According to research1 by the World Health Organization, cardiovascular pathologies are in first place among the causes of mortality: coronary heart disease, stroke and similar diseases. It is much easier to prevent them than to eliminate the consequences.
In addition to regular examinations, weight control and moderate physical activity, a diet rich in omega-3 polyunsaturated fatty acids (PUFAs) is of great importance for the prevention of heart and vascular diseases. There are many of them, but the most valuable of them are EPA and DHA, eicosapentaenoic acid and docosahexaenoic acid. They help maintain a healthy heart, brain, and immune system.
The human body does not synthesize PUFAs; we must obtain them from food. EPA and DHA are found in fish oil from mackerel, salmon, herring, halibut and a number of other fish, but people do not eat them in adequate quantities. Therefore, it is important to take special “heart vitamins” - omega-3.
Introduction
Diseases of the cardiovascular system (CVD) are the leading cause of premature death and loss of years of life.
The most common diseases are coronary artery disease, ischemic stroke, and peripheral artery disease [1, 2]. The development of dyslipidemias may be caused by other diseases (secondary dyslipidemias) or a combination of hereditary predisposition and adverse environmental factors. Prevention and treatment of dyslipidemia are considered within the framework of preventing the development of cardiovascular diseases - CVD [3]. In addition to elevated total cholesterol (TC) and low-density lipoprotein (LDL) levels, some other types of dyslipidemia also increase the risk of developing CVD. The most common is a certain combination called the atherogenic lipid triad. This triad includes an increase in very low-density lipoprotein (VLDL) remnants, which is manifested by a moderate increase in triglycerides (TG), an increase in small LDL particles, and a decrease in high-density lipoprotein (HDL) levels. Data from clinical studies aimed at assessing the effectiveness and safety of influencing these factors to reduce the risk of CVD are limited. Therefore, this triad and its individual components should be considered as additional targets for the prevention of CVD diseases.
When prescribing drug therapy, the greatest attention should be paid to reducing the level of TC and LDL, which can be influenced by changing the patient’s lifestyle (reducing excess body weight, increasing the level of regular physical activity, anti-atherosclerotic diet, etc.). Therapy for lipid metabolism disorders is currently based on the degree of risk of a particular patient, identified using special tables [3]. The target LDL level in patients at high and very high risk is 1.8 mmol/L. Today, it is not enough to limit ourselves to achieving target levels only for LDL, it is also necessary to focus on target levels of non-HDL cholesterol, HDL and apo-B levels, especially for individuals with obesity, metabolic syndrome and type 2 diabetes mellitus. Prevention and treatment of dyslipidemia should be considered from the point of view of preventing the development of cardiovascular diseases.
The table shows comparative characteristics of drugs that correct blood lipid levels [4]:
Note. LDL - low-density lipoproteins, HDL - high-density lipoproteins, Apo LP - apolipoproteins, LP(a) - lipoprotein (a). ↑ – increase in level, ↓ – decrease in level, 0 – no effect (the number of crosses indicates the severity of the effect).
As can be seen from the table, statins and bile acid sequestrants have the strongest hypocholesterolemic effect. They are rightfully considered hypocholesterolemic drugs, although they can moderately affect HDL and TG levels. These drugs are prescribed for hypercholesterolemia and moderate hypertriglyceridemia.
Fibrates have a pronounced hypotriglyceridemic effect and a very moderate hypocholesterolemic effect. Therefore, they are prescribed for isolated and combined hypertriglyceridemia. Nicotinic acid combines equal hypocholesterolemic and hypotriglyceridemic activity. The drug quite significantly increases the concentration of HDL and lowers the level of Lp(a), so it is prescribed in cases of mixed hyper- and dyslipidemia. Cholesterol absorption inhibitors moderately reduce LDL levels and are mainly used for combination therapy. Fish oil preparations are used for hypertriglyceridemia and low HDL levels.
Thus, each group of drugs has its own niche in the spectrum of lipid disorders, but absolute importance in practice remains with statins due to the highest prevalence of hypercholesterolemia among the population.
Harmful and healthy fats
Fat is an essential element of the human body. This substance is part of the cell membrane. Without fats, no system can function. In addition, vitamins of some groups (such as A, D, E, K) are fat-soluble. That is, without this connection they simply will not be absorbed.
Fats ensure stable functioning of the digestive system, sufficient production of hormones, and maintain good condition of the skin, nail plates, and hair. Not all such substances are beneficial. The body needs unsaturated fats. Saturated ones, on the contrary, are poorly digested and are deposited in the form of excess fatty tissue.
Most unsaturated compounds are of plant origin and are liquid. Saturated fats found in dairy products, meat, lard, solid. You should not completely abandon the listed products. They contain a lot of protein, vitamins, and minerals necessary for the full formation of cells and tissues. Saturated fats need to be introduced into the diet in doses, as they cause an increase in the content of low-density lipoproteins (“bad” cholesterol).
Attention: with strong heating, vegetable oils lose their beneficial properties. When exposed to high temperatures, carcinogens are formed in them!
The most harmful are trans fats (or hydrogenated oils), which are difficult to digest and have extremely low nutritional value. They have a destructive effect on the pancreas, digestive and cardiovascular systems.
This difference in how the body perceives fats is explained by their structural differences. The benefits come from compounds saturated with fatty acids.
Omega-3 polyunsaturated fatty acids
In 1971, an article was published in the Lancet journal [5], which spoke about the lower content of atherogenic lipoprotein fractions in the blood plasma of Eskimos compared to continental Danes (the difference is statistically significant), which was explained by the peculiarities of the Eskimo diet, which contains a large amount of seafood in its composition. However, this message remained virtually unheeded.
Interest in omega-3 polyunsaturated fatty acids (ω-3 PUFAs) arose after the publication of the results of a Danish epidemiological study, in which the morbidity patterns of Greenlandic Eskimos and continental Danes were studied for 24 years (1950–1974, number of participants – 1800) [6]. It has been shown that Eskimos suffer little from myocardial infarction (MI), multifocal atherosclerosis, diabetes mellitus, thyrotoxicosis and psoriasis. These differences were associated with the nutritional habits of the Eskimos, since they consume large amounts of ω-3 PUFAs with food (13 g versus 1 g per day, respectively). These observations were subsequently confirmed by a number of large epidemiological studies, which traced and determined an inverse statistically significant correlation between the level of ω-3 PUFAs in the blood plasma and the risk of developing fatal and non-fatal MI.
For example, in the epidemiological study of the Honolula Health Program (observation period of 8006 Japanese people - 1963-1988), the effect of a diet rich in seafood (systematic consumption of fresh fish more than 2 times a week) on the risk of mortality from coronary heart disease (CHD) was investigated [ 7]. The results of this study indicated that individuals who systematically consume seafood rich in ω-3 PUFAs have a significantly lower risk of mortality from CHD (p < 0.01).
Another study provides data that long-term (20 years) daily consumption of fresh fish (30 g or more) reduces the risk of mortality from CHD by 40–50% [8].
Fatty acids are divided into three groups:
• Saturated fatty acids (lauric, myristic, palmitic and stearic). In their molecules, all carbon atoms are connected by single covalent bonds, and two bonds are replaced by hydrogen atoms. These acids are found in large quantities in coconut, palm, nutmeg oils, as well as in pork fat. A diet that includes these acids contributes to an increase in atherogenic lipoproteins in the blood plasma [9–11].
• Monounsaturated fatty acids (oleic, palmitooleic, elandic, etc.) have one double bond in their molecule. The human diet is dominated by oleic acid, which is found in large quantities in olive oil and peanuts. A diet rich in oleic acid helps reduce the level of anti-atherogenic HDL in the blood plasma.
• Polyunsaturated fatty acids – ω-3 and ω-6 PUFAs. There are several double bonds in the carbon chain of these acids, the number 3 indicating the position of the double bond farthest from the carboxyl group.
ω-3 PUFAs are classified into short-chain (γ-linolenic) and long-chain (eicosapentaenoic [EPA] and docosahexaenoic [DHA]).
Unsaturated fatty acids mainly come from food. There are three groups of unsaturated fatty acids depending on the carbon atom involved in the formation of the last double chain. The main ω-3 PUFAs include ENA and DHA.
ω-3 PUFAs improve endothelial function, reduce platelet aggregation and TG concentration in the blood, have an anti-inflammatory effect, affect the synthesis of eicosanoids, and increase the stability of atherosclerotic plaque [10, 12]. Ingestion of 23 g/day of fish oil (rich in long-chain ω-3 fatty acids) helps reduce TG levels by 25–30% in patients with normo- and hyperlipidemia. For CVD, fried fish prepared in public catering establishments (for example, restaurants and fast food outlets), as well as frozen processed fried fish, should be avoided, as they contain low amounts of ω-3 PUFAs and high amounts of trans fatty acids. Alpha-linoleic acid (a medium-chain ω-3 fatty acid found in chestnuts, some vegetables, and soybean and canola oils) is less effective at lowering TG levels. Long-chain ω-3 PUFAs also reduce the severity of the postprandial lipidemic response. When taken as a dietary supplement at a dose of 3 g/day, an increase in LDL-C levels of approximately 5% may be observed in some patients suffering from hypertriglyceridemia [13].
The source of ω-3 PUFAs can be either a diet rich in marine fish or dietary supplements. The amount of long-chain ω-3 PUFAs (EPA and DHA) consumed through food and/or nutritional supplements should be within 1 g/day [14]. The richest types of long-chain ω-3 PUFA are the following types of marine fish (in descending order): salmon, mackerel, herring, salmon, sardines, tuna and trout. For example, 100 g of salmon contains 18 g of ω-3 PUFA, of which 1.1 g is EPA, vitamin E – 0.3 mg, vitamin D – 6 mg.
It should be noted that heat treatment significantly changes the cis-configuration (geometric, spatial configuration) of ω-3 PUFA. Therefore, it is better to consume them lightly salted (3–5% brine). To maximize the preservation of ω-3 PUFAs, fish should be baked rather than fried. In boiled fish, the preservation of ω-3 PUFAs is slightly higher than in fried fish, but less than in baked fish.
It is preferable to consume fatty fish: anchovies (anchovies), carp, halibut, herring, trout, mackerel, salmon (salmon), striped sea bass, tuna, whitefish.
Omega-9
Monounsaturated Omega-9 consists of oleic acid. Included in most vegetable oils. Contained in nuts, pork, poultry, pork and beef fat.
Omega-9:
- prevents the formation of cholesterol plaques on the walls of blood vessels;
- stabilizes metabolic processes;
- participates in the synthesis of hormones;
- increases immunity.
Lack of connection provokes:
- drying of the skin and mucous membranes;
- brittle nails;
- hypertension;
- weakness;
- digestive disorders.
The listed beneficial properties of fatty acids are not a reason to “pounce” on fried meat and lard in huge quantities. It is important to maintain the optimal level of Omega content for the body.
ω-6 polyunsaturated fatty acids
Linoleic acid (LA), which is the main representative of the ω-6 PUFA families, is found in vegetable fats (sunflower, corn, soybean) and margarines based on them. Arachidonic acid is found in the liver and milk fat of mammals.
It has been shown that low intake of LA (<4% of total caloric intake) and low content in the human body (Finland, Scotland) are associated with an increased risk of coronary heart disease [15]. The optimal consumption of LA is 6% of the total calorie content of food. It is recommended to include in your diet foods that are food sources of γ-linolenic acid, such as soybeans, walnuts, and soybean oil.
According to WHO recommendations, the optimal ratio of ω-6/ω-3 PUFAs in food should range from 5: 1–8: 1. At this ratio, PUFAs entering the human body with food or medications (long-chain ω-3 PUFAs - EPA , DHA), will enter into competitive antagonism with ω-6 PUFAs and, therefore, can implement membrane and cardioprotective effects - suppress the synthesis of arachidonic acid from linolenic acid, i.e. compete with arachidonic acid for binding sites with membrane phospholipids, increase electrical stability of cardiomyocytes, etc. [11].
As a rule, nutritional supplements containing ω-3 PUFAs are well tolerated by patients, but taking them may cause belching with a fishy odor or taste, epigastric pain, nausea, vomiting, flatulence, diarrhea or constipation, exacerbation of chronic pancreatitis, and rarely acne. , eczema.
Contraindications to the use of nutritional supplements are exogenous hypertriglyceridemia (hyperchylomicronemia type I), severe dysfunction of the liver and kidneys, conditions after severe skeletal injuries and surgical interventions (risk of bleeding), childhood and old age, pregnancy, lactation, simultaneous use of fibrates and indirect anticoagulants.
The Russian market offers a fairly large number of food supplements containing ω-3 PUFAs in their composition, but the main drug is Omacor (Norway) - a registered pharmaceutical preparation based on ω-3 PUFAs, standardized in qualitative and quantitative composition, which has an evidence base for effective use in cardiology. Clinical experience in recent years has made it possible to establish the optimal dosage regimen for standard ω-3 PUFA preparations (1–4 g/day for at least 2–4 months).
In a randomized controlled trial of 4837 post-MI patients, the addition of low-dose margarine fortified with ω-3 PUFA (400 mg/day) or α-linolenic acid (2 g/day) did not significantly reduce TG levels. This dietary supplement did not cause a significant reduction in the incidence of cardiovascular complications [16].
Statins and ω-3 fatty acids
Treatment with ω-3 fatty acids (4 g/day) in combination with simvastatin (40 mg/day) for 8 weeks in a randomized, double-blind, placebo-controlled study of 254 patients resulted in a greater reduction in TG levels (29.5 vs 6 .3%) and caused a small but statistically significant increase in HDL levels (2.4 versus 1.2%) compared with the use of statins alone [17].
The use of ω-3 fatty acids in combination with pravastatin and fenofibrate as part of a triple treatment regimen caused a further decrease in TG and homocysteine levels, including in patients with diabetic dyslipidemia. There were no significant interactions of ω-3 fatty acids with other drugs.
In the JELIS (Japan EPA lipid intervention study) study [18], which included more than 18.5 thousand patients with high cardiovascular risk, 100% of the subjects received statins (80% for primary prevention, 20% for secondary prevention). Taking EPA at a dose of 1.8 g/day against the background of standard therapy led to a statistically significant reduction in the number of cardiovascular events (by 19%) compared with placebo. This study was conducted in a Japanese population that initially had a high ω-index, since this country has a historically high culture of consumption of fish and seafood. The use of EPA in combination with low-dose pravastatin, compared with the use of statins alone, reduced the incidence of coronary pathology without affecting the incidence of sudden coronary death. These effects were achieved without significant changes in TC, LDL, or HDL levels and with only a slight decrease in TG levels. Eicosapentaenoic acid may possibly reduce the risk of CVD through mechanisms other than lowering LDL levels. In a subgroup analysis, this combination therapy regimen also reduced the incidence of coronary artery disease in high-risk patients with metabolic syndrome with high TG levels and low HDL levels [19].
ω-3 PUFAs and metabolic syndrome
Metabolic syndrome is characterized by hypertension, excess body weight, elevated TG and glucose levels, decreased plasma HDL levels, and increased urinary albumin excretion. The use of ω-3 PUFAs helps normalize the lipid profile, lower blood pressure (through the vasodilatory properties of eico- and docosanoids), and prevent the loss of albumin in the urine, thereby having a multifaceted effect on metabolism and reducing the risk of diabetes.
In a cohort study of 3504 people (40–69 years old, Korea), consuming fish more than once per week was associated with a lower risk of developing metabolic syndrome (odds ratio [OR] = 0.43, 95% confidence interval [CI] – 0.23 -0.83). The higher the intake of ω-3 PUFA, the lower the risk of developing diabetes (OR = 0.53, 95% CI – 0.28–0.99) [20].
Use of Omacor in acute coronary syndrome
The multicenter, randomized, placebo-controlled study GISSI-Prevenzione study [21] included 11,323 patients with a recent (≥ 3 months ago) MI. These patients took the drug of highly purified ω-3 PUFA Omacor at a dose of 1 g/day for 3.5 years (one capsule contains 84% EPA and DHA). In the groups of patients taking Omacor, the total indicator, which included mortality from all causes, as well as non-fatal MI and stroke, was 15–16% lower than in the placebo group (p = 0.02), and the risk of death from CVD plus non-fatal MI and strokes were lower than in the placebo group by 20–21% (p = 0.006). The greatest reduction in the risk of sudden death was 45% (p = 0.0006), which manifested itself after 4 months of treatment.
In Fig. Figure 1 shows the early effects of ω-3 PUFAs in the GISSI-Prevenzione study on overall mortality (calculations were made taking into account adjustments for drug interactions and main influencing indicators). In Fig. Figure 2 shows the early effects of ω-3 PUFAs on the incidence of sudden death in the same study [22]. Analysis of the results of the GISSI-Prevenzione study showed that the positive effect of ω-3 PUFAs is observed among patients with left ventricular dysfunction after myocardial infarction, who are at high risk of death.
The GISSI research group began another study, GISSI and Prevensione ( [email protected] ) [23], aimed at studying the preventive effects of ω-3 PUFAs in patients at high cardiovascular risk, but without a history of MI. More than 12.5 thousand patients participate in GISSI [email protected] Diabetes mellitus, along with at least one cardiovascular risk factor, is the main criterion for inclusion in this study (47% of patients).
As for the recommendation to increase physical activity, the emphasis is on moderate weight loss and regular moderate-intensity aerobic physical activity, which is very effective in preventing the development of abdominal obesity, metabolic syndrome, and type 2 diabetes. Patients are recommended to exercise 30 minutes a day.
Summary
Proper diet, physical activity and vitamin complexes are the three pillars on which the health of the endocrine system rests. We told you what foods it is advisable to include in your daily diet, and which ones you should avoid. We recommend purchasing multivitamin complexes, and even more so medications for treatment, only after consultation with an endocrinologist. The specialist will also help you choose a special diet and monitor the results of treatment or prevention.
Tokareva Lyudmila Georgievna, therapist, medical offices 36.6
THERE ARE CONTRAINDICATIONS, BEFORE USE YOU MUST CONSULT WITH A SPECIALIST
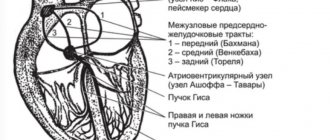
Cardiac arrhythmias and ω-3 PUFAs
Existing problems of antiarrhythmic therapy (limited effectiveness, arrhythmogenic effects, extracardiac side effects, etc.) dictate the need to search for new therapeutic approaches. Of great interest is the study of the possibilities of using ω-3 PUFAs in arrhythmias [24]. Experimental and clinical studies have shown that ω-3 PUFAs have antiarrhythmic properties; in particular, they block voltage-gated sodium channels, L-type calcium channels and potassium channels [10]. Omega-3 PUFAs have a beneficial effect on the function of the autonomic nervous system, the imbalance of which contributes to the development of arrhythmias and adverse cardiovascular outcomes [25].
Omega-3 PUFAs increase heart rate variability (HRV). A positive correlation was found between the content of DHA in cell membranes and an increase in HRV in patients who had suffered an MI, in patients with indications for coronary angiography, in healthy males and in women with initially low HRV [26].
The comparative epidemiological study Zutphen study [27] examined the effectiveness of systematic intake of ω-3 PUFAs (diet containing an average of 250 mg/kg ω-3 PUFAs) on the risk of sudden coronary death in 1373 patients aged 40–60 years. The retrospective analysis period is 40 years. The data obtained in this study showed that systematic intake of long-chain ω-3 PUFAs statistically significantly (p < 0.05) reduced the risk of sudden coronary death (by an average of 54%). It was noted that with regular intake of ω-3 PUFAs, each increase in fatty fish intake by 20 g/day is statistically significant (p = 0.03) reduces the risk of death by 7%.
According to a meta-analysis [28], which analyzed the results of 13 randomized studies (average duration - 11.8 years), including 22,364 patients, systematic intake of ω-3 PUFAs statistically significantly (p < 0.05) reduces the risk of mortality in coronary heart disease. heart diseases.
The greatest antiarrhythmic effect in the treatment of ω-3 PUFAs should be expected in patients with coronary heart disease with ventricular arrhythmias without pronounced structural changes in the myocardium, with normal or moderately reduced left ventricular ejection fraction. Large randomized controlled trials have established the effectiveness of long-term therapy with ω-3 PUFAs at a dose of 1 g/day in the prevention of cardiovascular outcomes in patients with MI and heart failure, often associated with cardiac arrhythmias.
The working group of the European Society of Cardiology (ESC - European Society of Cardiology) to study the treatment of patients with acute myocardial infarction with ST segment elevation recommends additionally prescribing 1 g of ω-3 PUFAs derived from fish oil to the therapy (class of recommendations I, level of evidence B ) [29].
Benefits of fish oil for the brain
Fish oil acts as an antidepressant and stimulant for the brain. It affects the nervous system, ensuring the improvement of its structures, improves memory, attention and cognitive functions. Controls the emotional state, preventing the development of depressive disorders, relieving irritation, anxiety, and also providing other similar effects. The benefits of fish oil for the brain are provided by reducing the negative effects of alcoholic beverages and preventing cell damage. Drugs with this component help reduce the rate of spread of degenerative changes in Alzheimer's disease. They can also be used to correct behavioral factors. When used for children, fish oil helps cope with absent-mindedness, hyperactivity, and sleep disturbances.