Conduction dysfunction (blockades) hearts - this is a slowdown or complete cessation of the conduction of impulses through any part of the conduction system.
In this case, there is a violation of the sequence, speed and strength of excitation and contraction of the heart, or there is no contraction of a certain area of the heart.
Based on the degree of conduction disturbance in an element of the conduction system of the heart, the following are distinguished:
- incomplete (partial) blockade – impulse conduction is slowed down;
- complete blockade - there is no impulse conduction.
Causes of heart failure
The lecture of every expert in the field of cardiology begins with cardiac arrhythmia and conduction disorders. First of all, it is important to analyze the reasons for the development of the pathological condition. There are the following unfavorable factors that provoke the disease:
- Cardiological (ischemic heart disease, myocardial infarction, angina pectoris, congenital and acquired heart defects, myocardial abnormalities, prolapses);
- Pharmacological influence (taking glycosides, antiarrhythmic drugs, diuretics, sympatholytics);
- Electrolyte type failure (hyperglycemia, hypercalcemia, etc.);
- Toxic substances (smoking, drug, alcohol addiction, poisoning with one’s own hormonal substances).
2. Reasons
A coordinated, step-by-step, normally having a clear rhythm - the cycle of contraction of the heart muscle is ensured by the special bioelectric properties of muscle cells - cardiomyocytes. However, any pulsation must be set by some kind of generator or pendulum. The role of such a pacemaker (literally, “setting the step”, “setting the pace”) generator in the heart contraction system is performed by the so-called. The sinoatrial node (more often called simply the sinus node) is a collection of cells in the upper part of the right atrium, where the initial impulse is formed, which triggers the next cycle of cardiac contraction in a strictly defined sequence. Excitation from the initial signal propagates along three main pathways (Bohmann's bundle, Wenckenbach's and Thorell's pathways). Disturbances in the process of generating a pacemaker impulse, as well as difficulties or impossibility of its normal propagation along the conduction pathways inevitably lead to arrhythmia, etc. heart blockade (atrioventricular, intraventricular, dysfunction of ion channels, etc.). The cause of conduction disturbances and/or initial impulse generation can be almost any congenital developmental anomalies and acquired heart diseases. Risk factors also include:
- electrolyte imbalance (especially deficiency of potassium and magnesium ions);
- hormonal imbalances (especially thyroid dysfunction);
- lack of oxygen (hypoxia);
- poisoning by certain groups of substances (including alcohol, nicotine, caffeine, etc.);
- long-term use of certain medications.
Visit our Cardiology page
Types of cardiac conduction disorders
Arrhythmias are divided into the following categories:
- Impaired automaticity (sinus arrhythmia, tachycardia, bradycardia);
- Heart rhythm disturbances (ventricular extrasystole, paroxysmal tachycardia, sick sinus syndrome);
- Failure in the conduction program (increase or decrease in blockade);
- Mixed species.
Considering exactly where the failure occurs, heart rhythm disturbances are divided into atrial (supraventricular) and ventricular. Tachycardia is a heart rhythm disorder that is manifested by an increase in heart rate (more than 90 beats/min). Bradycardia is the opposite condition when the heart rate decreases to 55 beats or less.
What is cardiac conduction
The heart has a complex structure, consisting of many departments, the work of which is interconnected.
For example, an electronic impulse occurs in the sinus node. It goes to cardiomyocytes. Their conductive capacity is determined by the ability of muscle cells to respond to an incoming impulse. The signal generated in the sinus node passes through a number of structural divisions, causing excitation in the atria and ventricles. The essence of this complex process is to push blood flow from the heart muscle into the aorta and further throughout the body. The impulse can be delayed at any point along its path, thereby causing a violation of the intraventricular conduction of the heart - that’s what it is. We tried to present the essence of the problem briefly and in an accessible form. If we succeed, then we can move on.
Symptoms
Considering each specific heart rhythm disorder, the symptoms should also be studied taking into account a certain deviation. Common complaints made by patients:
- Feeling of a hard or fast beating heart;
- Headache;
- Discomfort behind the sternum;
- Fainting;
- Blueness of the nasolabial triangle;
- Pale dermal tissue;
- Severe shortness of breath;
- Inexplicable feeling of anxiety;
- Partial or complete disorientation in space and time.
With tachycardia, the child feels a “heavy heart”, he is too overexcited against the background of general weakness, and there is a strong feeling of chest compression. With bradycardia, patients are more prone to fainting. Severe dizziness, severe cephalalgia, the patient's skin becomes sticky from cold sweat.
What symptoms should you look out for?
Usually, a violation of intraventricular conduction does not manifest itself in any way if it is a block of the right leg or one of the branches of the left is blocked. In cases of two- or three-bundle block, symptoms occur more often, but they are caused by the underlying cardiac pathology. This could be pain in the heart area, interruptions in heart function, increased blood pressure, etc.
Symptoms of blockades themselves occur in the case of a rare heartbeat (less than 50 per minute) and are expressed in the form of dizziness, flashing spots before the eyes, severe general weakness, lightheadedness or loss of consciousness. These symptoms are regarded as equivalents or attacks of MES (Morgagni-Edens-Stokes). They occur due to a sharp decrease in blood flow to the brain. Such symptoms require immediate medical attention. Remember! A rare pulse combined with loss of consciousness requires treatment in a cardiology or therapeutic hospital!
Diagnostic measures
The arrhythmia may disappear on its own. Minor disturbances in heart rhythm and conduction do not require emergency care. If failures occur too often and bother the patient for a long time, you should immediately seek help.
Diagnosis of heart rhythm and conduction disorders is based on the use of the following diagnostic techniques:
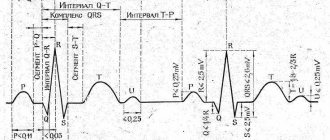
- Electrocardiography is the main way to thoroughly study the characteristics of the heart rhythm;
- ECG monitoring – recording of heart function for 24 hours on magnetic media;
- Echocadiography is used as an additional diagnostic method.
Diagnostics
- analysis of life history (past diseases and operations, bad habits, lifestyle, level of work and living) and heredity (presence of heart disease in close relatives);
- Indicators of general and biochemical analysis of blood and urine, analysis of hormonal status (hormone levels) - can identify extracardiac (not related to heart disease) causes of the blockade;
- Electrocardiography (ECG) data – allows you to identify changes characteristic of each type of blockade;
- Indicators of daily ECG monitoring (Holter monitoring) - a diagnostic procedure that involves the patient wearing a portable ECG device throughout the day. At the same time, a diary is kept in which all the patient’s actions are recorded (getting up, eating, physical activity, emotional anxiety, deterioration in health, going to bed, waking up at night). ECG and diary data are compared, thus identifying intermittent cardiac conduction disturbances (associated with physical activity, food intake, stress, or night blockades);
- Echocardiography data - EchoCG (ultrasound examination of the heart) - allows you to identify cardiac causes of blockades (heart disease leading to impaired cardiac conduction);
- The results of stress tests - recording an ECG during and after physical activity (squats, walking on a treadmill or exercising on an exercise bike) - allow you to identify blockade that occurs during physical activity, determine the heart's response to stress, and exclude myocardial ischemia (insufficient blood supply and oxygen starvation of the heart). muscles);
Heart rhythm disturbances: treatment of arrhythmia
Treatment of most types of arrhythmias is aimed at eliminating the underlying disease that provoked the occurrence of systematic failures. Some conduction and rhythm disorders can be eliminated by adhering to a healthy lifestyle: eating right, giving up any strong alcoholic drinks and nicotine, playing sports, avoiding stress and psycho-emotional tension.
If necessary, the attending physician will prescribe medication. For patients with tachycardia, topical pharmacological products from the group of beta blockers, calcium channel blockers, cardiac glycosides. To generally stabilize the patient’s emotional state, sedatives are prescribed.
In some cases, patients are indicated for surgical intervention. The pacemaker is a pacemaker and helps to correct the functioning of the organ in such serious conditions as AV blockade, severe bradycardia that is not amenable to medication, and sick sinus syndrome. The treatment regimen is always selected strictly individually, taking into account the characteristics and needs of each patient.
How does the conduction system in the heart work?
The histological structure and structure of the cells that provide conductivity make it possible to distinguish them into a special type, indicating an affinity for myocardial elements and the nervous system. Transport fibers consist of intensively innervated cardiomyocytes with a reduced number of myofibrils.
The transfer of excitation from one cell to another is ensured by an electrophysiological mechanism
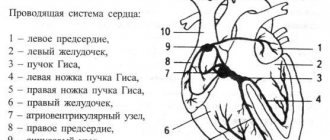
The whole system is divided into 2 parts:
- sinoatrial (sinoatrial);
- atrioventricular (atrioventricular).
The sinoatrial section includes:
- sinus node (Kisa-Flyaka node) - located in the right atrium near the mouth of the vena cava, therefore it is also called the sinoatrial or pacemaker, since it is in it that the normal impulse originates to ensure the correct rhythmic contraction of all chambers of the heart;
- three internodal bundles for quick connection of the sinus node with the atrioventricular one;
- interatrial tract connecting the main node with the left atrium.
Transport of information between nodes occurs along bundles:
- Bakhmana - to the left atrium;
- Wenckebach - to the atrioventricular node along a branch of medium length;
- Torella - in the same direction, but along a longer path along the back surface.
To this day, there remains debate among cardiologists about the role of these tracts in the conduction system. The presence of additional paths is shown. Some scientists believe that they, together with the Torell beam, are spare and are connected only in emergency cases.
Both the sympathetic and parasympathetic nervous systems contact the node.
The parasympathetic nervous system has the maximum influence through the vagus nerve on the sinus and atrioventricular nodes
The atrioventricular part includes the following elements.
Atrioventricular node (Ashof-Tavara) - lies in the lower part of the interatrial septum. It differs in structure from sinus:
- a lower content of pacemaker cells, which provide excitability, and a higher content of transport cells;
- is divided by collagen layers into longitudinal structures (α slow and β fast channels), they are the anatomical basis of conductivity dissociation, create conditions for impulse conduction in both directions, they are called anterograde and retrograde;
- the structure creates the possibility for the occurrence of paroxysms of nodal tachycardia;
- has mainly the endings of parasympathetic nerve fibers, through which it participates in the process of slowing down the heart rate.
The bundle of His, consisting of a common trunk and three branches (the left one is further divided into posterior and anterior), receives innervation from the parasympathetic nodes.
Purkinje fibers - directly come into contact with cardiomyocytes and transmit excitation with the requirement to contract; they have no connection with nerve endings.
The impulse speed in the trunk of the His bundle is about 1.5 m/s, in the interventricular zone of the branching of the branches of the His bundle it increases to 4 m/s, in the terminal Purkinje fibers it decreases significantly and reaches 1 m/s.
Passing through the myocardium of the atria and ventricles, excitation reduces the speed to 0.8 and 0.4 m/s. Such a small rate of propagation in the atrioventricular node provides physiological protection against the entry of a large number of impulses and reduces the conditions for ventricular arrhythmias.