Cardiac diseases are not always detected by routine methods. Especially functional, in the early stages of their development. Long-term follow-up is required, which apparently healthy patients do not receive.
Slowing of intraatrial conduction is a clinical variant of the disorder in which the intensity of the electrical impulse from the natural pacemaker to the atria weakens.
As it progresses, the entire organ, including the ventricles, becomes involved in the pathological process.
The main and immediate cause is the death of the structures of the sinus (SA) node, which precisely forms the very signal necessary for myocardial contraction.
Treatment has different prospects. Secondary forms (caused by non-cardiac diseases), provided that the main factor of formation is eliminated, are completely stopped.
Cardiogenic diseases cannot be eradicated, but there are good opportunities to slow down and even stop the progression, relieve symptoms and equalize the patient’s chances of life with other people who do not have cardiac pathologies.
Development mechanism
Slowing of impulse conduction through the atria is a consequence of the death of cells of the sinoatrial or sinus node.
As a result of insufficiently intense production of the bioelectric impulse, weak activity of the myocardium itself is observed. First, only the atria, then the ventricles and the entire muscular organ as a whole suffer.
Read more about intraventricular conduction disorders here.
Up to a certain point, violations are not visible at all; information about the deviation is provided only by electrocardiography, if you look closely.
As it progresses, bradycardia (slow heart rate) develops. The natural pacemaker produces an insufficiently strong signal, and after reaching a critical cell level, threatening consequences develop. The probability of cardiac arrest increases to 70%; only transplantation can save the patient.
The contractility of the myocardium decreases, the volume of pumped blood decreases, therefore all organs and systems suffer from ischemia. Liver and kidney failure, brain hypoxia, and neurological deficits develop.
Death is a matter of time. Fortunately, such a fatal scenario is not a matter of just one year. There are chances for high-quality diagnosis and the prescription of adequate therapy.
Classification and degrees
Typifications that are used in clinical practice.
According to the number and nature of symptoms:
- No manifestations. The most common option. There is no picture at all, the patient feels fine. Changes in the electrocardiogram are absent or insignificant. Diagnosing pathology at this stage is a great success.
- With mild symptoms. Deviations occur when 10-30% of the sinus node cells die.
- With pronounced clinical signs. It can be easily detected by objective methods. Treatment is prescribed urgently, there is a risk of death of the patient.
Depending on the current:
- Paroxysmal type. Symptoms or, in their absence, signs on the ECG are inconsistently detected. Develops in episodes. Each lasts from a few minutes to hours. Such moments may arise repeatedly.
- Persistent form. About the same thing, only the duration is longer. Several days in a row.
- Chronic variety. Symptoms and the objective picture do not disappear at all; they are constantly recorded.
- Spicy. The symptoms are most pronounced; with significant cardiac dysfunction, there is a high risk of cardiac arrest and sudden death of the patient.
Depending on the main feature:
- Sinoatrial node block (SA block).
- Slowing down the sinus cluster.
- Classic sinus bradycardia.
All three forms appear approximately the same. ECG findings vary. The critical option is to stop the natural pacemaker. This is a direct path to death, asystole.
Based on etiology:
- Primary variety. Develops as a result of heart disease itself.
- Secondary. Or external. The result is the influence of other pathological conditions.
There are only three degrees of intra-atrial conduction disturbance:
- First. The patient has no complaints about his health. Objectively, minor deviations in the electrocardiogram are detected. The discovery was purely an accident.
- Second. The symptoms are pronounced, the ECG pattern is clearly visible. Specific signs make it possible to detect blockade or disruption of the sinus node. This is the most common point of diagnosis.
- Third. All manifestations are expressed to the maximum extent. The cardiologist notices “his” patients with the naked eye. A cardiogram verifies conduction disturbances. Treatment is urgent, otherwise cardiac arrest will occur as a result of insufficient stimulation and death of the person.
Causes cardiac
All factors need to be considered in the system. During the survey, they are excluded one by one.
A sharp increase in blood pressure
If, against the background of chronic hypertension and a gradual increase in blood pressure, the body somehow manages to adapt to new, albeit difficult, conditions, a rapid increase in the tonometer reading leads to overload of the right atrium.
The result is damage to the cells of the sinus node. If such episodes are repeated, and this is exactly what happens against the background of uncorrected hypertension, more and more cells die.
Progression depends on the course of headache. Crises have an even more severe impact.
Inflammation of the heart muscle or myocarditis
It has a detrimental effect mainly on the atria. Without treatment it leads to tissue destruction and severe scarring.
The sinus node is located in the right chamber, and its partial destruction is possible. Slow conduction is a complication of the disease.
The nature of inflammation can be infectious or autoimmune. Both forms are acute, with a pronounced clinical picture of the heart, blood vessels, respiratory and nervous systems.
Treatment is strictly in a hospital. Endocarditis is a similar pathological process affecting the inner lining of the heart. Less often it leads to a slowdown, but this is also possible.
Coronary insufficiency
Narrowing or blockage of special arteries that supply the heart itself. Tissue necrosis is a variant of the condition. Another is possible. The so-called angina pectoris.
It is not so catastrophic; there is death, but the process does not reach that critical point when destruction leads to damage to large areas.
May last for years. It flows spasmodically. In waves. Each episode destroys part of the myocardium. The result is insufficiency and dysfunction. The sinus node suffers not least.
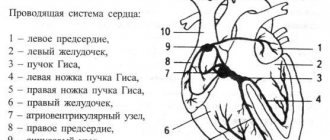
In addition to the death of cardiomyocytes, scarring of the impulse pathways occurs. The so-called bundle of His and its branches (legs), which leads to blockade.
Atherosclerosis of the coronary arteries or aorta
The essence of the process is the formation of cholesterol plaques that close the lumen of blood vessels. Blood flow weakens, pressure in the atria and ventricles increases.
How the growth of the indicator ends is with an increase in load and tissue destruction at the cellular level.
There is another variant of pathology - narrowing of the lumen of the arteries. This is the result of smoking, vasculitis, when the walls of blood vessels scar and close, alcohol abuse, and other autoimmune pathologies.
Treatment is urgent, conservative in the first stages. If ineffective, surgical intervention is indicated.
Heart attack
Acute circulatory disorder in the heart muscle. Leads to rapid destruction of cardiomyocytes. The process is avalanche-like, the longer the ischemia is observed, the more significant the area of destruction.
Major heart attacks are almost guaranteed to result in death. Even with colossal luck, the process will not pass without a trace. Heart regeneration is impossible. The affected tissue is replaced by scar tissue, unable to contract or create impulse. The result is ischemic disease.
What does normal conductivity depend on?
Studies have shown that for blockade to appear in the conduction system of the heart, damage to 1 mm of the atrioventricular communication is sufficient. The normal spread of excitation depends on:
- the content of parasympathetic and sympathetic mediators of the nervous system in the blood (acetylcholine slows down conduction in all parts, norepinephrine speeds up);
- ischemia of the myocardial zone along which the conduction pathways pass, it causes a direct block or indirect through a change in the acid-base balance in the affected area (creates a local zone of acidosis) of the heart;
- level of adrenal hormones (glucocorticoids, catecholamines);
- concentration of potassium in the blood (with hyperkalemia, conduction slows down, hypokalemia accelerates the speed of impulse transmission along the extra- and intraventricular pathways.
Extracardiac causes
Other factors also play a role, although they are not directly related to the heart. They are easier to correct, and there is the possibility of completely eradicating conduction disorders:
- Cardioversion performed. Prescribed to patients with paroxysmal tachycardias and other arrhythmias. The procedure involves placing electrodes and passing a charge through the heart.
A side effect is a slowdown in conduction due to dysfunction of the sinus node. Correction using medications.
This is a reversible condition. The acute period requires resuscitation, but this phenomenon occurs relatively rarely.
- Compression of the neck at the level of the carotid sinus. As a result of wearing clothes with a tight collar, tie, jewelry. The process is also reversible, but threatening acute variants of the condition are possible. Nocturnal cessation of breathing or apnea. It develops in patients with ENT problems, obese people, and severe snoring. Heart pathologies in this category of people are a proven fact. The condition needs to be corrected as soon as possible.
- Stroke affecting the subarachnoid space. Violation of cardiac activity is a purely reflex act associated with dysfunction of the parasympathetic region of the autonomic nervous system. Requires urgent medical attention. A prerequisite for the development of deviations is bleeding. The same effect is observed in traumatic brain injuries with the formation of a hematoma.
- Prolonged or improper use of certain medications. Particularly dangerous are cardiac glycosides, calcium antagonists, beta-blockers, neuroleptics, anxiolytics (tranquilizers), mood stabilizers, psychotropic drugs in general, opioids, narcotic analgesics, corticosteroids in inappropriately large dosages, and others. Correction of the treatment regimen or replacement of drugs is required.
- Excessive amount of potassium in the body. Excessive consumption takes its toll. It is difficult to achieve such a concentration with food; most likely, the patient is taking drugs like Asparkam.
- Excess calcium in the bloodstream. The result of leaching of mineral salt from bones. Observed in cases of cancer and prolonged immobilization. Osteoporosis. The nutritional factor does not play a role.
- Intoxication with salts of heavy metals, tumor decay products (for cancer, especially advanced ones).
- Increased intracranial pressure (hypertension caused by impaired outflow of cerebrospinal fluid).
Factors are taken into account in the system. Diagnostics puts an end to the issue. It is extremely rare that no cause is found. Then they talk about the idiopathic form. May be revised in the future.
How does pregnancy go with this diagnosis?
Any disruptions in the functioning of the female body during pregnancy are unpredictable, especially when it comes to heart pathologies. Rhythm disturbances are a serious medical problem that threatens the life of the fetus. The mechanisms for the development of such deviations are usually associated with hormonal changes and functional changes that occur in a pregnant woman.
If there is any deviation in the functioning of the cardiovascular system, the patient is referred for diagnostics. The research methods are practically no different from the generally accepted ones. If necessary, drug therapy is prescribed, including antiarrhythmic drugs.
Symptoms
The clinical picture is variable. In some cases it is absent altogether. The patient does not experience any difficulties in everyday life or when performing work duties.
Attention:
Insufficient conductivity is an incidental finding. There are also acute forms that are aggressive and often end in death.
A sample list of symptoms looks like this:
- Blood pressure surges. Sometimes low, sometimes high. The change in numbers is not due to any external factor, such as physical activity or food intake. This is a spontaneous process. As it progresses, frequent crises with high tonometer readings develop. The effect of the drugs is minimal.
- Peripheral edema. The lower extremities suffer, less often the fingers. Face.
- Dyspnea. After intense physical activity. When the process enters the critical phase (stage 3 and beyond), it is observed in a state of rest.
- Discomfort and pain in the chest of moderate intensity. Severe attacks are uncharacteristic, although this is also possible with a parallel course of angina pectoris. Nitroglycerin has no effect.
- Darkening in the eyes, tinnitus, headache, fog in the field of vision, flickering, vertigo, inability to navigate in space, fainting. The result of insufficient blood circulation in cerebral structures.
- Weakness, drowsiness, decreased performance. Already from the second stage. In some cases, symptoms are also detected at the first stage.
- Bradycardia. Decrease in heart rate. Up to 50-60 beats per minute and below.
During acute periods or moments of deterioration, apathy or psychomotor agitation, fear, suffocation, pallor of the skin, mucous membranes, and cyanosis of the nasolabial triangle are also noted.
As part of the development of heart failure, ascites is possible - an enlargement of the abdomen due to the accumulation of fluid.
Kinds
Sinoatrial blockade
Violation of sinoatrial conduction of the heart is a condition when impulses that appear in the sinus node do not fully reach the atria, which delays excitation. This situation is sometimes typical for a healthy person and does not require urgent treatment. But most often, heart block occurs against the background of organic heart disease.
The reasons for the violation may be:
- NCD with a predominant effect on the sinus node, which causes a slowdown in heart rate;
- an increase in heart size in people actively involved in sports;
- uncontrolled use of glycosides used to treat arrhythmia;
- congenital and acquired heart defects;
Symptoms of complete sinoatrial block:
- heart rhythm disturbance;
- dizziness;
- pain in the sternum;
- pulse rate is less than fifty beats per minute.
With partial violation, there are practically no signs.
Intraatrial block
Slowing intraatrial conduction is not dangerous to human life, but can cause irregular heart function, which leads to very dangerous consequences.
The causes of intraatrial conduction of the heart are:
- glycoside intoxication;
- rheumatism;
- heart development disorders;
- persistently high blood pressure.
Signs of acute manifestations of conduction slowing do not appear until the electrocardiogram.
In the chronic course of the disease, patients complain of shortness of breath both during movement and at rest, swelling of the legs, acrocyanosis of the skin, pain in the sternum, and others.
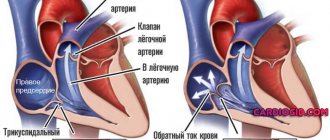
Atrioventricular block
Violation of cardiac conduction through the atrioventricular node of the first and second degrees appears when there is a delay in the transmission of impulses from the atria to the ventricles.
- Violation of intraventricular conduction of the heart: classification, causes, signs, treatment
With third-degree blockade, the ventricles contract independently of the atria, since impulses do not reach them at all. Thus, a dangerous condition for the body arises, and sudden death is possible.
Causes of atrioventricular block:
- heart pathologies, congenital and acquired;
- estate;
- myocardial inflammation;
- toxic hormonal influence.
The danger of the condition is that in the absence of treatment, active development of the blockade is noted.
The symptoms of a blockade of the first two degrees are not pronounced, especially if the pulse is within fifty-five beats per minute. The third degree is characterized by cardiac bradycardia (pulse rate within forty beats), weakness, and short-term fainting. In this state, convulsions occur. The patient requires urgent medical care, the absence of which can lead to death.
Intraventricular block
Violation of intraventricular conduction of the heart is a complete or partial block of the bundle branches. There are disorders of the contractility of the right or left ventricles.
The causes of intraventricular conduction of the heart are as follows:
- opening between the atria;
- myocardial proliferation;
- ischemia;
- myocardial infarction;
- pulmonary diseases;
- cardiosclerosis.
An ordinary person may experience a partial right bundle branch block that is asymptomatic.
Complete blockade is manifested by bradycardia, pain in the sternum, and short-term loss of consciousness. If there is pressing pain in the thoracic region, nausea, weakness, the cardiogram will show complete blockade on the left, then a heart attack can be diagnosed. Only a multiple cardiogram shows this accurately. For such indications, urgent inpatient treatment of the patient is required.
Sometimes the impulse is blocked in distant parts of the heart - Purkinje fibers. This phenomenon is called nonspecific intraventricular conduction disorder. The reasons are the same, but the symptoms are practically absent.
Wolff–Parkinson–White syndrome
This is a condition in which the impulse is accelerated. This disruption occurs due to the activity of accessory pathways. As a result of this, impulses reach the ventricle in greater quantities than they should, the ventricles contract more often, and the impulses pass in the opposite direction. The result of this process is supraventricular tachycardia of the heart.
- Are intraventricular conduction disorders dangerous?
Normal heart rhythm on ECG and atrial fibrillation
Wolff–Parkinson–White syndrome is congenital. During normal pregnancy, the fetal accessory pathways close at approximately twenty weeks.
This pathology can be caused by various external factors affecting the unborn child. This includes an increased radioactive background, the use of drugs and alcohol by the expectant mother during pregnancy. A genetic factor may also be the cause.
Signs are noticed in early childhood, although sometimes the disease is asymptomatic until adulthood. Rarely, the disease is detected during a medical examination by analyzing the electrocardiogram. A symptom of arrhythmia is an increase in heart rate up to two hundred beats. In this case, the patient complains of pain, breathing problems, and oxygen deficiency. In some cases, cardiac fibrillation may develop, which is a threat to the patient’s life.
One type of SVC syndrome is shortened PQ interval syndrome. The James bundles play the role of pathological pathways. When diagnosing a disorder only by a cardiogram, without outwardly having any signs, experts call the phenomenon a phenomenon, and in case of rapid heartbeat - shortened PQ syndrome. The difference can only be seen in the cardiogram readings.
Diagnostics
It takes place on an outpatient basis. Impaired intra-atrial conduction means that there is damage to the sinus node. A thorough examination is required to detect the causes of this phenomenon.
Sample list:
- Oral interview with the patient by a cardiologist. When complaints appeared, whether they exist at all, how much they interfere with daily activities and other points are subject to clarification.
- Anamnesis collection. Family history, lifestyle, past or current pathologies.
- Measurement of blood pressure and heart rate. The classic picture is that blood pressure is unstable, even when the procedure is repeated after 10-15 minutes, an increase in the indicator prevails. Heart rate is consistently below normal.
- Daily monitoring. Gives a lot of information about the dynamics of the same levels over 24 hours. The result is an indirect confirmation of the presence of conduction disturbances in the atria.
- Echocardiography. Visual assessment method. Deviations of anatomical development are detected only with gross defects, after a heart attack, inflammation and other moments. In advanced forms, the left ventricle enlarges and blood flow is disrupted.
- X-ray of the chest. An increase in the pulmonary pattern and an increase in the size of the heart are detected.
- ECG. Profile research. Gives basic information. Typical features: decreased pulse, deformation or complete disappearance of atrial waves (P), heart rate does not increase during physical activity, detection of replacement sliding complexes. A slowdown in AV conduction on the EGC is recorded even in the early stages.
EPI is also performed (for severe concomitant diseases, the technique is not used); if necessary, a consultation with a neurologist is prescribed.
Treatment
{banner_banstat9}
Therapy depends on the form and course. Early stages that do not produce obvious symptoms and do not interfere with the patient in any way do not require urgent supervision. Further examination and clarification of the etiology of the process is necessary.
In case of secondary origin, the underlying disease is eliminated. Cardioprotectors, such as Mildronate, and vitamin and mineral complexes are prescribed as a supportive measure.
The patient is monitored every 3 months. Deterioration of the condition is the basis for surgical intervention. The way is implantation of a pacemaker, which artificially creates the required electrical impulse.
As a measure to prepare for surgical treatment, the use of antiarrhythmics (Amiodarone), antihypertensives (Perindopril in different trade variations, Moxonidine, Diltiazem or Verapamil, others, at the discretion of the treating specialist), diuretics, and cardioprotectors is indicated. Cardiac glycosides as needed.
Also indicated are cessation of smoking, drinking alcohol, excessive physical activity, and consumption of fatty foods (treatment table No. 10).
Therapeutic measures
Slowing of intraatrial conduction on the ECG, occurring in an acute form, requires specific therapy.
| Drug groups | Drug names | Action provided |
| Anticholinergics | atropine, scopolamine, platyphylline | Reducing smooth muscle tone, improving the conduction of electrical impulses in the heart. |
| Vasopressors | norepinephrine | Increased blood pressure |
| Glucocorticoids | hydrocartisone | Stopping and relieving inflammation |
| Diuretics | lasix, furosemide | Removing excess potassium and fluid from the body. |
| Cardiac glycosides | cordigitite, lantoside, adonis-bromine | Elimination of arrhythmia, stimulation of the heart muscle. |
In some cases, the doctor decides on the advisability of using sedatives.
Pregnant women are prescribed magnesium supplements, which do not have a negative effect on the development of the fetus. Other medications aimed at improving intraatrial conduction are used only for clinical indications when there is a threat to the mother's life.
Forecast
{banner_banstat10}
Depends on the diagnosis. Primary forms cannot be cured, but in the early stages they can be corrected with medication, the survival rate is 90% or higher.
Secondary ones require relief of the cause. Mortality due to atrial conduction disorders generally ranges from 10-60%, acute forms are fatal in 40% of situations. The death of more than 90% of sinus node cells almost always leads to death.
Young patients without bad habits, with a good family history, relatively healthy, have a better chance of survival.
What can cause conduction problems?
The causes of conduction disturbances may be:
- general diseases accompanied by changes in metabolism (endocrine pathology, systemic collagenosis);
- local damage to the conduction system by zones of ischemia, inflammation, cardiosclerosis, myocardial stretching with hypertrophy of individual areas.
After scarring of the necrosis zone, myofibrils and conductive cells are gradually replaced by areas of cardiosclerosis
An inflammatory reaction (myocarditis) most often occurs when:
- acute infectious diseases of a viral and bacterial nature (influenza, ARVI, diphtheria in children, rheumatic attacks after tonsillitis);
- autoallergic processes against the background of vasculitis involving the coronary vessels;
- productive granulomatous inflammation.
The ischemic zone, caused by insufficient blood supply to the conducting fibers, depends on thrombus formation in both the right and left branches of the coronary artery. Sometimes the possible localization of a heart attack is judged by the appearance of intraventricular blockade.
Pathology is observed in acute heart attack and chronic coronary insufficiency.
Heart defects cause deformation of the heart chambers, overstretching and hypertrophy. Therefore, conduction disorders are not uncommon in children with congenital changes in the structure of the chambers and valve apparatus.
The development of left ventricular hypertrophy with hypertension and cardiomyopathy also leads to interruption of the ventricular impulse propagation pathways. In these cases, the degree of blockade indicates the severity of the lesion.
Complications
The cause of intraatrial conduction disturbance is weakness or dysfunction of the sinus node.
The condition threatens with the following consequences:
- Cardiac arrest or asystole. The result of insufficient stimulation of cardiac structures, in particular the muscle layer.
- Heart attack. The result of poor nutrition. Little blood flows through the coronary arteries. Hence acute necrosis or, at least, repeated attacks.
- Stroke. Death of nerve cells and tissues. Ends in death or permanent neurological deficit.
- Cardiogenic shock.
- Fainting and injuries incompatible with life.
- Vascular dementia.
All conditions, one way or another, lead to a minimum of severe disability. There is no point in delaying therapy, if indicated.
Electrophysiology of intraatrial conduction slowing
Slowing of intraatrial conduction on the ECG is assessed by the state of the P wave, the duration of which normally should not exceed 0.11 s. This disorder may be caused by hypertrophy of the left atrium or a failure in the conduction of impulses along the Bachmann bundle.
Slowing of intraatrial conduction on the ECG.
If a P wave splitting for more than 0.02 s appears on the cardiogram, then the specialist predicts the possibility in the near future of complete heart block, which is observed with myocardial infarction and coronary artery disease.