Materials and methods
Of the 16,839 patients included in the “Registry of Coronary Angiography Operations” [5] from 1998 to 2013, patients with stenosis of >75% of the lumen of at least one coronary artery, without acute or anamnestic myocardial infarction, without congenital and acquired heart defects: 75 patients with RV dilatation and 1134 without it. The transverse size of the pancreas in the parasternal position was 26 mm or less [6]. For a clearer division of the groups, patients with pancreatic dilatation included patients with a pancreatic size of 30 mm or more; patients with a slight enlargement of the pancreas (>26 and <30 mm) were not included in the study. A clinical, comprehensive echocardiographic examination was performed (one-dimensional, two-dimensional, Doppler echocardiography using Imagepoint NX ultrasound devices, Agilente Technologies, Phillips, USA; Vivid 3, 4, 7, 9 Systems, Vingmed-General Electric - Horten, Norway), determination of lipid composition of blood serum, Holter monitoring, selective coronary angiography according to Judkins (1967) (angiographic complexes Diagnost ARC A, Poly Diagnost C, Integris Allura, Phillips, Holland). Linear echocardiography (EchoCG) parameters were indexed to height; myocardial mass, calculated using the Devereux formula, to the body surface area [7]. Echocardiographic syndromes were diagnosed according to standard criteria: the LV was considered dilated when its end-diastolic diameter index was more than 32 mm/m2 in women and more than 33 mm/m2 in men [2], LV systolic function was reduced when the LV ejection fraction was less than 50%, hemodynamically significant mitral regurgitation (≥II degree) - with an effective area of the regurgitant orifice ≥0.2 cm2, regurgitant volume ≥30 ml [8].
Statistical processing of data was carried out using a package of applied statistical programs (SPSS Inc., version 17.0). Indicators are presented in the form M
±
SD
_
The distribution of variables was determined using the Kolmogorov–Smirnov test. To compare values with their normal distribution, t
; for a non-normal distribution, the nonparametric Mann-Whitney test was used.
When analyzing qualitative indicators, Pearson's χ2 test was used. Differences at p
<0.05 were assessed as statistically significant. Multivariate analysis was performed - binary logistic regression analysis with calculation of odds ratio (OR).
Clinical significance of minor cardiac anomalies in children
In recent years, much attention has been paid to connective tissue dysplasia (CTD) in children. DTD is understood as a congenital anomaly of the connective tissue structure of various organs and systems, which is based on a decrease in the content of certain types of collagen and/or a violation of their ratio, leading to a decrease in the strength of connective tissue [12, 13, 24, 26].
Endogenous (chromosomal and genetic defects) and exogenous (unfavorable environmental conditions, inadequate nutrition, stress) factors take part in the development of DST [12, 30, 43]. The peculiarity of connective tissue morphogenesis is that it participates in the formation of the heart frame at almost all stages of ontogenesis; therefore, the influence of any damaging factor can lead to the development of cardiac dystrophy [15].
In 1990, in the classification of diseases of the cardiovascular system of the New York Association of Cardiologists, as well as in Omsk, at a symposium dedicated to the problem of connective tissue dysplasia, the syndrome of cardiac dysplasia, accompanying both differentiated and undifferentiated dysplasia, was first identified. In case of DST syndrome of the heart, its connective tissue framework is involved in the pathological process - heart valves (atrioventricular, semilunar, Eustachian valve), subvalvular apparatus, heart septa and great vessels.
In clinical practice, when it comes to the morphological basis of changes in the cardiovascular system without hemodynamic disturbances, Yu. M. Belozerov (1993) and S. F. Gnusaev (1995) instead of the term “DST of the heart” proposed another one - “minor developmental anomalies heart" (MARS) [3, 8]. According to the definition of these authors, MARS are considered anatomical changes in the architecture of the heart and great vessels that do not lead to gross impairment of the functions of the cardiovascular system [9].
Classification of MARS according to S. F. Gnusaev, 2001 (as amended)
- Localization and form:
atria and interatrial septum: prolapsed valve of the inferior vena cava, enlarged Eustachian valve more than 1 cm, patent foramen ovale, small aneurysm of the interatrial septum, prolapsed pectineus muscles in the right atrium;tricuspid valve: displacement of the septal leaflet into the cavity of the right ventricle within 10 mm, dilatation of the right atrioventricular orifice, prolapse of the tricuspid valve;
pulmonary artery: dilatation of the pulmonary artery trunk, prolapse of the leaflets;
aorta: borderline narrow and wide aortic root, dilatation of the sinus of Valsalva, bicuspid aortic valve, asymmetry and prolapse of the aortic valve leaflets;
left ventricle: trabeculae (transverse, longitudinal, diagonal), small aneurysm of the interventricular septum;
mitral valve: mitral valve prolapse, ectopic attachment of chords, impaired distribution of chords of the anterior and (or) posterior leaflet, “fluttering” chords, additional and abnormally located papillary muscles.
- Complications and associated changes: infectious carditis, calcification, myxomatosis, fibrosis of valve leaflets, chordae ruptures, cardiac arrhythmias.
- Characteristics of hemodynamics: regurgitation, its degree, presence of circulatory failure, pulmonary hypertension.
There is still no consensus on the clinical significance of MARS, many of which are unstable due to the growth of the child. Thus, it is possible to reverse the development of an enlarged Eustachian valve, prolapsed pectineus muscles in the right atrium, mitral valve prolapse (MVP), closure of the open oval window, normalization of the length of the mitral valve chords and the diameter of the great vessels. In some cases, MARS change not only qualitatively, but also quantitatively [3]. Exceeding the established threshold level of cardiac stigmatization in healthy children (more than 3 MARS), according to S. F. Gnusaev (1995), indicates possible disadvantage both in relation to factors influencing the formation of health and indicators characterizing it [8].
Considering that MARS are a variant of visceral DST, children, as a rule, have a pronounced polymorphism of clinical and morphological disorders, depending on the degree of DST and the involvement of other organs and systems in the pathological process. An associative relationship has been identified between the number of external phenotypic markers of CTD and MARS [12, 16, 21, 22]. In this case, not only the number of external phenotypic markers matters, but also the “diagnostic weight” of each of them. It has been noted that skin and skeletal dysplasias are most often combined with MARS [12].
The clinical significance of connective tissue pathology in people with CTD is confirmed by data on the high frequency of neurovegetative disorders, changes in the central nervous system (enuresis, speech defects, vegetative-vascular dystonia (VSD)), and mental disorders [5, 12, 24]. As a rule, VSD is always detected in such patients, which is probably due to hereditary (hereditary) features of the structure and function of the limbic-reticular complex, which determine the abnormal nature of neurovegetative reactions [12]. E. V. Bulankina (2002) established a clear relationship between autonomic dysfunction and DST [4]. At the same time, the severity of dysplastic changes was combined with the severity of the processes of maladaptation of regulatory mechanisms and a decrease in the stress resistance of the body. The most common manifestations of autonomic dysfunction are cephalgia, autonomic crises, vegetative visceral paroxysms, pre- and syncope [12, 16]. According to the data of S.F. Gnusaev (1995), insufficiency of segmental autonomic structures was revealed in persons with MVP [8]. Research by T. M. Domnitskaya (2000) made it possible to establish a direct relationship between MVP, abnormally located trabeculae (ART) and the prevalence of neurotic (neurotic reactions, obsessive-compulsive neurosis, panic disorders) and encephalopathic (cerebrasthenic syndrome, stuttering, tics, sleep disorders, enuresis , hyperdynamic syndrome, fears) disorders [10].
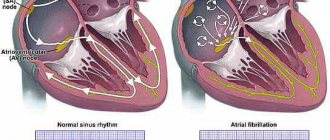
MARS is often accompanied by pathological conditions such as cardiac rhythm and conduction disorders, including early repolarization syndrome, sick sinus syndrome, Wolff–Parkinson–White syndrome, increased electrical activity of the left ventricle, right bundle branch block, extrasystole and paroxysmal tachycardia [ 4, 6, 8, 34]. According to L.A. Balykova et al. (2002), in 90% of patients with cardiac arrhythmias, MARS (mainly MVP) were identified using echography [2]. However, not all MARS are accompanied by heart rhythm disturbances and/or may be their cause. Arrhythmogenic MARS include fibromuscular abnormal chordae (APC) and ART, MVP and tricuspid valve prolapse (TVP), atrial septal aneurysm, enlarged and/or prolapsed Eustachian valve.
The presence of conducting cardiomyocytes in the fibromuscular ARH and ART forms additional conducting pathways, which explains the origin of the impulse that advances intraventricular conduction and causes early excitation of adjacent segments with subsequent earlier repolarization [12, 15, 19, 20, 28]. There is histological confirmation of the presence of conducting cells in the ART with diagonal-basal, mid-transverse and longitudinal localization and in the ART connecting the basal septal sections and the lateral wall of the left ventricle [3, 10, 33]. M. Suwa et al. (1986) noted an increase in the frequency of ventricular extrasystoles with increasing chord thickness. According to E. Chesler et al. (1983), the appearance of ventricular extrasystoles is associated with myxomatous changes in the chordae, causing mechanical irritation of the wall of the left ventricle [27]. The fact that ARX and ART are arrhythmogenic is also confirmed by the disappearance of extrasystoles in patients in the event of their independent rupture or surgical dissection, or during physical activity, when the degree of their tension decreases [8, 10, 12]. A fairly common cardiac arrhythmia in patients with ARH and ART is early ventricular excitation syndrome [6, 12].
Arrhythmias during MVP and PTC, according to various authors, occur in 15 to 90% of cases [11]. Among the causes of arrhythmias, autonomic dysfunction, mechanical stimulation of the endocardium, interstitial magnesium deficiency, psychological stress and myxomatous degeneration of valve leaflets are considered [3, 10–12, 18, 27, 29, 37, 39]. A direct correlation has been established between the frequency and severity of rhythm disturbances and the depth of MVP [1]. A number of authors believe that the cause of the development of arrhythmias in MVP and PTC may be turbulent flow resulting from regurgitation through the valve ring during ventricular systole, especially in PTC, when mechanical irritation of the sinus node area occurs [3, 8, 23]. Most researchers consider excessive tension of the papillary muscles due to their abnormal traction during prolapse of the leaflets as a possible mechanism for the development of ventricular extrasystoles in MVP [12, 14, 25, 38].
The development of arrhythmias can be provoked by a prolapsed Eustachian valve and an aneurysm of the interatrial septum: the conditions for the occurrence of arrhythmias arise as a result of their hilly movements and their reflex irritation of pacemaker formations in the right atrium [42].
According to studies by O. A. Dianov (1999), heart rhythm disturbances occurred in children with a borderline narrow aorta, in whom supraventricular and ventricular extrasystoles were recorded in 32.4% of cases and ventricular extrasystoles in 10.8%, indicating decompensation of adaptation, especially in conditions physical activity [4].
According to Yu. M. Belozerov, children with MARS are characterized by reduced cardiohemodynamic capabilities and demonstrate poor tolerance to physical activity [3]. According to N.A. Mazur, a connection has been established between MVP and sudden death syndrome in adults. Enough information has been accumulated that children with MARS are at risk for developing infective endocarditis.
Thus, existing research results indicate that MARS in some cases are the basis of cardiovascular pathology in children. At the same time, it would be unjustified to exaggerate their role in functional disorders of the cardiovascular system. Obviously, in each specific case the significance of structural abnormalities of the heart must be considered individually.
The principles of therapy for children with MARS have not yet been fully formulated. However, today we can propose the following tactics for the management of children with MARS:
- Comprehensive health assessment, including various types of examination of children.
- The choice of therapy depends on clinical, electrophysiological and echocardiographic changes.
- The use of drugs aimed at normalizing connective tissue metabolism.
- Determination of adequate physical activity depending on the functional state of the myocardium.
The use of non-drug treatment methods is generally accepted, including: - age-appropriate organization of work and rest;
- maintaining a daily routine;
- rational, balanced nutrition;
- psychotherapy and auto-training;
- water and balneotherapy;
- massage (manual, underwater, etc.);
- physiotherapy (electrophoresis with MgSO4, electrosleep, etc.);
- physical education classes, exercise therapy.
The issue of admission to sports is decided individually. In the presence of MVP, it is necessary to take into account family history (cases of sudden death in relatives), the presence of complaints of palpitations, cardialgia; syncope; changes on the ECG (heart rhythm disturbances, short and long QT syndrome) are the basis for deciding whether sports training is contraindicated. This also applies to the presence of ARCH, ART with early ventricular excitation syndrome, which, being arrhythmogenic MARS, can provoke cardiac arrhythmias in athletes under conditions of physical and psycho-emotional stress.
Drug treatment includes the use of:
- magnesium preparations;
- cardiotrophic therapy (in case of disruption of repolarization processes in the myocardium);
- antibacterial therapy for exacerbation of foci of infection, surgical interventions (prevention of infective endocarditis);
- antiarrhythmic drugs (according to indications, with pure group extrasystole with impaired repolarization processes).
Currently, therapy with magnesium preparations for MARS is approaching pathogenetic. This is due to the fact that magnesium is part of the main substance of connective tissue and is necessary for the proper formation of collagen fibers. Under conditions of magnesium deficiency, the ability of fibroblasts to produce collagen is impaired [29, 31]. In addition, magnesium has a membrane-stabilizing effect, retains potassium inside the cell, and prevents sympathicotonic effects, which makes it possible to use it for the treatment of cardiac arrhythmias [40, 41].
In the works of O. B. Stepura (1999), O. D. Ostroumova et al. (2004) there is information about a significant decrease in the degree of MVP, symptoms of VSD, and the number of ventricular extrasystoles during therapy with magnesium drugs [17, 18].
The following medications may be considered appropriate:
Magnerot containing magnesium salt and orotic acid. The latter not only enhances the reabsorption of Mg in the intestine, but also has an independent metabolic effect. Children are prescribed 500 mg of Magnerot (32.8 mg of magnesium 3 times a day for 1 week, then 250 mg 3 times a day for the next 5 weeks. The drug is taken 1 hour before meals).
Magne B6. Available in tablets (48 mg magnesium or in oral solution (100 mg magnesium). Children weighing more than 10 kg (over 1 year) - 5-10 mg/kg/day in 2-3 doses. Children over 12 years old — 3–4 tablets per day, in 2–3 doses, course duration 6–8 weeks.
Potassium orotate. For children, the drug is prescribed at a rate of 10–20 mg/kg/day in 2–3 doses, 1 hour before meals or 4 hours after meals. Course duration - 1 month.
Repeated courses of therapy with these drugs should be carried out (3-4 times a year).
To improve the cellular energy of the myocardium, drugs are used that have a complex effect on metabolic processes in the body, and are also active antioxidants and membrane stabilizers:
- L-carnitine (elkar - 20% solution of carnitine hydrochloride). Doses: 1–6 years, 0.1 g/day (14 drops) 3 times a day; 6–12 years – 0.2–0.3 g/day (1/4 tsp) 3 times a day. Course - 1–1.5 months.
- Coenzyme Q10 (ubiquinone) is prescribed to children over 12 years of age, 1 capsule (500 mg) 1–2 times a day. Preparations containing ubiquinone include kudesan: 1 drop per year of life (up to 12 years), then 12 drops 1 time per day. The duration of the course must be at least 1 month.
- Cytochrome C (cyto-mac). Available in ampoules (4 ml = 15 mg). Prescribed intramuscularly, 4 ml, No. 10. 2–4 courses are given per year.
In addition to these drugs, to improve metabolic processes in connective tissue, myocardium and the body as a whole, the use of:
- nicotinamide (vitamin PP) - 20 mg/day for 1.5–2 months;
- riboflavin (vitamin B2) - 10–15 mg/day for 1.5–2 months;
- thiamine (vitamin B1) - 10 mg/day and lipoic acid 100–500 mg/day for 1.5 months;
- limontara (complex of citric and succinic acid) 5 mg/kg/day 3–4 days weekly for 2 months;
- biotin - 2-5 mg/day - 1.5-2 months.
Repeated courses of treatment are indicated (up to 3 times a year).
In the presence of VSD, complex long-term therapy is carried out to restore the balance between the sympathetic and parasympathetic parts of the autonomic nervous system (differentiated herbal medicine, vegetotropic drugs, nootropics, vasoactive drugs - Cavinton, Vasobral, Instenon, cinnarizine, etc.).
Thus, all of the above allows us to conclude that MARS, being a visceral manifestation of connective tissue dysplasia, constitute the morphological basis of functional changes in cardiac activity and neurovegetative disorders. Choosing an individual course of treatment program helps improve metabolic processes in connective tissue and prevents possible complications of CTD in children and adolescents.
For questions regarding literature, please contact the editor.
N. A. Korovina , Doctor of Medical Sciences, Professor A. A. Tarasova, Candidate of Medical Sciences, Associate Professor T. M. Tvorogova, Candidate of Medical Sciences, Associate Professor L. P. Gavryushova, Candidate of Medical Sciences, Associate Professor M. S. Dzis RMAPO , Moscow
results
The majority in both groups were men, but in contrast to the group of patients with normal pancreatic size, men were more common in the group with pancreatic dilatation. Patients in this group showed a tendency toward older age (Table 1).
Table 1. Comparative characteristics of clinical, functional and laboratory parameters of patients with coronary artery disease without myocardial infarction, depending on the presence of pancreatic dilatation Note. Here and in the table. 2: data are presented as mean ± standard deviation or number of patients (in%). SBP—systolic blood pressure; DBP—diastolic blood pressure; FC - functional class; NYHA - New York Heart Association; nd - statistically insignificant differences.
The groups did not differ in the frequency of smoking, alcohol consumption, levels of SBP and DBP, the frequency of detection of arterial hypertension, diabetes mellitus, hypothyroidism and heredity burdened with ischemic heart disease. The average BMI in both groups corresponded to obesity, but in patients with a dilated pancreas it was statistically significantly higher. Patients with RV dilatation more often demonstrated a higher (III) FC of CHF according to the New York Heart Association (NYHA) classification, as well as NRPS with less frequently detected severe (III-IV) FC of exertional angina. There were no intergroup differences in basic laboratory parameters and coronary angiography data. When analyzing EchoCG parameters in patients with dilated RV, higher indices of the linear dimensions of the heart and LV myocardial mass were revealed with no statistically significantly different index of the thickness of the interventricular septum and a tendency towards a lower index of thickness of the posterior wall of the LV. The groups did not differ in the LV asynergia index; the LV ejection fraction was lower in the group with an enlarged RV. Dilatation of the left ventricle, a decrease in its contractility, as well as significant mitral regurgitation and signs of atherosclerotic lesions of the aorta were more often detected in patients with dilatation of the right ventricle (Table 2).
Table 2. Comparative characteristics of echocardio-, electrocardio- and angiographic parameters of patients with coronary artery disease without myocardial infarction, depending on the presence of RV dilatation Note. * — degree of coronary lumen stenosis >75%.
According to the results of multivariate analysis, an independent relationship with RV dilatation was demonstrated by a decrease in myocardial contractility, male gender, NRPS, significant mitral regurgitation, an increase in the FC of CHF and BMI, as well as a decrease in the FC of angina pectoris (Table 3).
Table 3. Parameters independently associated with pancreatic dilatation in patients with coronary artery disease without myocardial infarction
The pandemic has managed to push aside many of the most important problems of our health. Even the eternal leaders - cardiovascular diseases - are perceived without their usual relevance. But pandemics, I want to believe, end sooner or later. Are heart and vascular diseases our eternal companions? Today we are talking about them with the chief cardiologist of four regions of Russia, General Director of the National Medical Research Center for Cardiology of the Russian Ministry of Health, Academician of the Russian Academy of Sciences Sergei Boytsov.
Sergey Anatolyevich! You run the world-famous center, which is usually called Chazovsky. For the simple reason that an outstanding cardiologist, the chief Kremlin physician, Academician Yevgeny Chazov, created this center and led it for many years. Within its walls a unique team of the best representatives of Russian cardiology has gathered. Do you think that repurposing a center of such a level as yours for Covid was justified?
Sergey Boytsov: At that time, I think yes. Our center was one of the first federal centers repurposed as a Covid hospital. A “red zone” was created and more than 300 beds were used.
There are a total of 400 beds in the center. It turns out that almost everything was given over to the virus?
Sergey Boytsov: All beds that have oxygen supply.
And those who were tormented by heart pain? Who urgently needed operations on the heart and blood vessels?..
Sergey Boytsov: You may be surprised by my answer. But it is true. And, by the way, this applies not only to Russia. Around the world, at the beginning of the pandemic, there was a noticeable reduction in people seeking emergency care for cardiovascular diseases. Cause? It is obvious: people’s fear of getting infected has become paramount. The fear of the virus turned out to be stronger than the heartache.
And in fact?
Sergey Boytsov: In fact, they didn’t leave. And if the condition was very serious, then people asked for help. And Moscow had the opportunity to provide it in a timely manner. If I can use the podium of Rossiyskaya Gazeta, I would like to not just say thank you, but express my admiration for the work of the Moscow ambulance.
How long was Chazovsky a Covid center?
Sergey Boytsov: Two months. At the very peak of the first wave. During this time, 759 people received help in our center.
For men, the critically dangerous waistline is 102 cm. For women, 88 cm. Belly fat is the most dangerous for the cardiovascular system. Do you insist on the accuracy of these numbers?
Sergey Boytsov: I insist. In our digital times, it is impossible to do otherwise.
Notice that you said about digital time. Are modern technologies and digital technology incorporated into the Chazovsky Center? I ask this question not by chance. Sometimes doctors, and not only them, are accused of being old-fashioned, of insufficient use of the latest technologies in practice, and so on...
Sergey Boytsov: Medicine, healing without preserving and respecting traditions is unthinkable. But we cannot do without moving forward, without using the latest technologies. And the Chazovsky Center has a tradition: as soon as something new, and especially revolutionary, appeared somewhere in the world, it invariably became the real practice of our center. The same medical information system was created in our country at the beginning of the 2000s. All endovascular technologies, cardiac surgical technologies for cardiac arrhythmias, resuscitation aids are all digital technologies, which are coupled with manual skills.
Your center is federal. Which Russians have the right to receive assistance under the compulsory medical insurance system?
Sergey Boytsov: More than half of our patients are not Muscovites, but residents of other regions of the country.
Sergey Anatolyevich! In addition to leading the Chazovsky Center, you are also the chief cardiologist of Russia in four federal districts. The rest are commanded by your colleague from St. Petersburg, academician Evgeniy Shlyakhto. And if the patient is not from the region under your jurisdiction, but wants to get help in your center, what should you do? Does the patient have the right to choose the place of treatment and the doctor with whom he wants to be treated?
Sergey Boytsov: Definitely yes! Yes Yes! Has the right to. And he should have such an opportunity. Moreover, he has it.
Are you sure about that? Then why do applicants for help often turn to me with just such requests?
Sergey Boytsov: This may be the result of the patient’s ignorance of their rights or the slowness of local health authorities.
Let's say, I want academician Renat Suleymanovich Akchurin to operate on me? I live and am registered in Moscow. What should I do to get to Chazovsky, specifically to the operating table with Renat Suleymanovich?
Sergey Boytsov: You need to get a referral from the district clinic for a consultation to our center. True, the most difficult and complex cases are usually referred to us. That's probably how it should be.
I don't agree with you! In theory, you're probably right. But for the patient, his disease is the most complex, the most severe. And he has the right to count on the best help...
Sergey Boytsov: But I can’t agree with you either! I affirm: in recent years, the level of provision of cardiac and cardiac surgery care has increased in the country. This is a given that cannot be discounted. If you don’t mind, I’ll give you some addresses of such centers. They are in St. Petersburg, Novosibirsk, Krasnodar, Tomsk, Krasnoyarsk, Nizhny Novgorod, Penza, Astrakhan, Yekaterinburg...
Aren't you afraid that Chazovsky is losing his relevance?
Sergey Boytsov: On the contrary, it makes us happy and keeps us on our toes. For example, previously hybrid cardiac surgery was the property of only some clinics. Now it becomes a practice. It is now used in a number of centers for the most severe and complex cases. At our center, we conduct special educational courses that teach the latest technologies.
What does it mean to lead such an institution? Is Chazovsky at a decent level today?
Sergey Boytsov : To be honest: leading is very difficult and very responsible. It helps that before this director’s chair I went through the school of Evgeniy Ivanovich himself - I was his deputy for five years.
The optimal pressure with which you can live normally is less than 140 over 90. And it is better to strive for a pressure of 130 over 80 or even lower. This is the deadline. Moreover, I know how scrupulous Evgeniy Ivanovich himself was always in choosing personnel. It probably also helped you that you have the Leningrad Military Medical Academy, the Pirogov Medical Center and the National Center for Preventive Medicine behind you. By the way, this center was created by Evgeny Ivanovich. So the path upward - to the current center, one might say, was predetermined. And still . Sergey Anatolyevich, how to work with a team that is almost entirely made up of stars of Russian cardiology and cardiac surgery?
Sergey Boytsov: First of all, you need to match him. And help. So that colleagues have the opportunity to realize their scientific, clinical, and pedagogical plans.
Is it possible? To be honest again: are you loved in the team or?..
Sergey Boytsov: About love... Somehow I didn’t think about it. But in almost four years of working with the team, I have had no conflicts, thank God. But there is already a common history. Including passing the Covid test.
Key question Evgeny Ivanovich Chazov is invariably associated with the so-called Kremlin medicine. The Kremlin’s postulates are indeed very effective and justified: prevention, availability of assistance, high level of provision, and so on. Although, out of spite, they sometimes talked about it: parquet floors, doctors’ questionnaires. But by and large: all the best doctors had a place to be in Kremlin medicine. Although sometimes they were officially registered in completely different medical institutions. But the principles of providing assistance themselves, I think, were the best.
Sergey Boytsov: I absolutely agree with you. But you did not mention one, and, in my opinion, the main quality of this service: an individual approach to each patient. Fidelity to the eternal postulate: it is not the disease that must be treated, but the patient. And this is necessary in the age of digital medicine. Now the terminologies themselves are changing somewhat. They talk about a personalized approach based on the principles of evidence-based medicine. But in fact, this is the same rule that, in my opinion, will never become outdated: treat not the disease, but the patient.
Especially when it concerns the heart and blood vessels, when, according to you, cardiologists, almost by the age of 35-45, most of us begin to have all sorts of cardiovascular problems. All over the world they take precedence among all ailments. This was the case even when there was no covid. So, apparently - at least in the foreseeable future - it will be after it.
Sergey Boytsov: Most likely, that’s exactly it. The population is aging. And that's a plus. But with age, the blood vessels begin to suffer first. Arterial hypertension manifests itself. And since we are talking about numbers today, I will refer to them again. Between the ages of 25 and 65 years, 48% of men are affected by hypertension. There are slightly fewer women. And among those over 65+, hypertension reaches 70-80-90%. It is the main, main culprit of heart attacks, strokes, and premature deaths.
But for some reason, the same hypertension does not cause, for example, such fear in us as Covid. A lady I know weighing 140 kilograms just can’t deny herself the pleasure of eating another piece of cake. She reported that in recent weeks her working blood pressure has remained at 160 over 100. And she feels fine.
Sergey Boytsov: Allow me a tiny educational lesson? In medicine there is no concept of “working blood pressure” at all. And 160 to 100 practically excludes the possibility of feeling normal.
Since it’s educational and numbers, then name the optimal ones with which you can live without fear of a heart attack or stroke.
Sergey Boytsov: Less than 140 over 90. It’s better to strive for a pressure of 130 over 80 or even lower.
You will not recommend medications. Nowhere in the world is there an optimal treatment for hypertension. Let’s say I completed a course of taking them and got rid of her high numbers...
Sergey Boytsov: I won’t. Hypertension is a chronic disease. It is impossible to completely get rid of it. But you can, by taking the medications prescribed by a specialist specifically for you, keep the disease under control and maintain a high quality of life. This is not one or two courses of therapy. This, I’ll disappoint you, often lasts for the rest of your life. The drugs themselves vary depending on the condition, age, and time of year. That is, I repeat once again: in our digital time, the time of the onset of artificial intelligence, we need to treat not the disease, but the patient.
I think not only now, but throughout everything, including post-Covid times.
By the way
Recipe from an academician
1. Get a flat stomach. To do this, you can look in the mirror, or you can use a measuring tape. For men, the critically dangerous waist width is 102 cm or more. For women - 88 cm and more. Belly fat is the most dangerous for the cardiovascular system.
2. Physical activity is necessary. Working muscles is a proven remedy against hypertension.
3. Don't overuse salt. Try not to add enough salt to your food when cooking. Try to remove the salt shaker from the table so as not to spill salt into prepared dishes.
4. Stop smoking. Including from electronic cigarettes.
5. Less alcohol. There are no useful doses of it.
Source: https://rg.ru/
Discussion
It is known that ventricular dilatation after MI is more pronounced in patients with a larger area of LV myocardial damage [9]. Therefore, in patients with coronary artery disease, one can expect to find a connection between RV dilatation and multiple coronary stenoses or with a larger size of LV asynergia. RV MI often develops as a result of damage to the proximal part of the non-dominant right coronary artery [10, 11], so RV dilatation in our patients could be associated with damage to this localization in the left type of coronary circulation. However, there were no intergroup differences in the type of coronary circulation, the prevalence or localization of coronary lesions, and the LV asynergia index. The negative relationship between right ventricular dilatation and the FC of angina pectoris necessitates further study.
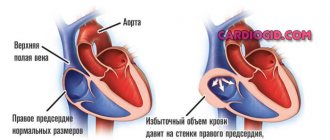
An increase in the size of the pancreas in patients with coronary artery disease can serve as a sign of increased pulmonary vascular resistance and load on the pancreas, determined by the condition of the left chambers of the heart [2]. Left ventricular dysfunction, causing postcapillary pulmonary hypertension, is the most common cause of right ventricular dilatation [8]. In the present study, LV systolic dysfunction was observed in 25% of patients with dilated RV, and it was the strongest predictor of RV enlargement in multivariate analysis.
The risk of RV dilatation also increased with NRPS, significant mitral regurgitation and with an increase in the FC of CHF - the same as in patients with MI [3].
Among the factors associated with RV dilatation and not related to the LV condition were male gender and an increase in BMI (the same connections were found in patients with MI [3]). The fact is that obese patients often develop obstructive sleep apnea syndrome due to hypoventilation and hypercapnia, accompanied by the development of pulmonary hypertension and, as a consequence, pancreatic dilatation [12]. Perhaps it is this factor that explains the connection between pancreatic dilatation and obesity.
A limitation of this study was that the only parameter of the pancreas was analyzed - its transverse size in the parasternal position. This is explained by the fact that the collection of data for the Register began in 1998, when not all patients had other indicators characterizing the structure and function of the pancreas. The point of our study is to use a large amount of material to study the general patterns of the course of IHD, in particular the factors associated with pancreatic dilatation in a specific population. Inclusion in the analysis only of patients with a complete set of pancreatic characteristics would significantly reduce the sample and would not allow obtaining the most reliable result. Thus, limitations of the study stem from its retrospective nature. Since P.Zh. is a chamber that is extremely sensitive to changes in afterload, and the assessment of the size of the pancreas is an integral part of the characteristics of its function [13], we consider it possible to judge the state of the pancreas by assessing its linear size alone.
Left ventricular diastolic dysfunction
Ultrasound diagnostics doctor Paliy K.A.
Diastolic dysfunction to the inability of the left ventricle to fill and maintain stroke volume without a compensatory increase in atrial filling pressure.
To a large extent, it is determined by the ability of the myocardium to relax and the compliance (rigidity) of the wall. Impaired diastolic function of the left ventricle can be observed both in combination with a decrease in systolic function of the left ventricle, and in isolation (for example, in diseases accompanied by left ventricular hypertrophy). Increased myocardial fibrosis that develops with aging can also cause significant diastolic dysfunction.
Understanding approaches to assessing left ventricular diastolic filling requires knowledge of the four phases of diastole.
- Isovolumic relaxation phase. Diastole begins with the onset of relaxation of the left ventricle, which is marked by the closure of the aortic valve. During the initial period of relaxation, the pressure in the left ventricle decreases rapidly, but until it falls below the pressure in the left atrium, the mitral valve remains closed. Thus, during this phase of diastole, the aortic and mitral valves remain closed, so the volume of the left ventricular cavity does not change.
- Rapid early filling phase. The next period of diastole begins after the pressure in the left ventricle falls below the pressure in the left atrium, allowing the mitral valve to open. In this case, blood begins to flow passively (i.e., according to the pressure gradient) from the left atrium into the left ventricle. Typically, during this phase of diastole, the main filling of the left ventricle occurs (if we mean by this the volume of incoming blood and the speed of the transmitral flow).
- Slow filling phase (diastasis). During this phase, the pressure gradient between the left atrium and the left ventricle is minimal, so slow passive filling of the left ventricle occurs until it finally disappears.
- Late filling phase. During this final phase of diastole, the left atrium contracts, causing additional blood volume to be actively “pushed” into the left ventricle through the opening of the mitral valve. Normally, during this period, 20–30% of the total diastolic filling volume enters the left ventricle.
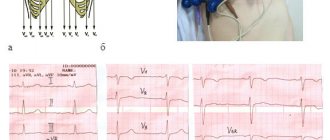
The above-described phases of diastole can be easily traced using pulsed wave Dopplerography, which visualizes changes in the speed of transmitral blood flow.
A typical transmitral flow velocity curve has two peaks: the first (peak E) corresponds to the rapid early ventricular filling phase, while the second relatively low-velocity peak (A) has a lower amplitude and coincides in time with atrial contraction. To assess left ventricular diastolic function, it has been proposed to use a large number of characteristics of the E and A peaks, but in practice only a few of them are routinely used: the maximum velocity of the E peak, the maximum velocity of the A peak, the ratio of the maximum E/A velocities and the deceleration time of the E peak.
As the diastolic function of the left ventricle is impaired, the end-diastolic pressure in its cavity begins to increase, which, in turn, causes an increase in pressure in the left atrium. As a result, the nature of the blood flow between the left atrium and the left ventricle changes, which can be recorded using pulsed wave Dopplerography of the incoming transmitral flow.
There are 4 main types of diastolic filling of the left ventricle:
- Normal. The volume and rate of early filling prevails over those during atrial systole (E>A).
- Impaired relaxation (Type 1 disorder of diastolic dysfunction). Impaired relaxation of the left ventricle leads to difficulty in the outflow of blood from the left atrium. Therefore, the volume and rate of early passive filling are reduced, and the maximum velocity of the E peak is reduced. In this case, left ventricular filling naturally becomes more and more dependent on atrial contraction at the end of diastole, and peak A (E<A) begins to dominate on the transmitral molasses velocity curve.
Violation of the diastolic function of the ventricle according to the first type can be a variant of the norm in older people, and occurs in people with arterial hypertension, angina pectoris, myocardial infarction, and myocarditis.
- Pseudonormal filling type (Second type). More severe left ventricular dysfunction results in an even greater increase in left atrial pressure, which is accompanied by an increase in the rate of early diastolic filling of the left ventricle. Therefore, the Doppler curve is again dominated by peak E (E>A), as with normal filling.
- Restrictive type of filling (Third type). In particularly severe cases, the pressure in the left atrium may be so high that filling of the left ventricle occurs almost completely in the early phase, and during other phases of diastole there is virtually no filling. Due to the fact that in such a situation the pressure in the left ventricle increases much faster as it fills, transmitral blood flow quickly stops. The maximum speed of peak E is much higher than the maximum speed of peak A (E>>A). This type of transmitral flow may be seen with restrictive cardiomyopathy (in which left ventricular systolic function is relatively high) or concomitantly with severe left ventricular systolic dysfunction due to other causes.
Factors influencing changes in transmitral blood flow can be divided into physiological and pathological. In turn, pathological ones are divided into extracardiac and cardiac.
Physiological causes include age, heart rate, patient position, breathing, preload (for example, changes in transmitral blood flow profile during exercise tests).
Extracardiac factors affecting transmitral blood flow: obesity, diabetes, renal failure, sleep apnea syndrome.
Cardiac causes: arterial hypertension (AH), coronary heart disease (CHD), cardiomyopathies, chronic heart failure (CHF), heart defects, myocarditis, pericardial diseases, etc.
Thus, echocardiography is the only available noninvasive method for assessing left ventricular diastolic function, which has important clinical implications.
Diastolic dysfunction is considered to be the onset of ventricular dysfunction in various heart diseases.
The degree of diastolic dysfunction may indicate the severity of the disease in patients with the same degree of systolic dysfunction.
The severity of diastolic dysfunction can act as an objective marker of the effectiveness of treatment or the course of the disease.
Riding E. Echocardiography. Practical Guide / Elisdair Riding; lane from English – 4th ed. – M.: MEDpress-inform, 2021. – 280 p.
Rybakova M.K. Practical guide to ultrasound diagnostics. Echocardiography / M.K. Rybakova and others - M.: Vidar-M Publishing House. 2008. – 512 p.