Tricuspid regurgitation is the reversal of blood flow from the right ventricle back into the atrium, but is not a diagnosis in itself. This is not even a disease, but a consequence of a malfunction of the tricuspid valve, which closes the passage from the right atrium to the corresponding ventricle.
The condition can be primary or secondary, depending on the origin of the pathological process. Recovery is carried out surgically.
The prospects for a complete cure are good, but only in the early stages, when there are no anatomical defects in the heart or distant systems yet.
Fortunately, the duration of the initial phase is sufficient for a thorough diagnosis. The intervention is planned, except for exceptional cases.
The approximate time frame from the moment the deviation occurs to the formation of a clear clinic is 3-6 years.
Development mechanism
The essence of the pathological process is the disruption of hemodynamics at the local level and the formation of a persistent anatomical defect.
In the normal state of affairs, blood in the cardiac structures moves strictly in one direction, ending the cycle in the left ventricle and being transported to the aorta, and from there to its branches in a large circle.
The heart is represented by a group of chambers, each separated from the other by valves, which does not allow fluid connective tissue to move in the opposite direction.
The tricuspid structure closes the gap between the right atrium and ventricle. In case of weakness, insufficiency, or defects of the connective tissue, a reverse flow of blood or regurgitation occurs, which is called according to the name of the valve that causes the condition.
The result of the deviation is, firstly, a disruption in the transport of blood in the small circle, and secondly, an insufficient amount of it, which is released into the aorta.
This leads to generalized hemodynamic deviations, tissue hypoxia, and multiple organ failure in the future.
List of sources
- L.A. Boqueria, O.L. Bockeria, E.R. Jobava review article “Functional mitral regurgitation in atrial fibrillation”, 2015
- Mashina T.V., Golukhova E.Z. Left ventricular diastolic dysfunction in patients with atrial fibrillation: pathogenetic mechanisms and modern ultrasound assessment methods (analytical review). Creative cardiology. 2014
- Karpova N.Yu., Rashid M.A., Kazakova T.V. , Shostak N.A. Aortic regurgitation, Regular issues of “RMZh” No. 12 from 06/02/2014
Forms of violation
Typification of the pathological process is carried out on two grounds.
Based on the origin of the anatomical defect, they talk about:
- Primary form. It develops spontaneously, against the background of cardiac problems themselves. Including aortic insufficiency, previous inflammatory, infectious conditions and others.
It is characterized by greater complexity from the point of view of cure and prospects for recovery, since correction requires not only the symptomatic component, but also the acquired defect.
This group also includes congenital factors caused by genetic defects and spontaneous deformations of the tricuspid valve.
- Secondary variety. Against the background of current pathologies of distant organs and systems.
Procedures and operations
In cases of acute regurgitation, patients undergo emergency valve replacement. The modified valve is removed and an artificial one is installed in its place. In some cases, valve repair is sufficient. During the rehabilitation period, patients are prescribed medications that support normal cardiac activity: vasodilators and nootropics. In case of a chronic process, surgical interventions to replace the valve are also performed routinely as negative dynamics progress. In the absence of negative symptoms and stable EchoCG indicators, symptomatic therapy is prescribed.
Degrees of regurgitation
Another basis for classification is the degree of deviation from the norm. Also called stages of the pathological process.
Accordingly, they distinguish:
- Weakly expressed type. 1st degree. The amount of blood returning is not known exactly. The volumes of the jet do not exceed 1 cm in diameter. The intensity of manifestations with minimal tricuspid regurgitation is insignificant or completely absent, which makes early diagnosis a matter of luck. This is the best time to start therapy under the supervision of cardiac surgeons.
- Moderate type. 2nd degree. Characterized by disruption of normal blood flow in a volume of 2 cm, no more. Recovery is carried out surgically. The clinical picture is minimal, characterized by chest pain, shortness of breath during intense physical activity. There is a chance for a complete cure, the likelihood of the formation of persistent cardiac and extracardiac defects is present, but it is not yet great. Even if these occur, the likelihood of a high-quality, long life is maximum.
- Expressed type. 3rd degree. A stream of blood more than 2 cm in diameter. Chronic heart failure of congestive type develops. There are prospects for recovery, but they are not complete, and long-term, lifelong maintenance therapy is required.
- Terminal phase. 4th degree. Surgical assistance does not make much sense, since the heart, kidneys, liver, and brain are significantly changed. Recovery is impossible; palliative care is required to ensure an acceptable quality of life for the short remaining period of life. Death occurs from acute heart failure.
Classifications are used to accurately assess the patient’s condition, prospects for treatment, and determine diagnostic and therapeutic tactics.
Clinical manifestations
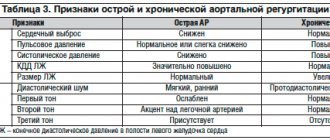
In the acute form of aortic regurgitation, the patient suddenly exhibits signs of cardiogenic shock:
- severe weakness;
- pale skin;
- severe hypotension;
- dyspnea.
For pulmonary edema:
- the patient is suffocating;
- breathing is noisy and hoarse;
- when coughing, foamy sputum mixed with blood is released;
- face, lips, limbs are cyanotic;
- heart sounds are sharply muffled;
- A lot of moist rales are heard in the lungs.
With chronic aortic regurgitation, a long asymptomatic period is possible. Symptoms appear only with the development of myocardial ischemia and severe cardiac decompensation. The patient notes:
- shortness of breath on exertion;
- strong heartbeats;
- extrasystoles;
- angina attacks at night;
- a “cardiac asthma” clinic is possible.
During the examination, the doctor notes:
- shaking the head in rhythm with the pulsation of the heart;
- a typical pulse on the radial artery is a sharp shock wave and an immediate fall;
- trembling when palpating the chest at the base of the heart;
- expansion of the left cardiac border;
- pulsating carotid arteries;
- diastolic murmur on the aorta, along the left edge of the sternum in the third and fourth intercostal spaces, is better heard in a sitting position with a slight bend forward, the first sound is clapping.
How dangerous is the disease?
Complications arise starting from the third, less often the second stage of the pathological process. Tricuspid valve regurgitation determines the following consequences for health and life:
- Acute heart failure. Disruption of the normal functioning of cardiac structures. It is characterized by a triad of signs: a decrease in blood output, a drop in local and generalized hemodynamics, and arrhythmic processes. It has a short period of development in an acute case; in a latent course, the duration of formation of a full-fledged picture is 2-4 weeks; death occurs as a result of stopping the work of a muscular organ.
- Cardiogenic shock. The condition is lethal in almost 100% of cases. There is no prospect of cure. Even with partial recovery, there is a guarantee of a repeat episode.
- Heart attack. Myocardial nutritional disturbances, acute tissue necrosis and, as a result, decreased functional activity. Heart failure develops with all its consequences.
- Stroke. Cerebral ischemia.
- Dangerous forms of arrhythmia leading to cardiac arrest.
Minor regurgitation provokes fatal complications in 0.3-2% of cases, often the result of a random coincidence.
Hemodynamically significant forms determine the risk of death in a wide range: from 10 to 70% and higher.
The main cause of death is not regurgitation, but organic defects of the heart and systems developing against its background.
Consequences and complications
In acute mitral regurgitation, the prognosis is extremely unfavorable in the absence of timely surgical care. The prognosis worsens with the addition of heart failure. In the second degree of the disease, the 5-year survival rate without surgery is 38% for men and 45% for women. Regurgitation can be complicated by endocarditis (non-infectious and infectious origin), rhythm disturbances, myocardial infarction , heart failure .
Causes
Factors of formation are divided into primary and secondary, according to the main forms of the pathological process.
Primary factors
- Burdened heredity. Leads to the development of tricuspid valve insufficiency. Problems arise during the prenatal period. In this case, there is a genetic predisposition. The exact mechanism, however, is not known.
One thing has been proven: in the presence of a sick parent, children are born with the defect in question and regurgitation in 12-15% of cases. Spontaneous defects of the perinatal period are possible, caused by internal and external factors.
- Spikes in the heart. These are small fibrin strands that disrupt the normal anatomical structure of the organ. They develop as a result of inflammatory processes of any type, especially infectious. This is a kind of protective mechanism, as well as further deposition of calcium salts to isolate the affected area.
- Previous heart attack. It ends with the replacement of functionally active tissues with weak, scarred ones, incapable of contraction, signal transmission, or spontaneous excitation.
If the process affects the tricuspid valve, the following options are possible: its complete fusion, stenosis, or functional failure, immediately leading to severe regurgitation. Recovery is urgent, surgical.
- Inflammatory pathologies of the heart (myocarditis and others). Accompanied by rapid destruction of tissue of cardiac structures. Treatment is urgent, in a hospital, with the use of antibiotics and NSAIDs, as well as steroids and diuretics.
- Rheumatism. Inflammatory pathology of a chronic nature, with frequent relapses and short periods of remission. Therapy is lifelong, using supportive tactics. If necessary, surgical correction of the consequences is performed.
Secondary factors
The secondary pathological process is caused by cardiac problems and extracardiac issues:
- Pulmonary hypertension and the development of specific abnormalities in the anatomical development of the heart. Requires urgent treatment in the early stages, since in the later stages there is no longer any sense. The main risks are smokers, alcoholics, asthmatics and patients with long-term COPD.
- Cardiomyopathy.
- Endocrine pathologies: hyperthyroidism, excess of adrenal hormones, their deficiency, diabetes mellitus and others.
Risk factors
They do not directly cause tricuspid regurgitation, but lead to the onset of the pathological process:
- Long-term smoking.
- Consuming alcohol in immoderate quantities.
- A long period of immobilization, without the possibility of vigorous activity. Development takes a long time, from six months or more.
- Drug addict.
- Excessive use of “dangerous” drugs: glycosides, antiarrhythmics, progestin agents, also hormonal medications, broad-spectrum antibiotics.
- Harmful working conditions affect chemical, hot production, and mines.
The reasons are considered as a whole; a system of development factors is possible.
Characteristic symptoms
Manifestations depend on the stage of the pathological process. A hemodynamically insignificant variety has no signs at all.
Typical signs in other situations include:
- Liver lesions. They make themselves known in the later stages. They are determined by pain in the right hypochondrium, an increase in the size of the organ, and yellowness of the skin due to excess bilirubin. A gradual formation of insufficiency is possible.
- Abdominal pain of unknown localization. Wandering, radiating to the iliac regions. Acute discomfort is not typical, therefore it is impossible to confuse it with the clinical picture of appendicitis.
- Shortness of breath for no apparent reason. It develops first against the background of intense physical activity, then occurs in a state of complete rest. Significantly reduces quality of life.
- Polyuria. As a result of developing renal failure. At later stages (3-4), with primary damage to the excretory system, it is replaced by a reverse process. Daily diuresis is 500 ml or less.
- Tachycardia. The heart rate reaches 120-150 beats. They are full-fledged, regular. Type - sinus. Less often paroxysmal.
- Weakness, lack of ability to work.
- Feeling of constant cold. The patient freezes because the intensity of peripheral circulation decreases.
- Increased pressure in the veins. Objectively, the symptom is manifested by swelling of the cervical vessels, their intense pulsation, and visible tension. Not only the doctor, but also the patient himself or the people around him can determine the sign. However, blood pressure drops in most cases. Not significant, however, clinical significance is present.
- Swelling of the lower extremities. As a logical continuation of increasing renal failure.
- Breathing problems.
As a result, the patient has a whole range of symptoms from both distant organs and systems, and the cardiac structures themselves. The reason for all the sensations lies in the disruption of blood circulation, both in the large and in the small circle.
Diagnostics
The examination is carried out under the guidance of a cardiologist, and if the process is proven, the specialized surgeon continues to work. He is also responsible for prescribing treatment.
Scheme of events in the correct order:
- Oral questioning of the patient regarding complaints, their duration, as well as collecting anamnesis. This way the doctor understands the direction of further examination.
- Blood pressure measurement. Usually it is slightly reduced. Heart rate is higher than normal. The rhythm is correct; as it progresses, spontaneous premature beats (extrasystoles) occur.
- Listening to sound (auscultation). A sinus noise of reverse blood flow is detected. Tones can be either normal or dull.
- Daily monitoring. To record cardiac performance indicators over 24 hours in dynamics. It is most often used as the first method, after a routine examination. Provides comprehensive information about the movement of blood pressure and heart rate during the day.
- Electrocardiography. Assessment of the functional state of the heart.
- Echocardiography. Method of visualization of cardiac structures. It is carried out as a matter of priority, since it allows one to detect organic abnormalities on the part of the tricuspid valve.
- MRI or CR (much less often). It is carried out to detail the image of the heart and surrounding tissues.
- Pulmonary artery pressure measurement.
- Load tests. At an early stage, later not used due to significant danger.
The methods are aimed both at establishing the fact of an anatomical defect and at verifying the alleged diagnosis.
How much does it cost to treat tricuspid valve insufficiency in children in Israel?
Hadassah is considered one of the best medical institutions in Israel. The most effective methods for recognizing and combating children's heart defects are being developed and implemented here; qualified senior and mid-level physicians work here.
The administration of the medical complex has a competitive pricing policy, so our cost of stay is average across the country and is 20–30% lower than in Europe and America. In addition, all prices are controlled by the Israeli Ministry of Health.
Treatment methods
Therapy is carried out under the full supervision of a cardiac surgeon. Methods of exposure depend on the stage of the pathological process.
Grade 1 tricuspid regurgitation is the best time to start therapy. But there are no symptoms yet, identification is incidental (random), and does not pose any difficulties during a targeted search.
At this stage, dynamic observation for 3-5 years is indicated. In the absence of progression, with stagnation of the process, there is no need for treatment. Sometimes patients can live a quality life without knowing about their condition, without major restrictions.
Tricuspid regurgitation of grade 2 and higher is corrected strictly surgically. There are several intervention options.
But before the treatment stage, it is necessary to stabilize the patient’s condition, if there is time for that (planned operations).
Drugs used:
- Antiarrhythmics in the minimum dosage to restore an acceptable heart rate (Amiodarone, Hindin).
- Beta blockers (Metoprolol).
- Glycosides. In order to normalize myocardial contractility.
- Cardioprotectors.
- Anticoagulants. To prevent the formation of blood clots, which cause frequent premature death of patients.
- Diuretics in the treatment of early manifestations of renal conditions.
The duration of the preparatory period varies from 2 to 4 months, possibly more.
By the time of surgery, the rhythm should be stable, correct, blood pressure within the reference value or close to it.
Depending on the stage of the pathological process and the nature of the changes, plasty or prosthetics of the tricuspid valve is indicated. Both methods are generally equivalent.
Correction of pathologies and defects of distant organs is carried out under the supervision of specialized specialists. The list of techniques is wide and is determined based on the severity of the process.
Attention:
The use of folk remedies is impossible. Since the effect of them in case of organic deviation on the part of the cardiac structures is zero.
Changing your lifestyle will also not play a key role. It makes sense to give up smoking, alcohol and drugs. When carrying out severe therapy for third-party pathologies, correction by a treating specialist is recommended.
Forecast
{banner_banstat9}
Depends on the stage and nature of therapy.
- At the first stage, the survival rate is 100%, especially if there is no progression of the condition.
- The second is associated with a probability of 85%.
- Third - 45%.
- The fourth or terminal puts an end to the patient, giving no chance. The median is 1-2 years, often even less.
When carrying out complex therapy, it is possible to stabilize the conditions of even the most severe patients, prolonging life for several years.
Favorable prognostic factors:
- Period of youth.
- Absence of somatic pathologies, bad habits, complications after the operation.
- Good family history.
- Response to treatment.
- Reduction of symptoms.
Determining the possible outcome falls on the shoulders of the cardiologist. In order to say anything concrete, you need to at least carry out a full diagnosis.