Aortic regurgitation is mistakenly taken to be the name of the disease. Some are even trying to find an analogue in the ICD due to lesions of the aortic valves of various natures. Regurgitation is a physical phenomenon caused by the return of fluid flow. When applied to the aorta, it is the reverse flow of blood into the left ventricle. This is the meaning given to the term in functional diagnostics.
If previously experienced doctors could indicate this process only from a subjective point of view (as a result of auscultation and determination of the characteristic noise on the aorta), then with the introduction of ultrasound examination of the heart into practice, it became possible to see the movement of blood in the opposite direction. And the Doppler ultrasound method made it possible to assess the degree of return and connect this diagnostic sign to solving the problem of choosing a treatment method.
Prevalence
Patients with aortic regurgitation are recorded only in functional diagnostic rooms. Therefore, prevalence can be judged in relation to the number of Doppler-examined patients rather than in relation to the total population.
Various degrees and signs of reverse blood flow through the aortic opening are found in 8.5% of examined women and 13% of men. Among all heart defects in adults, chronic aortic regurgitation is detected in every tenth patient. Most often in old age in men.
Possible complications
Among the consequences of prolapse are:
- Heart failure. Occurs as a result of a significant decrease in myocardial contractility. Asystole requires urgent resuscitation measures.
- Heart attack. Necrosis of functionally active tissues. It always ends in ischemic disease of varying severity. The likelihood of fatal violations is minimal. In this case, first-degree prolapse progresses rapidly.
- Stroke. As a result, insufficient blood circulation in the cerebral structures.
- Vascular dementia. It is represented by a violation of normal trophism of the brain. The symptoms are similar to those of Alzheimer's disease. Recovery is potentially possible.
At the same time, the initial phases of the described heart defect practically do not cause complications. With a general prevalence of 1.5-3% of the number of cardiac pathologies, the risk of consequences is no more than 0.3-1% in general.
What anatomical structures are involved in the formation of regurgitation?
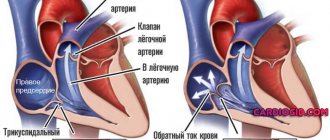
The structure of the four chambers of the heart ensures normal filling of the ventricles (blood flows from the atria) and active ejection into the aorta from the left ventricle, and into the pulmonary artery from the right. The valve system between the cavities and main vessels forms a natural barrier to the return flow.
View of an unclosed aortic opening when the heart is stopped, when valve replacement is required
The physiology of valves, their structure, and muscle bundles for tension react to blood pressure and obey nerve impulses that control the functions of the heart. Any violations of the structure and structure contribute to incomplete closure of the valves. The blood, having passed through the hole, is directed back.
The heart has 4 types of valves between:
- atria and ventricles on the left and right;
- left ventricle and aorta;
- right ventricle and pulmonary artery.
Accordingly, depending on the location of the lesion, mitral regurgitation, return through the tricuspid valve, and incompetence of the valves in the pulmonary artery are possible.
Aortic regurgitation seems to be a special case of dysfunction of the valve apparatus.
conclusions
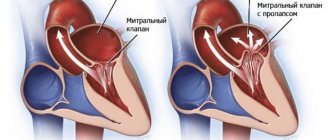
Regurgitation in the bicuspid valve occurs due to the inability of its leaflets to close tightly during systole. The danger of reverse blood flow is the expansion of the cavities of the heart and their excessive filling with blood. To support the pumping function, the myocardium hypertrophies compensatoryly. The heart muscle is not adapted for long-term stress of this degree, so decompensation occurs, expressed in characteristic clinical symptoms, the earliest of which is shortness of breath.
The gold standard for diagnosing regurgitation is Doppler ultrasound of the heart. Stages 3 and 4 of mitral regurgitation are subject to surgical treatment.
The mechanism of regurgitation in normal and pathological conditions
Cardiologists identify minor physiological regurgitation, which is possible under normal conditions. For example, 70% of tall adults have incomplete closure of the tricuspid valve, which the person is not aware of. Ultrasound reveals slight swirling flows when the valves are completely closed. This does not affect general blood circulation.
Pathology occurs during inflammatory processes:
- rheumatism,
- infective endocarditis.
Most typical for mitral localization, the formation of heart disease. It should not be confused with prolapse (stretching and bending of the valves into the atrium). It is with prolapse that physiological regurgitation often occurs and is found in growing children and adolescents. It is taken into account as a possible cause of extrasystole. The child must be observed by a cardiologist and re-examined. No special treatment is required.
The formation of scars after an acute heart attack, against the background of cardiosclerosis, in the area approaching the valve leaflets and threads, leads to breakdown of the necessary tension mechanism and changes the shape of the leaflets. Therefore, they do not completely close.
In a pathological process, an equally significant role is played by the diameter of the outlet, which must be blocked. Significant enlargement due to left ventricular dilatation or hypertrophy prevents the tight junction of the aortic valve leaflets.
Diagnostics of the process and detailing of complaints
The disease can only be diagnosed after the patient seeks help. Mitral valve regurgitation of the 1st degree (up to 5 ml) is not clinically manifested. Symptoms occur with more significant hemodynamic disturbances.
Long-term concealment of mitral insufficiency is ensured by thickening of the left ventricular myocardium. However, when the reserves of this mechanism are depleted, the patient’s condition sharply worsens.
There are 5 stages of mitral insufficiency.
| Stage | Complaints | Hemodynamic disorders | Treatment |
| Compensation | None | Clinically insignificant regurgitation, up to 1+ (no more than 5 ml) | Not required |
| Subcompensations | Shortness of breath when walking long distances or running | Regurgitation within 2+ (about 10 ml). Left heart: ventricular hypertrophy, atrial dilatation | Surgical treatment is not indicated |
| Right ventricular decompensation | Breathing problems with minor exercise | Significant regurgitation, 3+. Dilatation of the left ventricle, enlargement of the right sections. | Surgical treatments are recommended |
| Dystrophic | Shortness of breath without external causes, cough, swelling, fatigue | Deterioration of the pumping function of the heart, relative insufficiency of the tricuspid valve | Surgical treatment indicated |
| Terminal | The patient's condition is serious. Hemoptysis, cough, swelling, poorly healing ulcers. | Decompensation of the circulatory system | Treatment not indicated |
The army will not accept for military service a person with regurgitation of the second degree or higher!
Typical complaints with mitral insufficiency:
shortness of breath (initially with significant physical activity, in the terminal stages - on an ongoing basis);- palpitations (during physical activity);
- acrocyanosis (blue discoloration of fingertips);
- “mitral butterfly” (blue blush on the cheeks);
- cardialgia (pain in the heart of an aching or pressing, sometimes stabbing nature, not necessarily associated with stress);
- swelling in the legs (appears in the afternoon, in the evening, in the initial stages disappears overnight);
- pain in the right hypochondrium (appears as a result of blood stagnation, with pronounced swelling);
- cough (with stagnation of blood in the pulmonary circulation, often unproductive);
- hemoptysis (with decompensation of the patient’s condition).
Hemodynamic disorders can be diagnosed using the following instrumental methods:
- electrocardiography (left ventricular hypertrophy, arrhythmias, after the third stage - right ventricular hypertrophy);
- phonocardiography (the first tone is weakened, a systolic murmur is determined at the apex of the heart);
- echocardiography (enlargement of the heart cavities and thickening of the myocardium, changes in the movements of the interventricular septum, calcifications in the mitral valve leaflets);
- Doppler echocardiography (detection of the return of part of the blood to the atrium during ventricular systole).
Main valvular causes of aortic regurgitation
The causes of damage to the aortic valves, the diameter of the hole between the left ventricle and the initial part of the aorta, are:
- rheumatic inflammation localized along the line of valve closure - tissue infiltration at the initial stage leads to wrinkling of the valves, forming a hole in the center for the passage of blood during systole into the cavity of the left ventricle;
- bacterial sepsis with damage to the endocardium and aortic arch;
- warty and ulcerative endocarditis in severe forms of infection (typhoid fever, influenza, measles, scarlet fever), pneumonia, cancer intoxication (myxoma) - the valves are completely destroyed;
- congenital defects (formation of two leaflets instead of three) involving the aorta, large ventricular septal defect;
- specific autoimmune processes in the ascending aorta in chronic syphilis, ankylosing spondylitis, rheumatoid polyarthritis;
- hypertension, atherosclerosis - the process of compaction of the valves with the deposition of calcium salts, expansion of the ring due to dilatation of the aorta;
- consequences of myocardial infarction;
- cardiomyopathy;
- chest injuries with rupture of the muscles that contract the valves.
Bicuspid aortic valve is considered a type of congenital defect and increases the risk of regurgitation
The reasons include complications of treatment of heart diseases using catheter radiofrequency ablation, as well as cases of destruction of the biological valve prosthesis.
Mitral regurgitation
Mitral valve regurgitation
(mitral regurgitation, mitral valve regurgitation, mitral regurgitation (MR))
is the inability of the mitral valve to prevent blood from flowing back from the LV during its systole into the left atrium. The term “mitral regurgitation” refers specifically to the reverse flow of blood from the LV to the left atrium, i.e. a consequence of mitral regurgitation. Nevertheless, the terms have become practically synonymous.
Etiology
The mitral valve apparatus is represented by the mitral valve leaflets, chordae tendineae, papillary muscles and the fibrous annulus of the mitral valve. Pathology of any of these structures can lead to the development of MR. The most common causes of MR are:
- rheumatic fever (in such cases, MR is almost always combined with MC);
- mitral valve prolapse syndrome;
- cardiac ischemia;
Scheme
Functional classification of mitral regurgitation according to Carpentier. Classification of the range of motion of the mitral leaflet: type I – movement is not limited; type II – excessive mobility; type III – restriction of mobility
Clinic
During the compensation period, which can last several years, mitral regurgitation may be asymptomatic. In the subcompensation stage, subjective symptoms appear, expressed by shortness of breath, fatigue, tachycardia, anginal pain, cough, and hemoptysis. As venous stagnation in the pulmonary circulation increases, attacks of nocturnal cardiac asthma may occur. The development of right ventricular failure is accompanied by the manifestation of acrocyanosis, peripheral edema, liver enlargement, swelling of the neck veins, and ascites. When the recurrent laryngeal nerve is compressed by the dilated left atrium or pulmonary trunk, hoarseness or aphonia occurs (Ortner's syndrome). In the decompensation stage, more than half of patients with mitral insufficiency have atrial fibrillation.
Radiolic finds
Radiography
- Increased size of the left atrium.
- Increased size of the left ventricle.
- Signs of stagnation in the pulmonary circulation.
- Curley B lines
Ultrasound Echocardiography
To assess the degree of mitral regurgitation, there are a number of echocardiographic indicators. First of all, you should focus on such a parameter as the width of the vena contracta - the size of the convergent flow of regurgitation immediately under the leaflets. The vena contracta correlates with the diameter of the regurgitant orifice and therefore with the severity of the regurgitation. Mild regurgitation is characterized by a narrow vena contracta, the width of which is less than 3 mm; in severe MR, this parameter is 7 mm or more. More accurate indicators are obtained in the parasternal projection along the long axis of the heart. To optimize visualization of the vena contracta and increase measurement accuracy, it is preferable to use the magnification mode. Transverse section of the vena contracta is recognized as an effective regurgitant lumen and is also the recommended measurement method.
The method of assessing the proximal isovelocity surface or proximal regurgitant zone is a method of calculating the effective area of the regurgitant orifice, based on an assessment of the convergence zone of the regurgitant flow. If it is 1.0 cm or more, then MR should be considered severe. Having determined the radius of the proximal regurgitation zone at the beginning of diastole, the maximum speed of the regurgitation flow and knowing the speed at which the aliasing effect appears (the speed limit for the occurrence of the spectrum reversal phenomenon), we can calculate the effective area of the regurgitation orifice according to the formula EROA=6.28 R2 × integrated into the device Alias V / MR V. Effective regurgitation orifice area EROA 0.4 cm2 or more corresponds to severe MR, EROA no more than 0.2 cm2 indicates mild regurgitation.
Regurgitation flow area
determined by color Doppler ultrasound as the ratio of the area of the regurgitant flow to the area of the atrium with a Nyquist limit of 50–60 cm/s. The calculation of the regurgitation flow area index is obtained in a four- or two-chamber position in LV systole using a planimetric method of tracing the contours of the regurgitation flow using a correction factor (0.785) to the LA area. However, the use of this technique is limited by the possibility of error or incorrect interpretation of the data obtained. With atriomegaly, the severity of mitral regurgitation may be underestimated. If the jet is eccentric, it is impossible to assess its significance in one plane. Thus, this research technique allows one to obtain a rather rough idea of the volume of regurgitation, and is therefore considered to be uninformative and extremely dependent on signal amplification settings.
Scheme
Echocardiographic indicators for assessing the mitral valve during LV remodeling: a – normal; b – with LV remodeling, the angles of both MV leaflets increase; c – with further remodeling of the LV, the angle of the AMC (α2) can progressively increase, while the angle of the AMC (α1) decreases or the AMC – anterior mitral leaflet – does not change; PMS - posterior mitral leaflet
Echocardiography video
patient with mitral regurgitation.
Source
— Internal diseases — Volume 1 — textbook edited by Academician of the Russian Academy of Medical Sciences V.S. Moiseev, Academician of the Russian Academy of Medical Sciences A.I. Martynov, Academician of the Russian Academy of Medical Sciences N.A. Mukhina. - Radiopaedia.org - N.O. Sokolskaya, I.V. Slivneva ECHOCARDIOGRAPHIC CRITERIA FOR ASSESSING MITRAL INSUFFICIENCY OF ISCHEMIC GENESIS FSBI Scientific Center for Cardiovascular Surgery named after. A.N. Bakulev" (director - academician of the Russian Academy of Sciences and Russian Academy of Medical Sciences L.A. Bokeria).
Causes associated with aortic damage
The portion of the aortic arch closest to the heart is called the aortic root. It is its structure that influences the “health of the valves” and the width of the gate ring from the left ventricle. Root lesions include:
- age-related or degenerative changes causing dilatation;
- cystic necrosis of the middle layer of the aorta in Marfan syndrome;
- dissection of the aneurysm wall;
- inflammation (aortitis) with syphilis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis;
- giant cell arteritis;
- malignant hypertension.
Among the reasons, a negative effect of drugs used to reduce appetite in obesity was found.
Consequences of aortic regurgitation
The return of blood to the left ventricle inevitably leads to its expansion and increase in volume. Possible expansion of the mitral annulus and further enlargement of the left atrium.
At the point of contact of the blood flow, “pockets” are formed on the endocardium. The greater the degree of regurgitation, the faster the left ventricular overload develops.
Studies have shown the meaning of heart rate:
- bradycardia increases the volume of return flow and promotes decompensation;
- tachycardia reduces regurgitation and causes greater adaptation.
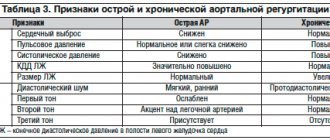
Forms of aortic regurgitation
It is customary to distinguish between acute and chronic aortic regurgitation.
Features of the acute form
Typical causes of acute aortic regurgitation are:
- injuries;
- dissecting aneurysm;
- infective endocarditis.
The volume of blood entering the left ventricle during diastole increases suddenly. Adaptation mechanisms do not have time to develop. The load on the left side of the heart and myocardial weakness increases sharply. Insufficient blood volume is released into the aorta to support general circulation.
Patients develop signs of pulmonary edema and cardiogenic shock. Symptoms are very severe when hypertension and aortic aneurysm dissection are combined.
Features of chronic aortic regurgitation
A distinctive feature of the chronic form is sufficient time for the full activation of compensatory mechanisms and adaptation of the left ventricle. This causes a period of compensation for circulatory disorders. Myocardial hypertrophy helps compensate for the reduced output.
When reserve energy reserves are depleted, a stage of decompensation occurs with severe heart failure.
3. Symptoms of the disease
Chronic mitral regurgitation is characterized by the absence of symptoms for many years. As a rule, patients do not know about heart disease for a long time, the symptoms of which appear gradually. The acute form of regurgitation is much more serious and is accompanied by the same symptoms as cardiogenic shock and acute heart failure.
We list the main symptoms of mitral valve regurgitation:
- constant shortness of breath;
- weakness and increased fatigue;
- dizziness;
- pain in the chest;
- confusion;
- swelling of the lower extremities.
If you notice at least two of the above symptoms, be sure to contact a good cardiologist. You may need immediate treatment.
About our clinic Chistye Prudy metro station Medintercom page!
Clinical manifestations
In the acute form of aortic regurgitation, the patient suddenly exhibits signs of cardiogenic shock:
- severe weakness;
- pale skin;
- severe hypotension;
- dyspnea.
For pulmonary edema:
- the patient is suffocating;
- breathing is noisy and hoarse;
- when coughing, foamy sputum mixed with blood is released;
- face, lips, limbs are cyanotic;
- heart sounds are sharply muffled;
- A lot of moist rales are heard in the lungs.
With chronic aortic regurgitation, a long asymptomatic period is possible. Symptoms appear only with the development of myocardial ischemia and severe cardiac decompensation. The patient notes:
- shortness of breath on exertion;
- strong heartbeats;
- extrasystoles;
- angina attacks at night;
- a “cardiac asthma” clinic is possible.
During the examination, the doctor notes:
- shaking the head in rhythm with the pulsation of the heart;
- a typical pulse on the radial artery is a sharp shock wave and an immediate fall;
- trembling when palpating the chest at the base of the heart;
- expansion of the left cardiac border;
- pulsating carotid arteries;
- diastolic murmur on the aorta, along the left edge of the sternum in the third and fourth intercostal spaces, is better heard in a sitting position with a slight bend forward, the first sound is clapping.
Diagnostic methods
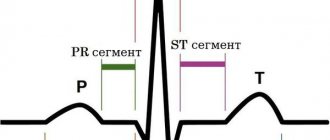
Indirect signs of aortic regurgitation are noted in:
- chest x-ray - the left contour of the cardiac shadow is expanded to the side and down, the expansion of the aortic arch is similar to an aneurysm, there are clear signs of enlargement of the left atrium, calcifications may be detected in the aortic arch;
- electrocardiogram - overload of the left chambers of the heart is revealed.
Deviation of the electrical axis to the left, a characteristic change in the shape of the ventricular complexes in leads I, AVL, V3-V6, negative T waves
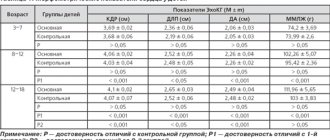
Echocardiographic method
In the diagnosis of regurgitation, echocardiography serves as the main objective method; it allows one to determine the cause, the degree of regurgitation, the sufficiency of compensatory reserves, and circulatory disorders even in the asymptomatic stage of the disease with minimal disturbances. It is recommended for patients in the initial stage annually, and twice a year when clinical symptoms appear.
The calculations take into account the surface area of the patient's body, due to the lack of pronounced expansion of the ventricular chamber in short people.
The most commonly used mode is color Doppler scanning. The sensors are installed in such a way as to measure the area of blood flow at the aortic valves, in the initial part of the aorta, and compare it with the width of the passage. In severe cases, it exceeds 60% of the ring diameter.
The device allows you to record the time interval of the wave and establish the expansion of the left ventricle
In the practice of cardiologists, a division of the return jet into 4 degrees is used in relation to its length to the size and internal formations of the left ventricle:
- 1 - does not extend beyond half the length of the anterior leaflet at the mitral valve;
- 2 - reaches or crosses the gate;
- 3 - the flow value approaches half the length of the ventricle;
- 4 - the jet touches the top.
The definition of regurgitation depends on the area (width) of the jet, its location, the level of loss of blood ejection from the left ventricle, and the volume per contraction. Based on quantitative indicators, they are conventionally divided into mild, moderate and severe forms.
If information from Doppler sonography is not enough, the following is carried out:
- magnetic resonance imaging;
- radionuclide angiography;
- cardiac catheterization.
4. Diagnosis and treatment of mitral valve regurgitation
Diagnosis of mitral valve regurgitation may include:
- medical examination;
- echocardiogram - a procedure based on the use of sound waves to determine the shape, size and structure of heart tissue;
- chest x-ray;
- electrocardiogram of the heart, which allows to detect irregularities in the heart rhythm;
- cardiac catheterization - examination of the cavities of the heart, as well as nearby blood vessels, using a hollow flexible tube.
These tests not only detect mitral regurgitation, but also determine the degree of mitral regurgitation. The information obtained during the study is the basis on which further treatment is based.
The choice of treatment for mitral valve regurgitation depends primarily on the form of the disease, as well as the degree of its progression.
For example, in chronic cases, doctors most often prescribe constant monitoring of the patient’s heart condition and the use of special medications to eliminate the symptoms of the disease. These drugs include:
- vasodilators – a group of vasodilating drugs;
- diuretics and diuretics;
- anticoagulants - drugs that prevent the formation of blood clots.
If necessary, your doctor may recommend surgery to repair or replace the mitral valve. Patients with mitral regurgitation need to radically change their lifestyle in order to reduce the load on the heart. Doctors recommend avoiding intense physical activity and emotional stress, leading a healthy lifestyle and eating right.
Who is indicated for surgical treatment?
The only form of surgery is aortic valve replacement. The operation is indicated for:
- severe form of regurgitation with impaired left ventricular function;
- if the course is asymptomatic, with preserved ventricular function, but pronounced expansion (dilatation).
Aortic valve replacement surgery is often combined with coronary artery bypass grafting.
Causes
Development factors are always pathological. Conventionally, they can be divided into two groups: congenital and acquired.
The moments that determine the existence of MVP from the first days are characterized by a genetic defect or a spontaneous disorder in the development of the cardiovascular system during the perinatal period.
The first stage of congenital prolapse is an isolated process extremely rarely. Mild MV prolapse occurs in parallel with developmental disorders of the aortic valve, interatrial septum, cardiopathy and other diseases.
In addition to problems with the muscular organ, disorders occur in the maxillofacial region and other anatomical structures.
Acquired defects are detected many times more often. They are not associated with genetic syndromes.
This is all due to negative internal and external factors: smoking, alcohol consumption, unfavorable environmental conditions, background radiation, taking medications, severe pregnancy and other factors.
There are many reasons:
- Insufficient elasticity of connective tissue. The incorrect structure is laid down in the prenatal period. The occurrence of autoimmune pathological processes is possible: systemic lupus erythematosus, collagenosis. All these factors lead to weakening and thinning of the valve structure. MV regurgitation and prolapse occur. It must be said that the disease does not stay at stage 1 for long. Progression rapidly leads to heart failure.
- Problems with local and general metabolism. The metabolic factor causes poor nutrition of the anatomical structure. The result is a decrease in elasticity and connective tissue degeneration. The result is a decrease in resistance. Even with normal pressure inside the left ventricle, there is excessive force on the mitral valve. It can’t stand it, opens up, allows blood to flow in the opposite direction, and regurgitation occurs.
- Arterial hypertension. Increase in pressure. It is not always associated with vascular problems. But more often than not it is. A stable increase in tonometer readings leads to a rapid disruption of the functional activity of the heart. The left ventricle grows and dilates. Overload occurs. The mechanical effect also increases on the mitral valve. At a certain moment, it cannot stand it, opens up, and allows liquid connective tissue to pass in the opposite direction. Correcting blood pressure does not provide full recovery. Requires surgery. Treatment is carried out in two directions at once: normalization of blood pressure and prosthetics of the anatomical structure.
- Cardiac ischemia. Has several etiological factors. The main one is coronary insufficiency. Develops as a result of atherosclerosis of the arteries. Such a complex chain-type scheme leads to difficulties in early diagnosis. The muscle layer does not receive enough nutrients and oxygen. Hence the dystrophy of the mitral valve. Recovery is carried out surgically. But there is no point in stopping the investigation. It is necessary to eliminate coronary insufficiency and restore myocardial contractility.
- Myocarditis. Inflammation of the muscle layer of the organ. It appears to be an infectious disease in almost 80% of cases. However, it is extremely rarely primary. Usually we are talking about a complication of a previous cold or acute respiratory viral infection. In the remaining 20% of situations, they talk about an autoimmune process. It turns out to be the result of rheumatism. Treatment is urgent, in a hospital setting. Loading doses of antibiotics are used, and it is possible to prescribe immunosuppressants that inhibit pathological reactions of the body.
- Previously suffered sore throat. Sore throat. Also called tonsillitis. Processes of this kind are progressing rapidly. It is urgent to transfer the disease into the latent phase and keep it in this state constantly.
- Pericarditis. Inflammation of the pericardial sac. It keeps the muscle organ in one position and does not allow it to move at the moment of full contraction. The danger lies not so much in the pathological process itself as in its complications. For example, tamponade. That is, compression of cardiac structures by effusion or blood (much less often). It can all end in sudden cardiac arrest.
- Other malformations of the muscular organ. Various conditions are affected. The connection is not always obvious at first glance. The operation becomes the only chance to restore normal activity of the organ and stabilize hemodynamics.
- Previous heart attack. Acute tissue death of the muscle layer. Necrosis leads to gross scarring (the phenomenon is called post-infarction cardiosclerosis). The elasticity of the heart decreases, while the volume of blood filling remains the same, the pressure in the chambers increases. Accordingly, the load on the mitral valve is significantly higher than usual. The organ cannot work like this for a long period.
The exact reasons, however, are not fully known. Doctors point to the important role of so-called connective tissue dysplasia. This is a congenital disorder of the formation of muscle structures, ligaments, including the myocardium and valves (aortic, mitral).
The pathological process is accompanied by a group of deviations. Not only prolapse, but also other things. Curvature of the spine occurs due to weakness of the muscular corset of the back, arthritis due to improper load distribution, and myopia.
Forecast
The prognosis for the patient’s life depends on the underlying disease, the degree of regurgitation, and the form. An early mortality rate is typical for the acute development of pathology. In the chronic form, 75% of patients live more than 5 years, and half live 10 years or longer.
In the absence of timely surgical intervention, the development of heart failure is noted in the next 2 years.
Treatment of moderate clinical symptoms is accompanied by positive results in 90% of patients. This reinforces the importance of evaluating and monitoring patients with aortic regurgitation.
Classification
Diagnosed cases of the disease in adolescents and adults are divided into two types:
- MVP with a high risk of developing regurgitation;
- moderate prolapse with a low risk of developing minor regurgitation.
Doctors can also divide the disease into stages:
- moderate prolapse 0-1 degree: also known as primary (even during pregnancy, no negative symptoms are felt; the body independently regulates the additional load on the heart);
- MVP stage 2 (transitional): signs - intracardiac pressure increases, in adolescents and during pregnancy there is constant shortness of breath and fatigue;
- 3rd (decompensated stage): significant damage to the heart muscle can be diagnosed.