct diagnosis is very important. The treatment of each disease of the veins of the lower extremities has a number of fundamental differences.
Among the diseases of the veins of the lower extremities, phlebologists name varicose veins, phlebitis, thrombophlebitis, thrombosis, trophic ulcers, chronic venous insufficiency, thromboembolism, etc.
Varicose veins
- This is varicose veins. Most often, varicose veins affect the lower extremities. Varicose veins are lesions of the venous walls. With the development of varicose veins, the walls of the veins are damaged, they become thinner and expand due to impaired blood flow. Varicose veins lead to decreased tone of the venous walls and valve insufficiency. As a result of pathological processes, venous outflow becomes more difficult, and the lumen in the veins increases. The valves are subject to deformation, their walls become thicker and shorter.
The reasons for the development of varicose veins, as a rule, are heredity, excess body weight, severe prolonged tension in the legs, physical inactivity or a sedentary lifestyle, a sedentary lifestyle, in women, pregnancy and childbirth, hormonal imbalance, bad habits (alcohol, smoking, drugs), long-term use of medications and hormonal drugs.
Varicose veins can be recognized by the following symptoms, which are characteristic of all diseases of the veins of the lower extremities:
- swelling of the legs, worsening in the evening;
- heaviness in the legs;
- bursting sensation in the calves;
- bulging veins.
With vigorous activity or during sleep, symptoms become less obvious.
However, the disease develops, and the symptoms become more pronounced: pain, heat in the lower extremities, and cramps appear. Telangiectasias appear on the skin.
A phlebologist at the Only Clinic conducts a phlebological examination: examines the patient and prescribes diagnostic measures, including duplex scanning and contrast venography.
The treatment prescribed by the Only Clinic phlebologist depends on the results of the phlebological examination.
As a rule, phlebological treatment of varicose veins in Nizhny Novgorod includes the use of medications, traditional medicine, physical therapy, wearing compression garments and surgical methods.
Drug treatment
varicose veins in the Only Clinic involves the use of drugs that strengthen vascular walls and thin the blood, for example phlebotonics, anticoagulants, venotonics, non-steroidal anti-inflammatory drugs.
Phlebologists at Only Clinic also recommend using local medications (ointments) to relieve pain and swelling.
At stages 3 and 4 of varicose veins, the only effective treatment is surgery.
Surgical operations for the treatment of varicose veins performed at Only Clinic include:
- sclerotherapy is when the inflamed vein is resolved with the help of a special sclerosant preparation;
- laser therapy is a procedure to turn off a diseased vein from the bloodstream using a laser beam;
- classic phlebectomy is the removal of a vein under anesthesia.
Phlebitis
- This is an inflammatory process of the walls of the veins.
Phlebitis usually develops against the background of varicose veins of the lower extremities. The inflammatory process leads to impaired blood flow and the formation of blood clots. Untreated phlebitis can lead to a more dangerous disease - thrombophlebitis.
Symptoms of the development of phlebitis are pain; skin redness; temperature increase; general weakness; swelling.
Phlebitis can become chronic. In the chronic form, the symptoms of phlebitis either subside, going into remission, or sharply worsen.
Treatment of phlebitis, as a rule, is quite lengthy and consists of several stages and must be comprehensive.
In the initial stage of phlebitis, hospitalization is not required.
If the disease is advanced, then the patient with phlebitis must be hospitalized.
While in the hospital, the patient undergoes a series of procedures. The patient is prescribed bed rest, while the patient's legs should be at rest and at some elevation.
To treat phlebitis, a phlebologist prescribes drugs that strengthen the walls of the veins, reduce blood density and eliminate inflammation.
After the acute phase of the disease and exacerbation are removed, the patient is prescribed to wear compression garments and bandage the legs with an elastic bandage.
Without fail, in order to relapse phlebitis, the phlebologist prescribes a diet and medication to reduce cholesterol in the blood.
Thrombophlebitis develops as
complication of varicose veins. Thrombophlebitis is characterized by an inflammatory process on the walls of the veins and the formation of blood clots.
The most common site of localization of the disease is the lower extremities (from the lower part of the buttocks to the lower part of the lower leg).
The causes of thrombophlebitis can be excess body weight, pregnancy, injury, some kind of virus, heredity, sedentary lifestyle, physical inactivity, diabetes, overheating.
Thrombophlebitis usually develops against the background of untreated phlebitis.
Thrombophlebitis can be recognized by the following symptoms. This is severe pain in the calf muscles, general malaise, high body temperature, redness of the skin, skin thickening, weakness in the lower extremities, a feeling of coldness in the toes, limping when walking.
Thrombophlebitis can develop rapidly: body temperature can suddenly and sharply rise to 38 - 39 degrees. Severe pain and redness of the skin are observed in the vein area.
Typically, this acute phase of thrombophlebitis lasts for 10-30 days.
After this, the disease thrombophlebitis becomes chronic.
Treatment of thrombophlebitis in Nizhny Novgorod must begin as early as possible, at the first symptoms.
To get rid of thrombophlebitis in a modern private medical clinic, as a rule, drug therapy or surgery is prescribed.
A patient with thrombophlebitis takes medications on an outpatient basis if the blood clot has not spread beyond the lower leg. If the disease is caused by injury to the venous wall, anticoagulants or an alcohol compress are used. Also, the phlebologist at the Only Clinic prescribes anti-inflammatory drugs to the patient.
Phlebologists usually include the following medications in the course of treatment for thrombophlebitis: phlebotonics (Detralex, Venosmin); angioprotectors (rutin derivatives); non-steroidal anti-inflammatory drugs (Sinmeton, Diclofenac, Meloxicam); anticoagulants (Warfarin, Sinkumar).
Surgical treatment of thrombophlebitis must be resorted to if the disease has spread to the deep veins, as well as if there is a risk of complications.
Surgical methods for treating thrombophlebitis include ligation of pathological vessels; thrombectomy (removal of a blood clot); phlebectomy (removal of veins affected by the pathological process).
Thrombosis
Phlebologists diagnose if there is a violation of the inner surface of the venous wall of the deep veins.
Phlebologists name the reasons for the development of thrombosis as infection, chemical or mechanical damage to the veins, as well as an allergic reaction.
The risk of thrombosis increases greatly if there is high blood clotting or congestion in the veins of the lower extremities due to low physical activity or prolonged standing.
IMPORTANT! Physical inactivity is the main factor leading to thrombosis!
When a person sits in a sitting position with bent legs for many hours, blood stagnates in the deep veins, which provokes the development of thrombosis.
Causes of blockage of blood vessels: increased blood viscosity due to a lack of fluid in the body, as well as as a result of metabolic disorders or the effects of a malignant tumor, stagnation of blood in the legs resulting from physical inactivity, varicose veins or inflammatory disease, pathology of the circulatory system (thrombophlebitis, erythremia) , genetic factor, infectious diseases (sepsis, allergies), pneumonia, obesity, diabetes.
At the initial stage, the symptoms of thrombosis are usually mild. However, over time, more and more signs of thrombosis appear, including: swelling of the lower extremities, formations in the form of spider veins, discoloration of the skin on the legs, cramps, especially disturbing at night, pain in the thigh, lower leg and foot (pain subsides with horizontal location of the limb), venous insufficiency, elevated body temperature.
In the acute stage, thrombosis proceeds rapidly: venous outflow completely or partially stops; thighs and legs increase in size; the saphenous veins dilate noticeably; cyanosis occurs; body temperature rises to 38 degrees.
The choice of treatment tactics for thrombosis at the Center for Modern Medicine Only Clinic depends on the stage of the disease, the general health of the patient, and the location of the pathology.
The main goal in treating thrombosis is to stop the spread of thrombosis, as well as to prevent pulmonary embolism (that is, blockage of the arteries of the lungs). Treatment is carried out only in a hospital setting.
A patient with thrombosis is prescribed strict bed rest and medications, including anticoagulants, thrombolytic and fibrinolytic drugs, as well as antiplatelet agents.
Surgery to remove thrombosis is performed if the patient’s life is threatened.
Treatment methods for deep vein thrombosis:
Drug therapy: Medications are prescribed to reduce symptoms and normalize blood flow. As a rule, a phlebologist prescribes coagulants (Coumadin, Heparin, Warfarin) to reduce blood thickness and prevent thrombosis in the vessels and veins of the legs, as well as reduce swelling.
Also, to eliminate thrombosis, it is necessary to take thrombolytic agents (Trypsin, Chymotrypsin) and phlebotonics.
Surgical treatment of thrombosis is indicated when there is a risk of thrombus rupture.
Surgery is contraindicated at the stage of exacerbation of the disease and in certain cardiovascular pathologies.
The use of traditional medicine is useful to prevent the development of thrombosis. Phlebologists recommend the use of herbal tinctures and foot baths based on nettle, horse chestnut, and chamomile.
Phlebologists at Only Clinic can also recommend moderate exercise, including walking and therapeutic exercises, for patients with thrombosis.
If thrombosis is diagnosed, the patient is strictly prohibited from activities with high stress on the feet, as well as thermal procedures (sauna, steam bath, hot baths).
A consultation appointment on the problems of varicose veins, thrombosis or phlebitis at the Only Clinic costs 1,200 rubles.
Examination by a phlebologist, including ultrasound of the veins of the lower extremities - 2100 rubles.
Call! We will help!
Diagnostics
Typically, the diagnosis of phlebitis of both superficial and deep veins does not cause difficulties. A phlebologist may suspect a disease based on complaints from patients and examination data. To identify other forms and causes of inflammation of the veins and prevent the development of inflammation, a comprehensive examination is carried out.
Laboratory and instrumental research methods:
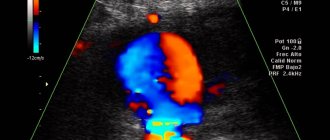
- ultrasound duplex scanning of blood vessels;
- blood tests: C-reactive protein, prothrombin index, coagulogram, CBC, thrombelastogram;
- phlebography;
- Ultrasound of vessels of adjacent organs.
More accurate instrumental diagnostic methods carried out for suspected thrombophlebitis:
- CT phlebography with contrast;
- phlebomanometry;
- Phleboscintigraphy.
Complications
Most often, thrombophlebitis is complicated by the spread of blood clots to the deep veins with the development of deep vein thrombosis and thromboembolism. The frequency of this complication is about 10% of all patients.
Purulent thrombophlebitis develops when an infection joins the inflammatory process. Suppuration is characterized by a sharp increase in temperature, chills, and a change in the number of leukocytes in the blood. Purulent thrombophlebitis can lead to the development of sepsis - a general blood infection and therefore requires emergency surgical care.
Features of therapy
Treatment of inflammation of the veins of the lower extremities includes medications and physiotherapy. For severe complications, surgical methods may be used.
Drug therapy
The following drugs are used to treat phlebitis:
- Antibiotics in case of infection. Taking them is also necessary in order to prevent infection. A frequently prescribed drug is Amoxicillin, which is a broad-spectrum drug.
- Non-steroidal anti-inflammatory drugs. These are different drugs containing diclofenac, ibuprofen, paracetamol. to improve microcirculation - Trental, Actovegin.
- To reduce viscosity - Aspirin, Cardiomagnyl.
- Anticoagulants – Heparin, improve circulation and prevent platelet aggregation.
- Histamine blockers - Tavegil, Suprastin.
When superficial veins are affected, local treatment is successfully used. Anti-inflammatory gels and ointments containing diclofenac, ibuprofen or their analogues are used. Local anticoagulant agent - Troxevasin, Heparin ointment. To treat endophlebitis, which most often appears as a result of unsuccessful intravenous injections, non-steroidal anti-inflammatory drugs are used in the form of tablets and topically. If an infection occurs, antibacterial drugs are prescribed. This disease is usually treated in a hospital.
Physiotherapy
Physiotherapy procedures are aimed not only at relieving inflammation and reducing swelling of the lower extremities, but also at increasing immunity and improving blood flow. Depending on the condition and characteristics of the course of the disease, the following may be prescribed:
- magnetic therapy;
- acupuncture;
- hirudotherapy - treatment with leeches;
- mud treatment and baths;
- infrared irradiation.
Sometimes compression stockings are prescribed; they support muscles and help blood vessels cope with stress. For superficial vein damage, an iodine mesh can be applied.
For various forms of phlebitis, complete rest is recommended. Pillows should be placed under sore legs so that they are higher than the heart. Periphlebitis of the lower extremities usually begins due to a pathological process in neighboring tissues, which is transmitted to the outer walls of the veins. Therefore, a mandatory aspect of therapy is the fight against the primary disease.
Surgery
If conservative treatment does not produce an effect and the exacerbation does not go away, the following types of surgical measures may be prescribed:
- removal of part of the vein - venectomy;
- ligation of the damaged part of the vein;
- vein bypass - insertion of an artificial vessel.
Surgery is usually necessary if blood clots form in the blood vessels.
Folk remedies
To treat phlebitis of the superficial veins use:
- Compresses made from buckwheat flour and cabbage leaves poured with boiling water.
- To relieve inflammation, use a compress of wormwood and fern leaves, mixing them with yogurt or sour cream.
- To strengthen the veins, make an infusion of beet tops. It is taken orally for 1-2 months.
Diagnosis and treatment of superficial (saphenous) vein thrombosis
Thrombosis of the superficial (subcutaneous) veins in clinical practice is referred to as “thrombophlebitis”. In the vast majority of cases, thrombophlebitis is a complication of chronic venous diseases that occur with varicose transformation of the saphenous veins (varicothrombophlebitis). Clinical signs: • pain along the thrombosed veins, limiting limb movements; • a stripe of hyperemia in the projection of the affected vein; • on palpation - a cord-like, dense, sharply painful cord; • local increase in temperature, hyperesthesia of the skin. When examining a patient with suspected thrombophlebitis, it is necessary to examine both lower extremities, since bilateral combined damage to both superficial and deep veins is possible. In addition to identifying symptoms of thrombophlebitis in patients suspected of having this disease, it is necessary to specifically determine the presence of symptoms indicating PE. The value of a physical examination for accurately establishing the extent of thrombosis is low due to the fact that the true prevalence of saphenous vein thrombosis is often 15-20 cm higher than clinically detectable signs of thrombophlebitis. In a significant proportion of patients, the transition of the thrombotic process to the deep venous lines is asymptomatic. The main diagnostic method is compression ultrasound duplex angioscanning. The standard scope of ultrasound angioscanning must necessarily include examination of the superficial and deep veins of not only the affected, but also the contralateral limb to exclude simultaneous thrombosis, which is often asymptomatic. The deep veins of both lower extremities are examined along their entire length, starting from the distal parts of the leg to the level of the inguinal ligament, and if intestinal gas does not interfere, then the vessels of the iliocaval segment are examined.
Indications for hospitalization: localization of acute thrombophlebitis on the thigh; — localization of acute thrombophlebitis in the upper third of the leg with damage to the small saphenous vein. Such patients should be hospitalized in vascular surgery departments. If this is not possible, hospitalization in a general surgical hospital is acceptable. Therapeutic tactics For thrombosis of superficial veins against the background of varicose veins, a more active surgical tactic seems appropriate.
Conservative treatment should include the following main components: 1) active regimen; 2) elastic compression of the lower extremities; 3) local therapeutic effect on the affected limb (cold, drugs containing heparin and/or NSAIDs).
4) systemic pharmacotherapy.
In case of spontaneous thrombosis of the superficial veins of the lower extremities, subcutaneous administration of fondaparinux sodium or prophylactic (or possibly intermediate) 1 dose of LMWH is advisable for at least 1.5 months. New oral anticoagulants (NOACs) (apixaban, dabigatran etexilate, rivaroxaban) should not be used for the treatment of saphenous vein thrombosis due to the current lack of data confirming their effectiveness and safety in this pathology. In addition to anticoagulants, in case of severe pain, it is possible to use non-steroidal anti-inflammatory drugs (NSAIDs) orally for 7-10 days. It should be taken into account that their combination with anticoagulants increases the likelihood of hemorrhagic complications. Intermediate doses include LMWH doses that are 50-75% of the therapeutic dose. It is not advisable to use antibacterial drugs in the complex treatment of superficial vein thrombophlebitis in the absence of signs of a systemic inflammatory reaction. Surgical treatment: 1. Crossectomy (Troyanov-Trendelenburg operation). High (immediately at the deep main) ligation of the large (or small) saphenous vein with mandatory ligation of all estuarine tributaries and excision of the trunk of the saphenous vein within the surgical wound. Indicated when thrombophlebitis spreads to the upper half of the thigh or estuarine tributaries when v. is affected. saphena magna and the upper third of the leg when affected v. saphena parva. The operation is feasible in any category of patients. 2. Thrombectomy from the main deep veins. Performed when thrombosis spreads beyond the sapheno-femoral or sapheno-popliteal ostium. The choice of access and thrombectomy method is determined by the level of location of the proximal part of the thrombus. After the anastomosis is released, a crossectomy is performed. 4. Miniphlebectomy in the pool v. saphena magna and/or v. saphena parva. Provides for the removal of all varicose veins (thrombosed and non-thrombosed) after crossectomy. It can be performed in uncomplicated patients in the first 2 weeks of the disease. At a later date, a dense inflammatory infiltrate in the area of varicothrombosis-lebitis prevents atraumatic removal of the affected veins.
5. Puncture thrombectomy from thrombosed nodes of the saphenous veins. Performed against the background of severe periphlebitis. Removal of blood clots from the affected veins under conditions of adequate postoperative elastic compression leads to a rapid reduction in pain and aseptic inflammation. Surgical treatment must be combined with the appropriate use of anticoagulants. Diagnosis and treatment of post-injection thrombosis of the saphenous veins of the upper extremities Clinical manifestations are similar to those of thrombosis of the saphenous veins of the lower extremities: - pain along the thrombosed veins; - a stripe of hyperemia in the projection of the affected vein; - on palpation - a cord-like, dense, sharply painful cord; - local increase in temperature. No special diagnostic methods are required.
Therapeutic tactics - only conservative treatment: - local therapeutic effect on the affected limb (cold, drugs containing heparin and/or NSAIDs); - in case of severe pain, it is possible to use NSAIDs orally for 7-10 days; — the use of anticoagulants is advisable only when the thrombotic process progresses and there is a threat of its spread to the subclavian vein. Diagnosis of DVT The formation of a blood clot can begin in any part of the venous system, but most often in the deep veins of the leg. There are occlusive and non-occlusive thrombus. Among non-occlusive thrombi, floating thrombi, which can cause pulmonary embolism, are of greatest practical interest. The degree of embolism of venous thrombosis is determined by the characteristics of the clinical situation. The decision about the degree of potential threat to the patient’s life is made by the attending physician based on a comprehensive assessment of the patient’s somatic status, characteristics of the thrombotic process and ultrasound angioscanning data. In this case, one should take into account the time of occurrence and localization of the thrombus, its nature (mobility in the lumen of the vein), the volume of the moving part and the diameter of the base. Embolic-dangerous thrombi are located in the femoral, iliac and inferior vena cava, the length of their moving part is usually at least 7 cm. However, in patients with low cardiopulmonary reserve due to concomitant pathology or previous pulmonary embolism, there is a real threat of life-threatening embolism. pain may represent floating thrombi of smaller sizes. Clinical manifestations depend on the localization of thrombosis, the prevalence and nature of damage to the venous bed, as well as the duration of the disease. In the initial period, with non-occlusive forms, clinical symptoms are not expressed or are completely absent. Sometimes the first sign of DVT may be symptoms of pulmonary embolism. A typical range of symptoms includes: • swelling of the entire limb or part of it; • cyanosis of the skin and increased pattern of subcutaneous veins; • bursting pain in the limb; • pain along the neurovascular bundle. For clinical diagnosis, the Wells index (Table 4) can be used, reflecting the likelihood that the patient has DVT of the lower extremities. Based on the sum of points scored, patients are divided into groups with low, medium and high probability of having venous thrombosis. Deep vein thrombosis in the superior vena cava system is characterized by: • edema of the upper limb; • swelling of the face, neck; • cyanosis of the skin and increased pattern of the saphenous veins; • bursting pain in the limb. Since clinical data do not allow us to judge with certainty the presence or absence of DVT, the diagnostic search should include subsequent laboratory and instrumental examination. Laboratory diagnostics Determination of the level of D-dimer in the blood. An increased level of D-dimer in the blood indicates actively occurring thrombus formation processes, but does not allow one to judge the location of the thrombus. The highest sensitivity (more than 95%) is provided by quantitative methods based on enzyme-linked immunosorbent assay (ELISA) or immunofluorescent assay (ELFA). After the development of thrombosis, the D-dimer gradually decreases and after 1-2 weeks can return to normal. Along with high sensitivity, the test has low specificity. Elevated levels of D-dimer are detected in many conditions, including tumors, inflammation, infection, necrosis, after surgery, during pregnancy, as well as in the elderly and patients in hospital. The upper limit of normal for D-dimer, determined by enzyme-linked immunosorbent methods, in persons under 50 years of age is 500 μg/l; in older age groups it is recommended to calculate it using the formula: age × 10 µg/l.
In connection with the described features, the following algorithm for using the D-dimer indicator for diagnosing DVT is proposed:
- patients without any clinical signs suggesting the presence of DVT should not have their D-dimer level determined for screening purposes; — patients with clinical symptoms and anamnesis that leave no doubt about the presence of DVT should not have their D-dimer level determined; — patients with clinical signs that suggest DVT, if it is not possible to perform compression ultrasound angioscanning in the next few hours, should determine the D-dimer level.
An increase in the indicator indicates the need for an ultrasound examination. If the medical institution does not have ultrasound equipment, the patient should be referred to another clinic with appropriate capabilities. In cases where the level of D-dimer in the blood is not elevated, the diagnosis of DVT can be rejected with a high degree of probability.
Instrumental diagnostics Ultrasound compression duplex angioscanning is the main method of examination for suspected venous thrombosis. The mandatory scope of the study includes examination of the saphenous and deep veins of both lower extremities, since there is a possibility of contralateral thrombosis, which often occurs asymptomatically. If the patient has symptoms of pulmonary embolism and there are no ultrasound signs of DVT in the main veins of the extremities, pelvis, and IVC, the gonadal, hepatic, and renal veins should be examined. An active search for DVT using ultrasound angioscanning seems appropriate in the preoperative period in patients at high risk of VTEC, as well as in cancer patients. In these same patients, it is advisable to conduct ultrasound angioscanning for screening purposes after surgery. When thrombosis spreads to the iliocaval segment, if it is impossible to determine its proximal border and nature according to duplex ultrasound scanning, radiopaque retrograde iliocavography or spiral computed tomography (CT) is indicated. During angiography, a number of therapeutic manipulations are possible: implantation of a vena cava filter, catheter thrombectomy, etc.
Prevention
To protect yourself from the onset or recurrence of the disease, it is recommended to follow some important rules:
- balance your diet and daily routine;
- get into the habit of spending at least 15-30 minutes for light exercise or jogging, without significant stress on your legs;
- give up all bad habits: alcoholism, smoking, drugs, etc.;
- consult a phlebologist or vascular surgeon at least once a year;
- fight all purulent and infectious diseases in a timely manner;
- avoid significant injuries, including blood vessels;
- strengthen the immune system;
- if there is a risk of relapse, use heparin-based ointment or aspirin prophylactically.
Preventive measures depend on the location of phlebitis. It is necessary to strictly follow the rules for intravenous infusions and injections, promptly treat pustular diseases, inflammatory processes and minor injuries. Patients with varicose veins of the lower extremities should follow the doctor's recommendations.